Hypertrophic Cardiomyopathy 2020: Updates, Clarity and Progress for HCM
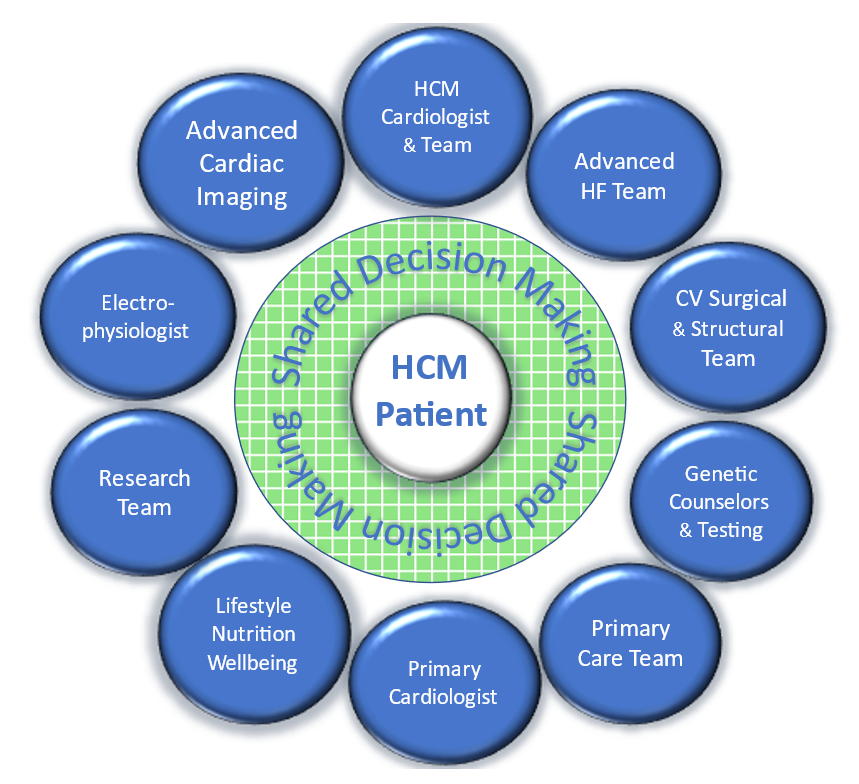
Towards the end of 2020, there was an important, somewhat quietly published document germane to the Sports and Exercise section community, the updated American Heart Association and American College of Cardiology clinical practice guidelines on the management of hypertrophic cardiomyopathy (HCM).1 These updated recommendations provide new evidence as well as a better understanding of earlier evidence in the management of HCM. In addition, several complicated and controversial HCM topics were addressed. From the initial planning meeting, the focus was on how to align the recommendations into a workflow that mirrors a patient evaluation including specific discussions on the management of obstructive versus nonobstructive HCM. In addition, we had an HCM patient advocate on the committee to assist with language and layout. The patient-centered multidisciplinary approach to HCM was well summarized in a recent editorial by an HCM expert and a patient with HCM.2 This summary helped frame the recommendations in the manner it was expected to be received; as a team of clinicians who care for patients with HCM. Figure 1 illustrates the Chanin T. Mast HCM program's vision of how we aspire to provide multidisciplinary care using a shared decision-making (SDM) filter for decisions for the patient with HCM.
Figure 1
The new recommendations reflect updated evidence on diagnostic modalities such as electrocardiography, imaging, and genetic testing. Cardiac imaging was highlighted as having an important role in the diagnosis and clinical decision-making for patients with HCM. Of course, the primary imaging tool remains echocardiography for diagnosis, determination of obstructive physiology, and assessment of risk. The significant impact of cardiovascular magnetic resonance imaging was also recognized for its diagnostic capabilities and utility in defining prognosis and guiding decision-making for placement of an implantable cardioverter-defibrillator (ICD). Clarity regarding assessment of risk for sudden cardiac arrest (SCA) was provided, including the recognition of novel risk factors such as apical aneurysm, decreased left ventricular systolic function, and extensive gadolinium enhancement. Pertinent to providers looking after minors, guidance for HCM SCA risk factors in children, who have different risk thresholds for ICD implantation compared to adults with HCM, was added to this new document.
The updated guideline provides a framework to aid the appropriate utilization of various therapeutic strategies, including medications and invasive therapies for septal reduction. The optimal use of genetic testing for patients with HCM and their families is reviewed, which can have important implications for sports cardiologists when dealing with athletes with left ventricular hypertrophy. Specifically, genetic assessment should be performed in a specialized multidisciplinary HCM center experienced in genetic counseling and testing. Clinical examples include downstream testing using known HCM genetic markers and clarity for genotype positive and phenotype negative patients that do not require athletic restrictions but require continuous annual surveillance for phenotypic expression. The diagnostic work-up, genetic and family screening, risk stratification approaches, lifestyle modifications, medical therapies, and surgical and catheter interventions all constitute the components of guideline-directed care for the HCM patient.
In contrast to the 2011 guideline, the 2020 guideline emphasizes SDM to personalize treatment plans based on the patient's goals and values. SDM involves a dialogue between the patient and care team in the review of testing and treatment options, discussion of the risks and benefits of treatment options, and importantly, engagement of the patient and family to express their own values. This is a common practice for medical professionals, including those who focus on the care of athletes and HCM patient care. The discussion should include development of a care plan regarding genetic evaluation, activity, lifestyle, and therapy choices, along with full disclosure of the risks, benefits, and anticipated outcomes of all options. SDM between patients and providers can lead to better patient-centered outcomes.
Most HCM patients are cared for and evaluated by a cardiovascular care team. The guideline offers a strong recommendation for patients facing complex decisions to be referred to multidisciplinary HCM centers to optimize care. Specialized needs, complex and evolving clinical management, access to research trials, and the relatively uncommon prevalence of HCM in many clinical practices have created a greater demand for clinical HCM centers. Consultation with or referral to a comprehensive or primary HCM center for collaboration in complex disease-related management decisions is emphasized. This is the setting where discussions around participation in healthy physical activity/exercise guidance is best provided. For most patients with HCM, mild-to-moderate-intensity recreational exercise is beneficial to improve cardiorespiratory fitness, physical functioning, quality of life, and for overall improved health in keeping with physical activity guidelines for the general population.3 Recreational exercise of mild-to-moderate intensity has not been associated with increased risk of ventricular arrhythmias in recent studies,4-8 which led to a new class I recommendation for mild-to-moderate exercise in most HCM patients highlighting the beneficial effects of exercise.
In selected patients with HCM, a class IIb recommendation was new to encourage HCM experts, after a comprehensive evaluation, to discuss the potential risks of competitive sports participation. For most patients with HCM, participation in low-intensity competitive sports is reasonable. Participation in other competitive sports may be considered in select patients only after a complete assessment and discussion between the patient and care team about their individual risk. In patients without high-risk features for SCA related to HCM (such as extensive late gadolinium enhancement, systolic dysfunction, marked hypertrophy), expert discussion about sport participation is supported under these updated recommendations. This is one aspect of how SDM is highlighted and utilized for HCM care.
In addition to sports participation, patients with HCM also have several occupational considerations addressed in the new document. Providers caring for patients with HCM were instructed to follow Federal Motor Carrier Safety Administration cardiovascular disease guidelines. Patients managed by a guideline-directed management plan are permitted to drive commercial motor vehicles if they do not have an ICD or any major risk factors for SCA.
Finally, the group acknowledged that many of the recommendations were based on observational data or expert opinion and urged for more randomized controlled trials in the HCM space. Additional, unmet needs include management strategies to improve functional capacity, attenuate or halt disease progression, and reduce adverse outcomes.
The evaluation and management of athletes with suspected or confirmed HCM is often encountered in sports cardiology clinics. As is customary for the sports cardiologist, care decisions require comprehensive disease understanding, assessment of individual risk, and often requires a team approach to reduce risk and maximize the patient-physician interaction.
References
- Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2020;76:3022-55.
- Semsarian C, Davis L. The wait is over: the 2020 American Heart Association/American College of Cardiology (AHA/ACC) Hypertrophic Cardiomyopathy Guidelines have arrived. Heart Lung Circ 2021;Feb 17:[Epub ahead of print].
- Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA 2018;320:2020-28.
- Turkowski KL, Bos JM, Ackerman NC, Rohatgi RK, Ackerman MJ. Return-to-play for athletes with genetic heart diseases. Circulation 2018;137:1086-88.
- Pelliccia A, Lemme E, Maestrini V, et al. Does sport participation worsen the clinical course of hypertrophic cardiomyopathy? Clinical outcome of hypertrophic cardiomyopathy in athletes. Circulation 2018;137:531-33.
- Lampert R, Olshansky B, Heidbuchel H, et al. Safety of sports for athletes with implantable cardioverter-defibrillators: long-term results of a prospective multinational registry. Circulation 2017;135:2310-12.
- Dejgaard LA, Haland TF, Lie OH, et al. Vigorous exercise in patients with hypertrophic cardiomyopathy. Int J Cardiol 2018;250:157-63.
- Sweeting J, Ingles J, Ball K, Semsarian C. A control theory-based pilot intervention to increase physical activity in patients with hypertrophic cardiomyopathy. Am J Cardiol 2018;122:866-71.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Sports and Exercise Cardiology, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Heart Failure and Cardiac Biomarkers, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Sports and Exercise and Imaging
Keywords: Sports, Athletes, Quality of Life, Gadolinium, Contrast Media, Hypertrophy, Left Ventricular, American Heart Association, Genetic Markers, Defibrillators, Implantable, Cardiovascular Diseases, Decision Making, Patient Advocacy, Magnetic Resonance Imaging, Echocardiography, Risk Assessment, Arrhythmias, Cardiac, Risk Factors, Patient Care, Cardiomyopathy, Hypertrophic, Life Style, Disease Progression, Patient-Centered Care
< Back to Listings