Redo-TAV For Bicuspid vs. Tricuspid Aortic Valves
Simulations using post-TAVR CT imaging show that redo-TAV is more feasible in patients with bicuspid aortic valves compared to tricuspid aortic valves, according to new research published in JACC: Cardiovascular Interventions.
Atsushi Okada, MD, et al., conducted CT simulations of redo-TAV using 913 electrocardiographically gated contrast-enhanced cardiac CT imaging cases taken 30 days post TAVR. Of participants, 623 underwent TAVR with a SAPIEN 3 or SAPIEN 3 Ultra valve, while 290 had an Evolut R, PRO or PRO+ valve. The 59 patients with bicuspid valve morphology (92% type 1, 8% type 0) tended to be younger than the 85 patients with tricuspid valve morphology (median age 77 years vs. 82 years) and were treated more frequently with a SAPIEN valve (81% of cases vs. 67% of tricuspid cases).
For each case, investigators simulated four redo-TAV scenarios: S3-in-S3, Evolut-in-S3, S30-in-Evolut and Evolut-in-Evolut. The primary endpoint of feasibility was defined as risk to coronary arteries. Patients were categorized as low risk if 1) their neoskirt plane (NSP) was below their coronary risk plane (CRP; the lowest edge of the lowest coronary ostium); 2) their NSP was above CRP, but valve-to-aortic sinus (VTAoS) and valve-to-coronary artery (VTC) distances were adequate (>4 mm); 3) or their NSP was above CRP, both were above sinotubular junction, and VTAoS, VTC and valve-to-sinotubular junction distances were adequate (>4 mm).
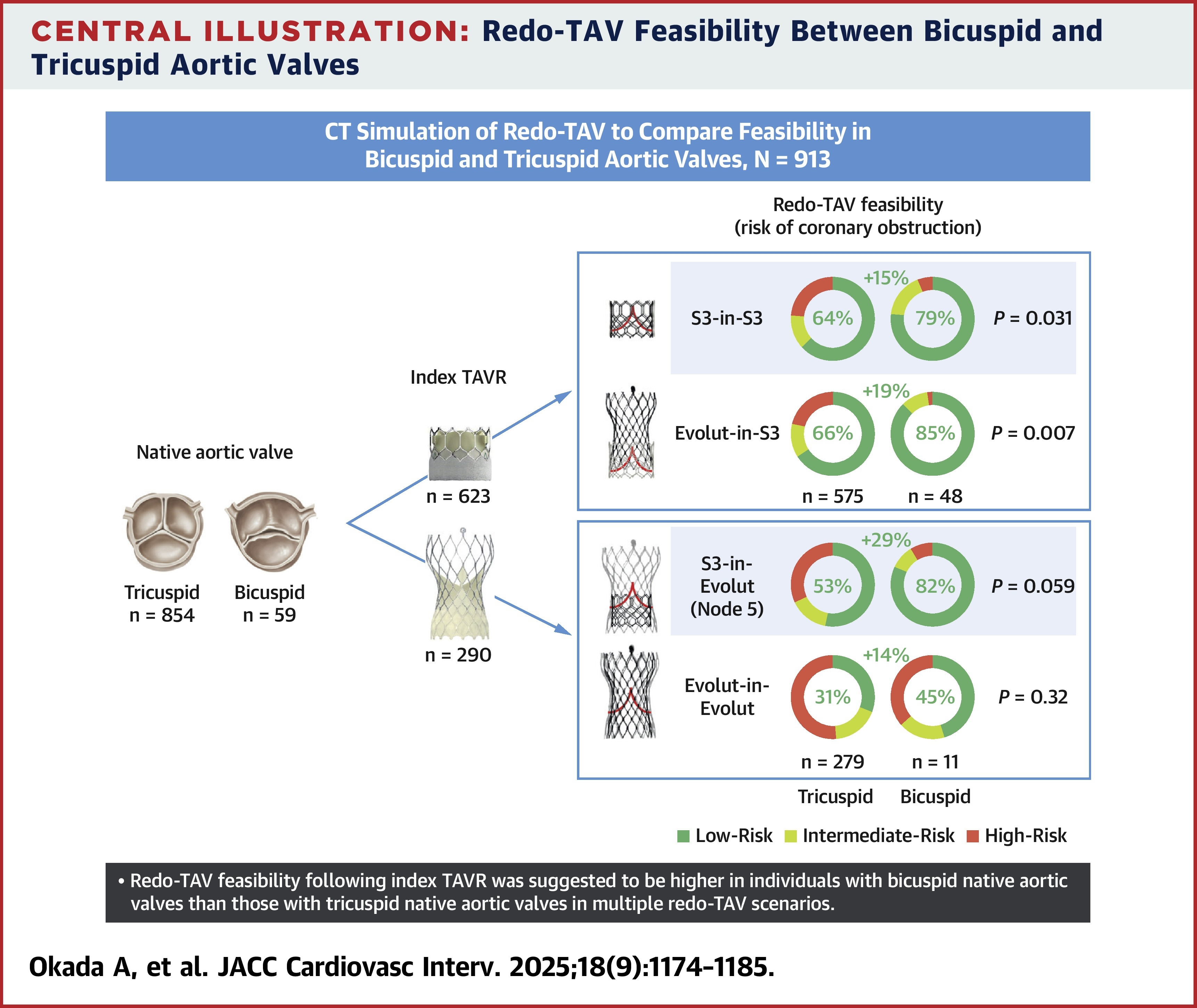
Results showed that patients with bicuspid valves had significantly higher redo-TAV feasibility in S3-in-S3 (79% considered low risk vs. 64% of cases with tricuspid valves), and Evolut-in-S3 (85% vs. 66%) scenarios. Although not statistically significant, similar trends were seen in the S3-in-Evolut (82% considered low-risk vs. 53%) and Evolut-in-Evolut (45% vs. 31%) scenarios, and feasibility tended to be higher for bicuspid cases.
Patients with bicuspid valves had larger aortic root anatomy: larger annular areas (522 mm2 vs. 479 mm2), sinus of Valsalva diameters (34 mm vs. 32 mm) and sinotubular junction diameters (30 mm vs. 29 mm). They also tended to have longer narrowest valve-to-aorta distances.
During the follow-up period, four patients underwent redo-TAV; the risk estimation based on the simulation matched the actual risk estimation in all four cases.
Okada, et al., write that their research could prompt, "further research into optimizing long-term treatment strategies in patients with bicuspid valves, including the selection of the index valve type." They add that, "This also may lead to advances in TAVR techniques, including leaflet modification, which may mitigate the risk for coronary obstruction during redo-TAV, or other technologies specifically tailored to this patient population."
In an accompanying editorial comment, Stephan Windecker, MD, and Daijiro Tomii, MD, write that the study "helps to clarify uncertainties" in an era that is seeing an increase in repeat interventions following TAVR in low-risk patients. However, they note that 30-day CT findings may not be applicable when typical aortic valve reintervention occurs more than a decade post index procedure. "Until comprehensive long-term data become available, heart teams must adopt an individualized approach," the authors write, "tailoring treatment strategies based on patient-specific anatomical factors, risk profiles, and anticipated need for future interventions."
Clinical Topics: Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Invasive Cardiovascular Angiography and Intervention, Valvular Heart Disease, Aortic Surgery, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Interventions, Interventions and Structural Heart Disease
Keywords: Mitral Valve, Tricuspid Valve, Bicuspid Aortic Valve Disease, Transcatheter Aortic Valve Replacement, Aorta, Thoracic, Coronary Vessels, Sinus of Valsalva
< Back to Listings
