Chief complaint: Chest pain and dyspnea on exertion.
History of present illness: A 61-year-old woman presents for preoperative evaluation prior to a cosmetic procedure. She reports persistent exertional dyspnea and chest discomfort for the prior year. Her chest discomfort is substernal in location, burning in nature, and radiating to the left side. Her symptoms are episodic, occur with moderate exertion, last 10-20 min, and resolve with rest. She underwent coronary angiography in the prior year for similar symptoms, which showed right coronary artery (RCA) stenosis that was treated with a drug-eluting stent; however, mild symptoms have persisted since.
Past medical history: Coronary artery disease with a prior RCA percutaneous coronary intervention, hypertension, gastroesophageal reflux disease, nephrolithiasis
Past surgical history: Cesarean section
Family history: No significant family history is known; father and mother died of unknown disease in old age
Medications: Aspirin, ticagrelor, atorvastatin, metoprolol succinate
Physical examination findings:
Height: 1.5 m
Weight: 74 kg
Body mass index: 33 kg/m2
Blood pressure (BP): 143/86 mm Hg
Heart rate (HR): 65 bpm
Respiratory rate: 14 breaths/min
Temperature: 35.67°C
General appearance: Comfortable
Head and neck: Jugular venous pressure 6 cm H2O and normal carotid upstroke
Chest: Clear lung fields
Cardiac examination: Nondisplaced point of maximal impulse, regular rate and rhythm, grade 2/6 soft systolic murmur auscultated in the left second intercostal space and increased with a squat-to-stand maneuver
Abdomen: Soft, nontender, nondistended
Extremities: Warm and well perfused; no peripheral edema
Neurologic: Alert and oriented, without any focal deficits
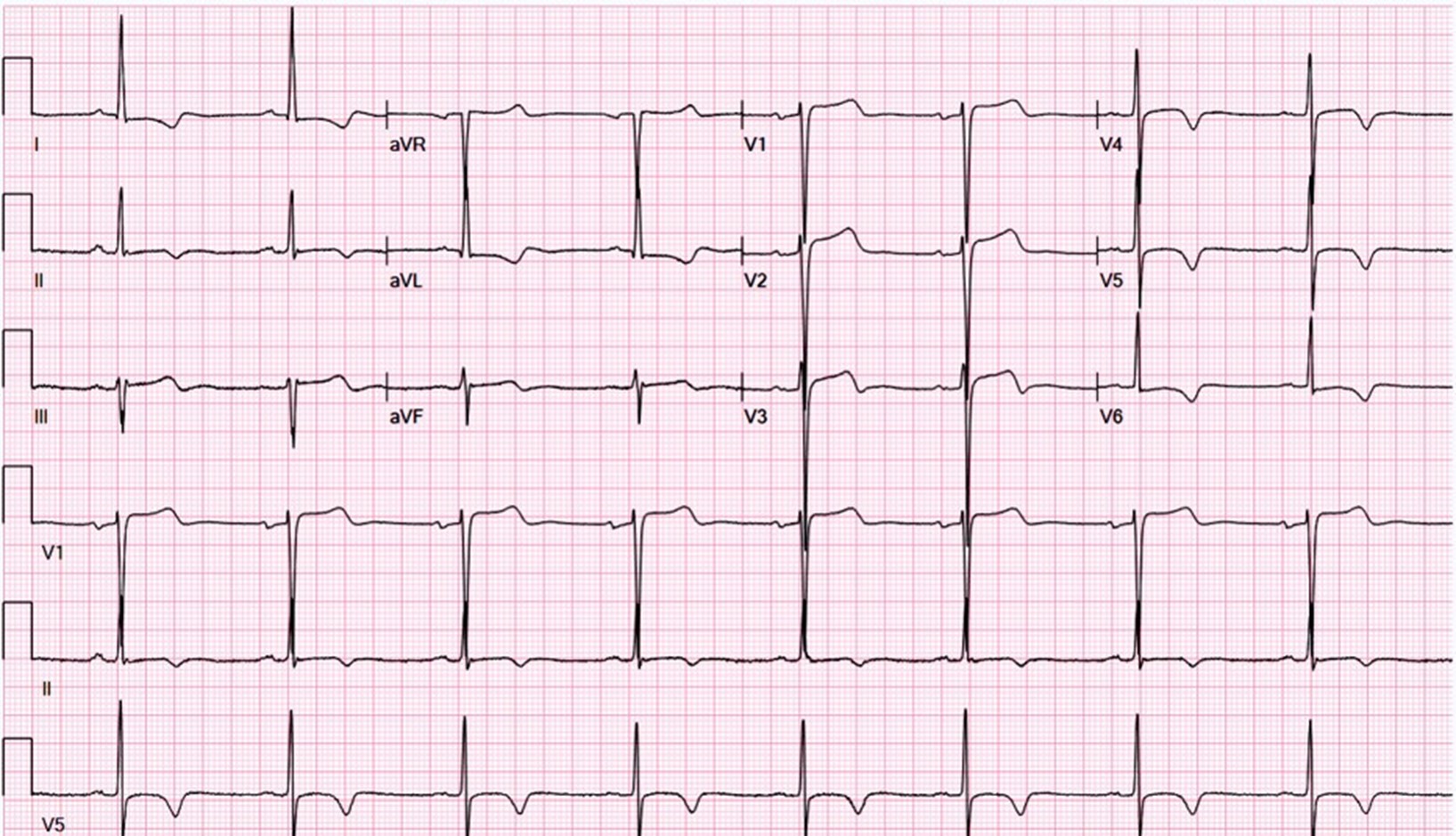
Electrocardiography: Sinus rhythm; left ventricular hypertrophy (LVH) with repolarization abnormalities, including T-wave inversions in the lateral and high lateral leads (Figure 1)
Figure 1
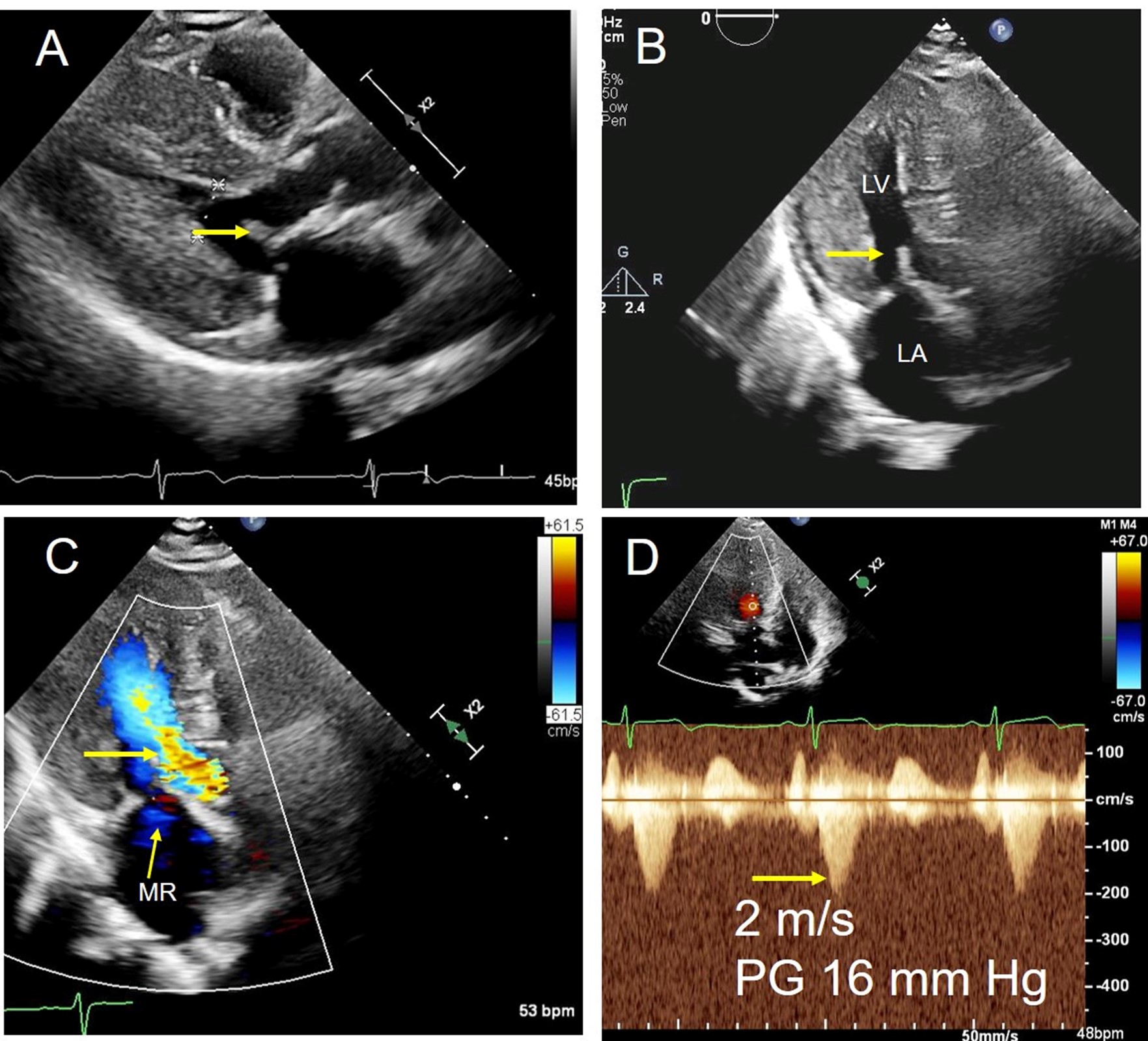
Echocardiography: Severe concentric LVH (interventricular septum diameter 1.7 cm, left ventricular [LV] posterior wall diameter 1.8 cm), small LV cavity size, hyperdynamic LV function with LV ejection fraction 75% (Figures 2, 3)
Figure 2
 PLAX view showing LVH.
PLAX view showing LVH.
LVH = left ventricular hypertrophy; PLAX = parasternal long-axis.
LVH = left ventricular hypertrophy; PLAX = parasternal long-axis.
Figure 3
 Apical five-chamber view showing trace MR and minimal turbulence in the LVOT.
Apical five-chamber view showing trace MR and minimal turbulence in the LVOT.
LVOT = left ventricular outflow tract; MR = mitral regurgitation.
LVOT = left ventricular outflow tract; MR = mitral regurgitation.
Doppler echocardiography at rest: Trace mitral regurgitation (MR), no MR signal; left ventricular outflow tract (LVOT) velocity 2 m/sec and LVOT gradient 16 mm Hg (Figure 4)
Figure 4
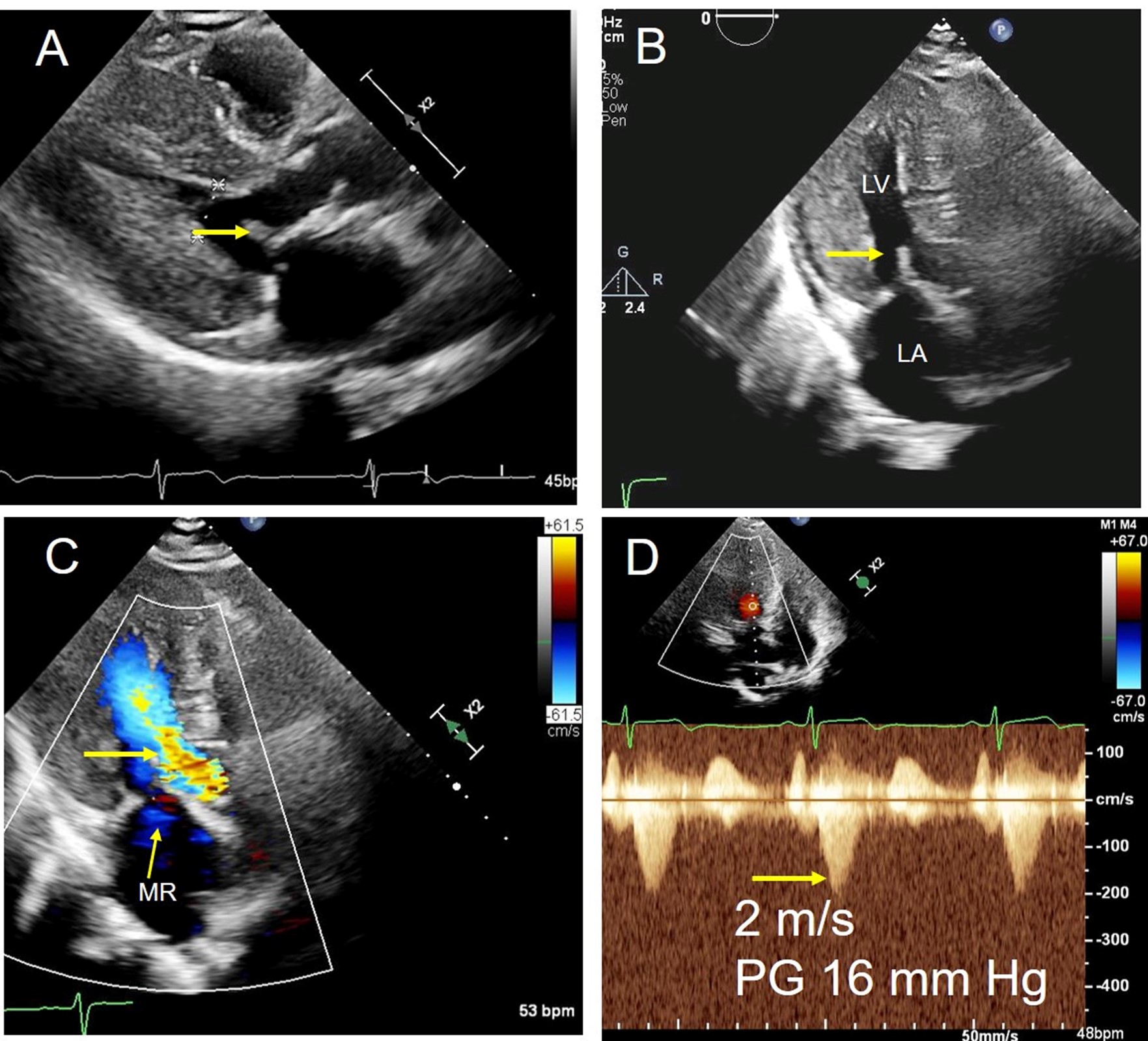 (Panel A) PLAX view in midsystole (arrow pointing toward the anterior mitral leaflet). (Panel B) Apical five-chamber view in midsystole (arrow pointing toward anterior mitral leaflet). (Panel C) Color Doppler in apical five-chamber view showing mild MR (thin arrow) and mild turbulence in the LVOT (thick arrow). (Panel D) CW Doppler in the LVOT, showing velocity 2 m/sec (i.e., 16 mm Hg gradient at rest).
(Panel A) PLAX view in midsystole (arrow pointing toward the anterior mitral leaflet). (Panel B) Apical five-chamber view in midsystole (arrow pointing toward anterior mitral leaflet). (Panel C) Color Doppler in apical five-chamber view showing mild MR (thin arrow) and mild turbulence in the LVOT (thick arrow). (Panel D) CW Doppler in the LVOT, showing velocity 2 m/sec (i.e., 16 mm Hg gradient at rest).
CW = continuous-wave; LA = left atrium; LV = left ventricle; LVOT = left ventricular outflow tract; MR = mitral regurgitation; PG = pressure gradient; PLAX = parasternal long-axis.
CW = continuous-wave; LA = left atrium; LV = left ventricle; LVOT = left ventricular outflow tract; MR = mitral regurgitation; PG = pressure gradient; PLAX = parasternal long-axis.
These findings are consistent with symmetric concentric hypertrophic cardiomyopathy (HCM) with mild systolic anterior motion (SAM) and mild resting gradient of 16 mm Hg. In patients with hypertrophic obstructive cardiomyopathy (HOCM), the severity of obstruction can be highly variable depending on multiple factors such as BP, preload, and HR, among others. In those with suspected obstruction and a resting LVOT gradient <30 mm Hg, provocative maneuvers are indicated (e.g., Valsalva or an exercise echocardiogram).
Stress echocardiography is performed next to assess the exercise LVOT gradient for evaluation of obstructive physiology because the patient has ongoing exertional symptoms. After 8.3 METs of exercise per the modified Bruce protocol, she develops dyspnea. Echocardiography at this time shows no wall motion abnormalities and images are obtained for evaluation of exercise-related hemodynamics (Figure 5). Poststress maximal HR is 131 bpm; however, it drops to 72 bpm by the time imaging is performed.
Figure 5
 Apical four-chamber view showing worsened LVOT turbulence and posterolaterally directed MR after peak stress.
Apical four-chamber view showing worsened LVOT turbulence and posterolaterally directed MR after peak stress.
LVOT = left ventricular outflow tract; MR = mitral regurgitation.
LVOT = left ventricular outflow tract; MR = mitral regurgitation.
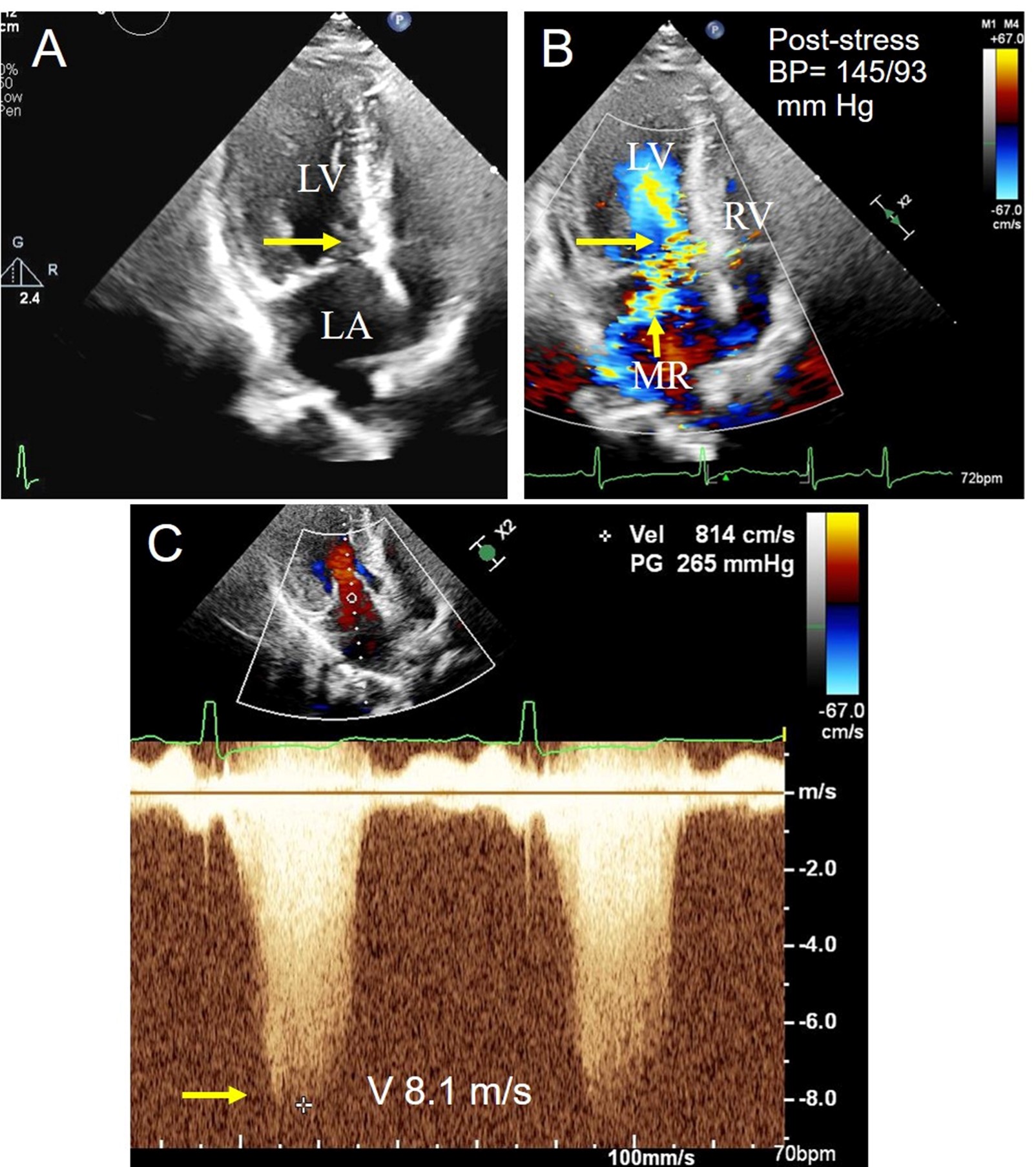
Poststress imaging shows worsened LVOT obstruction and MR. Poststress BP is 145/93 mm Hg. A continuous-wave (CW) Doppler is obtained at this point (Figure 6).
Figure 6
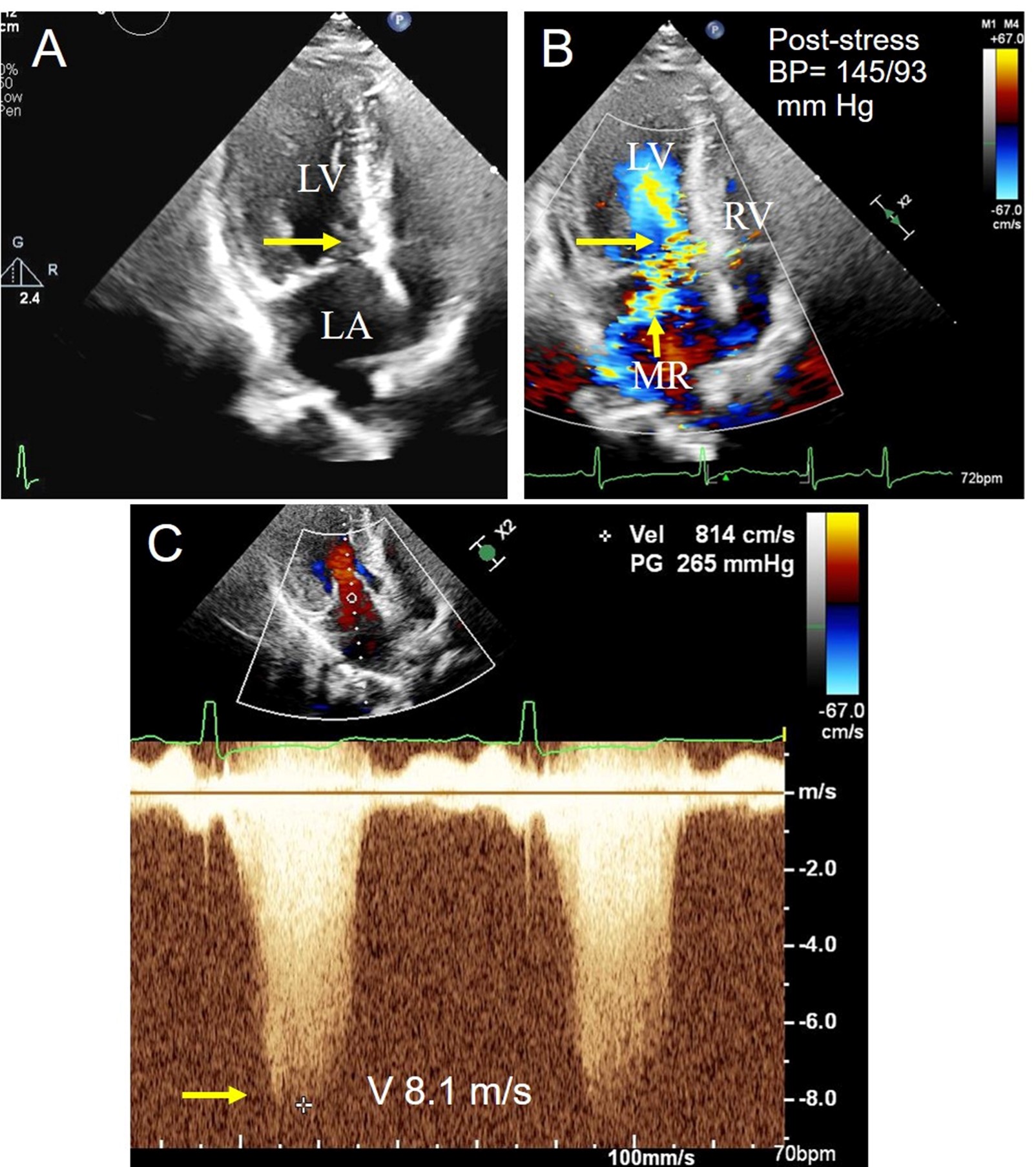 (Panel A) Apical four-chamber view (arrow pointing toward SAM). (Panel B) Apical four-chamber view with color Doppler showing worsened LVOT gradient (long arrow) and MR (short arrow). (Panel C) CW Doppler signal at peak stress, with maximal velocity and calculated pressure gradient.
(Panel A) Apical four-chamber view (arrow pointing toward SAM). (Panel B) Apical four-chamber view with color Doppler showing worsened LVOT gradient (long arrow) and MR (short arrow). (Panel C) CW Doppler signal at peak stress, with maximal velocity and calculated pressure gradient.
BP = blood pressure; CW = continuous-wave; LA = left atrium; LV = left ventricle; LVOT = left ventricular outflow tract; MR = mitral regurgitation; RV = right ventricle; SAM = systolic anterior motion; V = velocity.
BP = blood pressure; CW = continuous-wave; LA = left atrium; LV = left ventricle; LVOT = left ventricular outflow tract; MR = mitral regurgitation; RV = right ventricle; SAM = systolic anterior motion; V = velocity.
The correct answer is: B. 130 mm Hg.
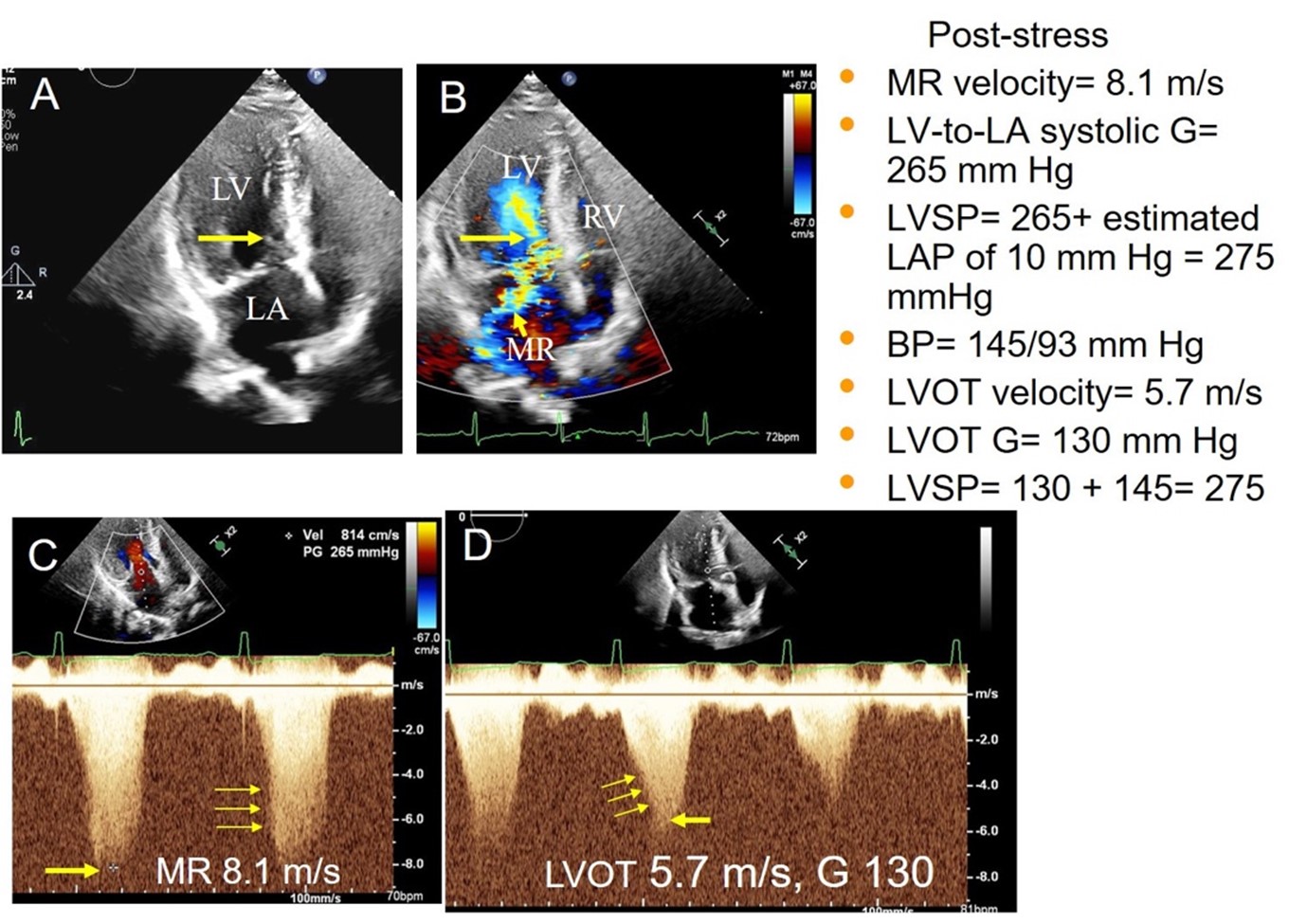
Figure 7 provides an explanation.
Figure 7
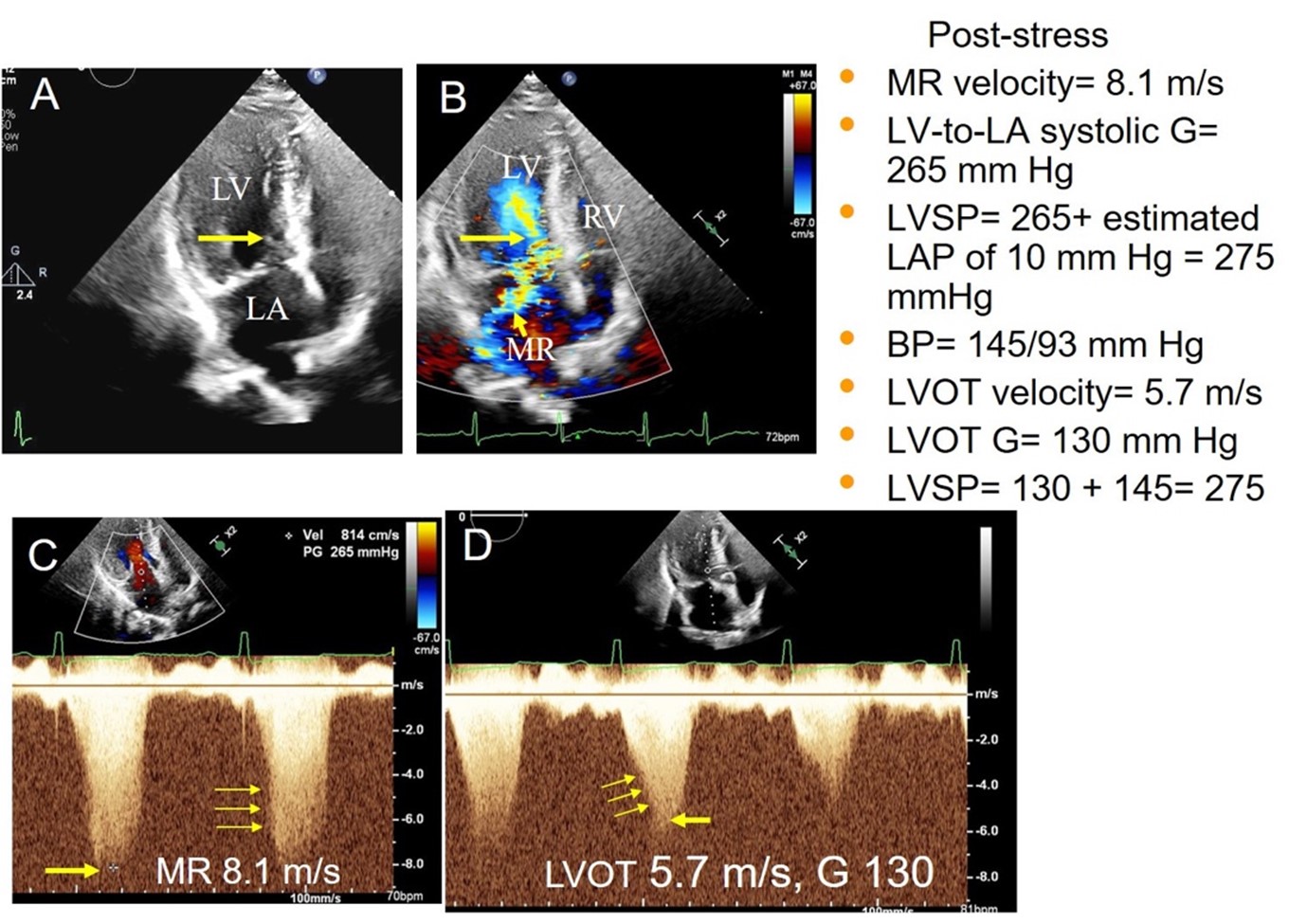 (Panel A) Apical four-chamber view (arrow pointing toward SAM). (Panel B) Color Doppler showing severe LVOT turbulence and moderate to severe posterolaterally directed MR. (Panel C) MR signal with peak velocity and gradient. (Panel D) LVOT signal with peak velocity and gradient. The middle signal shows the accurate LVOT signal; the first signal is likely mixed with the MR and the third signal appears incomplete (thin yellow arrows define the characteristic envelope shapes of both the MR and LVOT signal).
(Panel A) Apical four-chamber view (arrow pointing toward SAM). (Panel B) Color Doppler showing severe LVOT turbulence and moderate to severe posterolaterally directed MR. (Panel C) MR signal with peak velocity and gradient. (Panel D) LVOT signal with peak velocity and gradient. The middle signal shows the accurate LVOT signal; the first signal is likely mixed with the MR and the third signal appears incomplete (thin yellow arrows define the characteristic envelope shapes of both the MR and LVOT signal).
BP = blood pressure; G = gradient; LA = left atrium; LAP = left atrial pressure; LV = left ventricle; LVOT = left ventricular outflow tract; LVSP = left ventricular systolic pressure; MR = mitral regurgitation; PG = pressure gradient; RV = right ventricle; SAM = systolic anterior motion; Vel = velocity.
BP = blood pressure; G = gradient; LA = left atrium; LAP = left atrial pressure; LV = left ventricle; LVOT = left ventricular outflow tract; LVSP = left ventricular systolic pressure; MR = mitral regurgitation; PG = pressure gradient; RV = right ventricle; SAM = systolic anterior motion; Vel = velocity.
Answer choice A is an incorrect choice because the CW Doppler is showing the MR signal as noted by the characteristic envelope shape (as opposed to the LVOT signal). The MR signal will provide the LV-to–left atrium (LA) gradient, not the LVOT gradient.
Answer choice B is the correct choice. After one correctly identifies that the CW Doppler signal in this case is the MR signal, the LV-LA gradient is calculated to be 265 mm Hg (4V2). The left ventricular systolic pressure (LVSP) is then estimated by the formula LV-LA gradient + estimated LA pressure (assumed to be 10-15 mm Hg), which calculates to 275 mm Hg (265 + 10 mm Hg). The LVOT gradient is then estimated by the formula estimated LVSP – systolic BP, which reveals the correct answer choice of 130 mm Hg (275 – 145 mm Hg).
Answer choices C and D are incorrect choices.
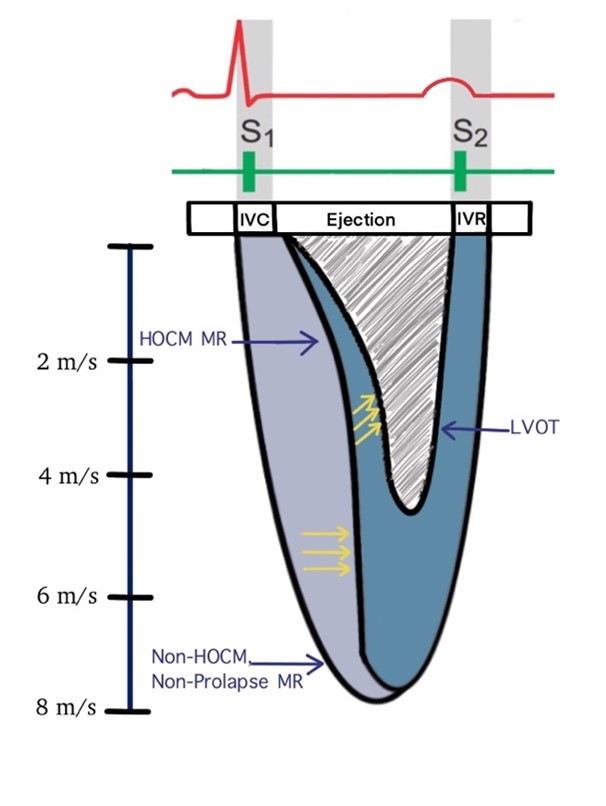
Accurate measurement of the LVOT gradient is critical in the diagnosis and management of HOCM. Apical imaging with color and CW Doppler provides the necessary information to assess LVOT obstruction. When using CW, special caution should be taken to localize and differentiate the LVOT gradient from the MR gradient, and to identify characteristic signal patterns of MR in HOCM (Figure 8).
Figure 8
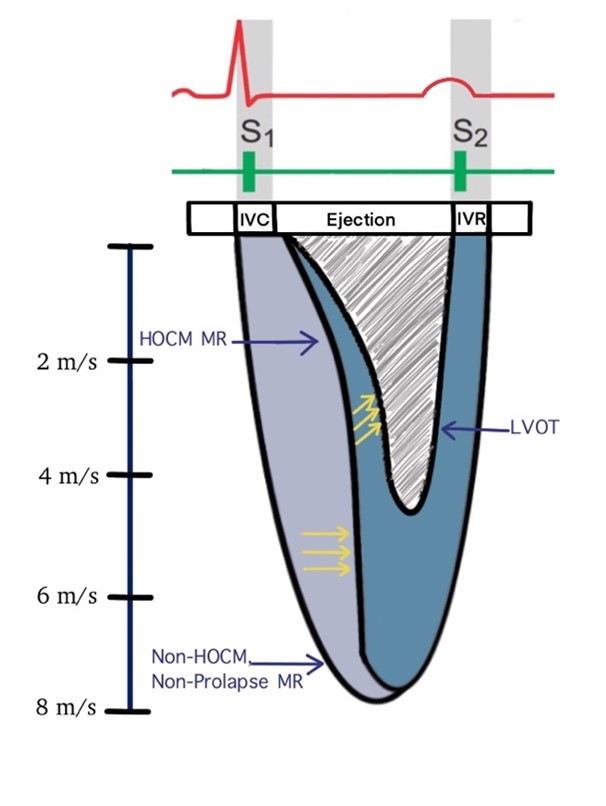 Characteristic signal envelopes of HOCM MR, non-HOCM/nonprolapse MR, and LVOT.
Characteristic signal envelopes of HOCM MR, non-HOCM/nonprolapse MR, and LVOT.
HOCM = hypertrophic obstructive cardiomyopathy; IVC = isovolumetric contraction; IVR = isovolumetric relaxation; LVOT = left ventricular outflow tract; MR = mitral regurgitation.
HOCM = hypertrophic obstructive cardiomyopathy; IVC = isovolumetric contraction; IVR = isovolumetric relaxation; LVOT = left ventricular outflow tract; MR = mitral regurgitation.
Differentiating the HOCM MR Signal From the LVOT Signal
The appearance of the HOCM MR and LVOT signals can be confusing and the differentiation can be challenging. If the MR signal is mistaken as an LVOT signal, the LVOT gradient can be overestimated. The features listed in Table 1 help differentiate these signals:
Table 1
| HOCM MR Signal |
LVOT Signal |
- MR signal velocity is always higher because it gives the LV-to-LA gradient
|
- LVOT signal velocity is lower
|
- HOCM MR envelope is wider, begins after the onset of ejection, and terminates at the end of IVR
|
- LVOT signal is narrower and spans the ejection time
|
- Curved initially but then straightens out (perpendicular to baseline) by midsystole
|
- Characteristic late peaking, dagger shaped, and continues to show rightward curvature in mid-late systole
|
HOCM = hypertrophic obstructive cardiomyopathy; IVR = isovolumetric relaxation; LA = left atrial; LV = left ventricular; LVOT = left ventricular outflow tract; MR = mitral regurgitation.
Differentiating the HOCM MR Signal From Other Causes of MR
- Most other MR signals (except mitral valve [MV] prolapse) have onset at the isovolumetric contraction (IVC) phase and last until isovolumetric relaxation (IVR; i.e., pansystolic MR).
- HOCM MR begins after IVC during the ejection phase but persists until IVR.
- This gives the HOCM MR signal its characteristic initial curved appearance, which is different from most other MR signals.
In HOCM, LV ejection is followed by LVOT obstruction and then onset of MR due to the SAM of the MV and disruption of coaptation between the two leaflets. This sequence of events in HOCM has been referred to as the eject-obstruct-leak sequence.
Educational grant support provided by: Bristol Myers Squib
To visit the course page for the Hypertrophic Cardiomyopathy: Accelerating Guideline-Driven Care grant, click here.
References
- Ommen S, Mital S, Burke M, et al. 2020 ACC/AHA guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2020;76:3022-55.
- Nagueh SF, Bierig SM, Budoff MJ, et al.; American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, Society of Cardiovascular Computed Tomography. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with hypertrophic cardiomyopathy: endorsed by the American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr 2011;24:473-98.
- Woo A, Jedrzkiewicz S. The mitral valve in hypertrophic cardiomyopathy: it's a long story. Circulation 2011;124:9-12.
- Adelman AG, McLoughlin MJ, Marquis Y, Auger P, Wigle ED. Left ventricular cineangiographic observations in muscular subaortic stenosis. Am J Cardiol 1969;24:689-97.