ACC Member Experience: Highlights From the 24th ASNC Scientific Meeting
This year's Annual American Society of Nuclear Cardiology (ASNC) Scientific meeting in Chicago presented innovative science in the field of nuclear cardiology. The meeting was coordinated by the Panithaya Chareonthaitawee, MD, FACC, and co-chaired by Terrence D. Ruddy, MD, FACC.
Twelve program tracks were available, with highlights including the advanced track, "Cases with the Aces" interactive reading track, inaugural scintillating learning through social media track, and plenary track.
In order to distill this information-rich conference, I have provided my "top 10 sessions," each with at least one take home point highlighting the science of imaging.
The meeting started with an opening keynote talk delivered by Clyde W. Yancy, MD, MACC, and titled, "Addressing Cardiovascular Disease Disparities-Are We Getting Closer to the Truth?"
The take home points of this talk included four suggestions for health care providers to decrease implicit bias, including listening to your patients; pausing and checking your assumptions; recruiting other ideas and a diverse workforce; and taking an implicit association test to make yourself aware of your own biases.
The importance of social media for imagers and national meetings continues to grow. ASNC's social media track chairs, Niti R. Aggarwal, MD, FACC, and Renee P. Bullock-Palmer, MBBS, FACC, encouraged the use of Twitter as an online platform to share science.
With 20 ASNC social media ambassadors designated, 2019 social media engagement soared to over nine million digital impressions on Twitter.
The top three tweets during the meeting focused on:
- The recently released ASNC multi-society document on cardiac amyloidosis.
- Debates in Cardiac PET: Clash of the Photons – First Test for Suspected Cardiac Sarcoidosis: FDG-PET vs. CMR.
- The Social Media (#SoMe) Session with the Giants: Controversies With Lifestyle Medicine & Preventive Cardiology. Kim A. Williams Sr., MD, MACC, and Regina S. Druz, MD, FACC, debated the Mediterranean vs. vegan diets with regards to cardiovascular outcomes.
The role of hybrid imaging techniques continues to evolve. The Mario Verani lecture, given by John J. Mahmarian, MD, FACC, was titled, "A Tale of Two Imaging Technologies: Can Nuclear Cardiology Survive the Emergence of Cardiac CT?" His talk outlined the novel and emerging applications of nuclear cardiac imaging and the utility of hybrid imaging with myocardial perfusion (SPECT or PET) and coronary artery calcium (CAC) score.
Three take home points included:
- The future of nuclear cardiology is bright, particularly with SPECT/PET-CT, as myocardial perfusion imaging (MPI) remains a first line test in patients with known coronary artery disease (CAD) and selective MPI remains useful in asymptomatic patients with coronary artery calcium score (CACS) >100.
- Integration of CACS in symptomatic patients with normal MPI is useful to enhance assessment of lifetime cardiovascular risk.
- Hot spot imaging is a unique aspect of nuclear imaging to diagnose infections of left ventricular assist devices (LVADs), prosthetic heart valves and other cardiac hardware.
Nuclear imaging plays a pivotal role in diagnosis of cardiac amyloidosis. A plenary session dedicated to cardiac amyloid imaging focused on the approved treatments of transthyretin type cardiac amyloidosis and the utility of bone scintigraphy for diagnosis, with discussion about the recently published ASNC/Multi-society Consensus Recommendations.
Cardiac amyloidosis remains a very exciting area of research as novel data continue to emerge with regards to this disease.
Important take home points included:
- For asymptomatic ATTR familial gene carriers, a physical exam, nTpro-BNP level, troponin level, echocardiogram, ECG, and Tc-99m-Pyrophosphate scan (+/- CMR) at baseline and then every 1-2 years is recommended.
- Beware of false positives on radionuclide scintigraphy, such as monoclonal gammopathy, hydroxychloroquine toxicity, rib fractures, pleural effusions, blood pool uptake, breast implants and recent myocardial infarction (4 or less weeks). For patients with AL amyloidosis, it is recommended to perform free light chain analysis for all cases. SPECT ± CT improves specificity to address most of the issues with non-myocardial uptake.
- Beware of false negatives on radionuclide scintigraphy, such as in patients with full length (type B) transthyretin (TTR) fibrils as in Phe64Leu and occasionally in Val30Met genotypes. False negatives may also be seen in early disease.
- Endomyocardial biopsy (EMB) should be considered if bone marrow biopsy is negative and clinical suspicion persists. EMB should also be considered if pyrophosphate (PYP) scan is positive and free light chains are elevated or in the presence of monoclonal gammopathy. It should also be considered if PYP is equivocal or negative and clinical suspicion persists.
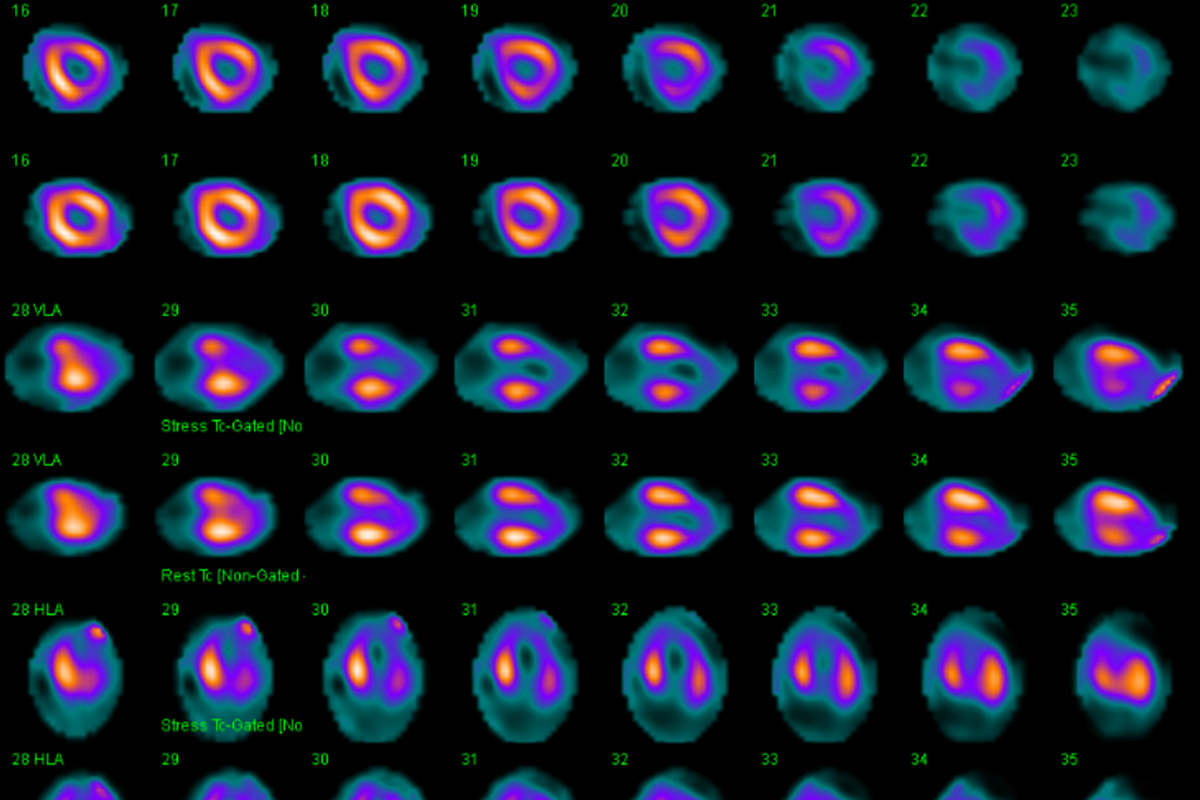
Debates on a national stage can often provide unique perspectives on controversial topics. In a session titled, "Clash of the Photons: Debates in Cardiac PET," there was an exciting debate on PET vs. SPECT for MPI. Venkatesh L. Murthy, MD, PhD, FACC, debated pro PET and outlined the advantages of cardiac PET which included faster protocols, lower radiation dosimetry, greater defect sensitivity, fewer artifacts, the ability to perform blood flow quantification, and the ability to assess myocardial viability and inflammation.
This was outlined in his recent paper published in September. Terrence D. Ruddy, MD, FACC, debated pro SPECT, where he outlined the fact that SPECT remains the "work-horse" for many nuclear labs with more than 4,000 patient studies per year, including MPI, radionuclide angiography, pyrophosphate scans for ATTR cardiac amyloid and MIBG imaging.
His final point was that SPECT is useful for most patients, but PET is useful for some patients such as obese patients, patients with complex CAD, and is useful in the assessment of viability and inflammation.
Tailoring imaging to the individual patient remains paramount as nuclear medicine imaging science continues to evolve. In the session on evaluation of ischemia in special populations, science was presented on targeted imaging in unique chest pain populations such as women, elderly patients and morbidly obese patients.
Unique take home points for women presenting with ischemia with non-obstructive coronary arteries (INOCA) undergoing PET imaging presented by Nils Johnson, MD, were:
- Pay attention to regional reduction in coronary flow reserve (CFR), not just global CFR.
- Hold caffeine for 24 hours to avoid falsely low CFR (5 percent of patients have elevated caffeine levels at the time of the scan).
- Look for subendocardial defects.
Sessions on novel SPECT applications included discussion of the novel application of assessing myocardial blood flow with SPECT. Reasons given for the increasing promise in this area included the fact that PET tracers are limited worldwide and the availability of SPECT more commonly in offices in and outside of the U.S. Myocardial blood flow assessment is useful to determine if the myocardial perfusion study is truly normal, to rule out non-response to vasodilator agent and to assess multi-vessel disease, balanced flow reduction, microvascular disease and endothelial dysfunction.
On the cutting edge of nuclear imaging, there were discussions of novel radiotracers in the pipeline such as Flurpiridaz, and PET based amyloid tracers such as Florbetapir and NaF. One potential clinical benefit highlighted for Florbetapir is the fact that this PET agent images direct amyloid binding and could potentially be useful in determining therapeutic response in patients with ATTR or AL type cardiac amyloidosis.
From a practical standpoint, ASNC 2019 provided guidance on optimization of SPECT imaging protocols. One such session, titled "Optimizing the Nuclear Lab to Exceed Your Ex-SPECT-ations," offered ways to enhance SPECT imaging protocols to improve lab throughput and minimize radiation exposure.
A practical take home point from this session was that Stress First (SF) and Stress Only (SO) imaging for myocardial perfusion SPECT is underutilized and that up to half of patients undergoing SF imaging may not require additional testing and are able to achieve a low radiation dose exposure of 2.9 mSv.
SO imaging may also obviate the need for additional isotope administration achieving at least a 30 percent isotope dose reduction compared to patients undergoing conventional rest/stress imaging.
Rounding out my "top 10," ASNC encouraged participation of Fellows in Training (FITs) and early career members as was seen at the "Choosing Wisely Challenge," which allowed these members to present their research and initiatives focused on delivering the best care for patients through appropriate and accurate cardiac imaging.
The top three presentations were:
- First place: Sudip K. Saha, MD, FACC, "Use of a Multi-Pronged Approach to Optimize Nuclear Cardiology Testing and Improve Safety."
- Second place: Benita Philip, DO, "Development of a Patient Centered, Cost Effective Algorithm Utilizing 99m-Technetium-Pyrophosphate Imaging to Diagnose ATTR Cardiac Amyloidosis."
- Third place: Anirudh Kumar, MD, "Impact of a Novel Myocardial Perfusion Imaging Risk Classification Scheme on Referral for Coronary Angiography, Revascularization and Mortality."
The 24th Annual ASNC meeting was educational, engaging and enlightening. Even narrowing things down to a "Top 10" list was challenging, given the sheer amount of novel applications and innovative technology presented in nuclear cardiology.
It was encouraging to see many established ASNC leaders engage with attendees both in person and virtually on social media. Talented FITs and early career faculty continued to demonstrate that the future of nuclear cardiology looks very bright.