Practical Considerations For ICD in Athletes
Quick Takes
- Implantable cardioverter-defibrillators (ICDs) are efficacious at aborting ventricular arrhythmias in athletes who carry a risk of sudden cardiac death.
- Athletes and practitioners must bear in mind the risks associated with participation in sports with an ICD.
- Shared-decision making is an effective discussion model for "return-to-play" in athletes with ICDs.
Background
Athletes who have a substrate for ventricular arrythmia (VA) may experience sudden cardiac death (SCD) as a first-time manifestation of their underlying disease. Some of the most common disorders that predispose young, healthy individuals to VA include hypertrophic cardiomyopathy (HCM), long QT syndrome (LQTS), Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia (CPVT), and arrhythmogenic right ventricular cardiomyopathy (ARVC). Providers may recommend beta-blocker medication alone or in combination with an implantable cardioverter-defibrillator (ICD) for primary or secondary prevention of VA in patients that are deemed high-risk individuals. Prior guidelines directed providers to apply a blanket recommendation against most sports participation besides Class 1A (e.g., billiards, bowling, cricket, curling, golf and riflery) for individuals that harbor conditions that predispose them to VA.1 Such strict recommendations have recently been met with opposition as a loss of autonomy in compromised patients' quality of life and mental health. The American Heart Association (AHA)/American College of Cardiology (ACC) scientific statement in 2015 has begun to adapt to these concerns and liberalized the guidelines to allow athletes with ICDs participation in higher intensity sports than Class IA, at the discretion of an expert provider. Additionally, there was the recommendation to have a discussion with their provider regarding the risk of inappropriate shocks and device-related trauma in high-impact sports.2 These discussions largely entail the practical considerations of having an ICD, and they may be best held with athletes according to a shared decision-making model (SDM).3
Risk Factors with Sports Participation and Device Programming
The incidence of SCD in athletes is approximately 1-2 out of 100,000 athletes per year.4 Adrenergic stimulation during exercise may increase the frequency of VA in individuals with an inherited arrhythmia diagnosis (channelopathy) and in those with pathological myocardial substrates (structural heart disease).5 Though ICDs do not decrease the risk of SCD, they have been shown to successfully abort arrhythmias and are equally efficacious in patients who participate in recreational sports as well as in competitive athletes.6
An analysis of the ICD Sports Safety registry identified a higher proportion of study participants receiving appropriate shock delivery during physical activity in comparison to during rest (8% vs. 3%). In the same study, 40 out of 77 (11%) participants were found to have experienced at least one inappropriate shock.7 Exercise can increase the propensity of inappropriate shocks by one of two mechanisms: 1) sinus tachycardia rates can compete with therapy zones and trigger inappropriate therapy and/or 2) T wave changes during exercise can lead to "double-counting" of sinus tachycardia leading to inappropriate therapy. Both issues can be avoided with age and disease-specific device programming and sophisticated sensing algorithms. The Primary Prevention Parameters Evaluation (PREPARE), Avoid Delivering Therapies for Nonsustained Arrhythmias in ICD Patients III (ADVANCE III) and the Multicenter Automatic Defibrillator Implantation Trial–Reduce Inappropriate Therapy (MADIT-RIT) trials showed that patients who had an ICD for primary prevention and had their devices programmed to detect arrhythmias at higher rates (≥200) and over longer intervals experienced a lower number of inappropriate shocks.8-10 To ensure robust yet safe programming of the device, an exercise stress test helps identify the maximal sinus rate that an individual may approach during exercise and our institutional practice has been to set the device therapy threshold at least 20 beats above their maximal sinus rate.
Damage to the ICD System
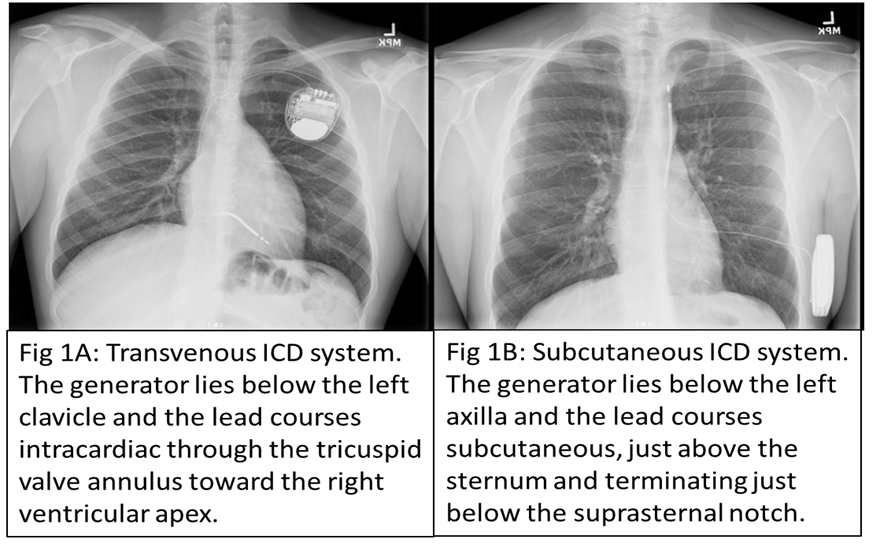
Another practical consideration with an ICD device is the risk of damage during contact sports and device malfunction with lead failure. Transvenous-ICD (TV-ICD; Figure 1A) has a greater likelihood of sustaining subclavian crush injuries. Football and hockey are examples of common contact sports in which there is an increased risk of device damage from collision injuries.11-12 Activities like golf and weightlifting consist of repetitive arm motion with increased pressure applied on the device which may also cause device damage.13 Additionally, patients should also be counseled about the possibility of device-related complications, such as endovascular infections with TV-ICD and pacemaker pocket infections and hematomas with subcutaneous-ICD (S-ICD; Figure 1B). The ICD Sports Safety Registry determined lead survival, free of malfunction to be 93% at 5 years.11 The S-ICD is relatively a more recent innovation in comparison to TV-ICD and has been proven to be a non-inferior device in terms of efficacy.14 The major advantages of S-ICD are avoidance of intracardiac hardware, eliminating the risk of endocarditis and the relative ease and safety of lead extraction.15 The S-ICD use is limited in athletes who require pacing for bradycardia and anti-tachycardia pacing.16 Overall, the rate of total complications with both TV-ICD and S-ICD are similar; however, prospective data over a greater follow-up period are required to study long-term outcomes.17
Figure 1
Shared Decision-Making Model
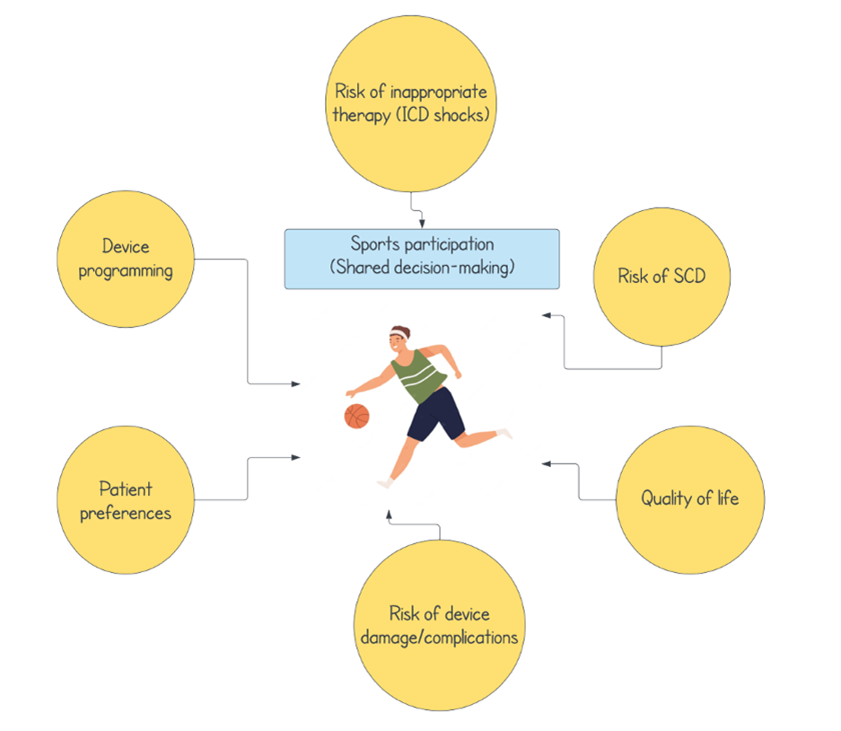
The objective of a discussion based on SDM is to provide the patient with all the information (risks and benefits) regarding sports participation and subsequently discuss their views and priorities in terms of health risk management to determine the safest and best way forward (Figure 2).18 It has become an increasingly popular method of developing a joint care plan (provider- and patient-decided) as it conserves patient autonomy within their health safety margin.
A conversation based on the SDM model is mechanically very different when patients are <18 years of age. In such circumstances, the driving principle behind the discussion is to arrive at a shared consensus with all parties involved including patients, physicians, and parents. Our practice is to provide the relevant pros/cons of that decision and guide the family and pediatric patient to arrive at a decision that is aligned to their values. Fortunately, with appropriate guidance, arriving at a consensus decision is invariably achievable.
Additionally, the discussions should be patient and disease specific since each disease substrate carries a specific risk profile as it pertains to the ICD. For example, in patients with CPVT, ICD therapy may cause additional catecholamine release leading to VT storm. Though the concept of device implantation as a "safety mechanism" to thwart the risk of sports participation might be proposed, several consensus statements warn against the placement of an ICD solely to facilitate sports participation (class III indication).19
Conclusion
Athletes equipped with ICDs and their providers are encouraged to have SDM discussions related to the practical implications of sports participation. It is important to discuss guidelines regarding sports participation recommendations, as well as the risk of device-related complications, inappropriate therapy, and the risk of SCD as it relates to sports participation. At the same time, it is essential to preserve their quality of life and sense of autonomy through the SDM paradigm.
Figure 2
References
- Maron BJ, Zipes DP. Introduction: eligibility recommendations for competitive athletes with cardiovascular abnormalities-general considerations. J Am Coll Cardiol 2005;45:1318-21.
- Maron BJ, Zipes DP, Kovacs RJ. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: preamble, principles, and general considerations: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2343-49.
- Baggish AL, Ackerman MJ, Putukian M, Lampert R. Shared decision making for athletes with cardiovascular disease: practical considerations. Curr Sports Med Rep 2019;18:76–81.
- Mont L, Pelliccia A, Sharma S, et al. Pre-participation cardiovascular evaluation for athletic participants to prevent sudden death: position paper from the EHRA and the EACPR, branches of the ESC. Endorsed by APHRS, HRS, and SOLAECE. Eur J Prev Cardiol 2017;24:41-69.
- Priori SG, Napolitano C, Memmi M, et al. Clinical and molecular characterization of patients with catecholaminergic polymorphic ventricular tachycardia. Circulation 2002;106:69-74.
- Heidbuchel H, Arbelo E, D'Ascenzi F, et al. Recommendations for participation in leisure-time physical activity and competitive sports of patients with arrhythmias and potentially arrhythmogenic conditions. Part 2: ventricular arrhythmias, channelopathies, and implantable defibrillators: a position statement of the Section of Sports Cardiology and Exercise from the European Association of Preventive Cardiology (EAPC) and the European Heart Rhythm Association (EHRA), both associations of the European Society of Cardiology EP Europace 2021;23:147-48.
- Lampert R, Olshansky B, Heidbuchel H, et al. Safety of sports for athletes with implantable cardioverter-defibrillators: results of a prospective, multinational registry. Circulation 2013;127:2021-30.
- Wilkoff BL, Williamson BD, Stern RS, et al. Strategic programming of detection and therapy parameters in implantable cardioverter-defibrillators reduces shocks in primary prevention patients: results from the PREPARE (Primary Prevention Parameters Evaluation) study. J Am Coll Cardiol 2008;52:541-50.
- Moss AJ, Schuger C, Beck CA, et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med 2012;367:2275-83.
- Kloppe A, Proclemer A, Arenal A, et al. Efficacy of long detection interval implantable cardioverter-defibrillator settings in secondary prevention population: data from the Avoid Delivering Therapies for Nonsustained Arrhythmias in ICD Patients III (ADVANCE III) trial. Circulation 2014;130:308-14.
- Rizal A, Ruspiono E, Putri DH. Intermittent pacemaker malfunction caused by continuous compression of the lead by the clavicle (subclavian crush syndrome). Eur J Case Rep Intern Med 2020;7:001684.
- Lampert R. Sport Participation in Patients with Implantable Cardioverter-Defibrillators. Curr Treat Options Cardiovasc Med 2019;21;66.
- Lampert R, Olshansky B. Sports participation in patients with implantable cardioverter-defibrillators. Herzschrittmacherther Elektrophysiol 2012;23:87-93.
- Chue CD, Kwok CS, Wong CW, et al. Efficacy and safety of the subcutaneous implantable cardioverter defibrillator: a systematic review. Heart 2017;103:1315–22.
- Bardy GH, Smith WM, Hood MA, et al. An entirely subcutaneous implantable cardioverter–defibrillator. N Engl J Med 2010;363:36-44.
- Viani S, Migliore F, Tola G, et al. Use and outcomes of subcutaneous implantable cardioverter-defibrillator (ICD) after transvenous ICD extraction: An analysis of current clinical practice and a comparison with transvenous ICD reimplantation. Heart Rhythm 2019;16:564–71.
- Su L, Guo J, Hao Y, Tan H. Comparing the safety of subcutaneous versus transvenous ICDs: a meta-analysis. J Interv Card Electrophysiol 2021;60:355-63.
- Hammond BH, Aziz PF, Phelan D. Importance of shared decision making for return to play after COVID-19. Circulation 2021;143:1733-34.
- Silka MH, Shah MJ, Avari Silva JN, et al. 2021 PACES expert consensus statement on the indications and management of cardiovascular implantable electronic devices in pediatric patients. Heart Rhythm 2021;18:1888-1924.
Clinical Topics: Arrhythmias and Clinical EP, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Sports and Exercise Cardiology, Implantable Devices, Genetic Arrhythmic Conditions, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Exercise, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology, Sports and Exercise and ECG and Stress Testing
Keywords: Sports, Athletes, Defibrillators, Implantable, Quality of Life, Gryllidae, Prospective Studies, Secondary Prevention, Tachycardia, Ventricular, American Heart Association, Arrhythmogenic Right Ventricular Dysplasia, Bradycardia, Brugada Syndrome, Channelopathies, Exercise Test, Follow-Up Studies, Institutional Practice, Mental Health, Tachycardia, Sinus, Death, Sudden, Cardiac, Exercise, Risk Factors, Risk Assessment, Registries, Cardiomyopathy, Hypertrophic, Primary Prevention, Long QT Syndrome, Risk Management, Catecholamines, Crush Injuries, Endocarditis, Adrenergic Agents, Pacemaker, Artificial, Hematoma
< Back to Listings