Hybrid Convergent Ablation for the Treatment of Persistent and Long-Standing Persistent AF: Results of CONVERGE Trial
Quick Takes
- The hybrid Convergent procedure has superior effectiveness compared with endocardial-only ablation in patients with advanced atrial fibrillation (AF).
- A heart team approach (i.e., collaboration between electrophysiologists and cardiac surgeons) helps improve outcomes in patients with advanced AF.
Introduction
AF affects 33 million people worldwide. Approximately 70% of these people have either persistent or long-standing persistent AF.1,2 Although pulmonary vein (PV) isolation is effective in treating paroxysmal AF, its effectiveness for treatment of persistent forms of AF is limited due to atrial remodeling and increased left atrial (LA) size that occur as AF progresses.3,4
LA Posterior Wall: Substrate for Sustaining AF
In patients with advanced AF, the extra-PV triggers drive and sustain AF.5-7 The LA posterior wall has been shown to have the highest proportion of non-PV triggers and is the most common site for AF re-entrant drivers.7 The posterior wall shares tissue origin with the PVs and has unique electrophysiological characteristics (i.e., short refractory period and high density of autonomic neurons), all of which contribute to initiation and maintenance of AF.8-10 Increased pressure and LA dilation due to prolonged AF cause stretching and inflammation, leading to fibrosis, which contributes to micro-re-entry.11-13 Another phenomenon that occurs as a result of progressive structural remodeling is dissociation of epicardial and endocardial activation patterns, allowing fibrillation waves to propagate between epicardium and endocardium, further adding to fibrillatory conduction.14
Challenges With Endocardial Ablation of Posterior Wall
Due to increasing evidence that the posterior wall provides substrate for maintaining AF, endocardial ablation of the posterior wall has been explored. Despite high acute success, substantial rates of posterior wall reconnections have been reported at repeat electrophysiology procedures, indicating difficulty in creating transmural and durable lesions.15-18
The lack of a standardized lesion set, challenges of achieving transmural lesions, and endocardial/epicardial dissociation in AF together contribute to limited effectiveness of endocardial posterior wall isolation. Furthermore, attempts to improve endocardial lesion depth and durability with higher power, force, or duration may increase procedural risks, including injury to periesophageal branches of vagus nerve and esophageal injury such as atrioesophageal fistula.
Combined Epicardial Endocardial Ablation: Hybrid Convergent Procedure
Due to these challenges, a hybrid approach combining epicardial and endocardial ablation was introduced. Specifically, the hybrid Convergent procedure combines epicardial ablation of PVs and LA posterior wall followed by endocardial mapping and ablation to complete PV isolation or address gaps. The epicardial ablation is conducted by a cardiothoracic surgeon via sub-xyphoid access to the pericardium and under direct visualization. The endocardial procedure is conducted by the electrophysiologist in standard fashion.
The published outcomes of the hybrid Convergent procedure using the contemporary lesion set are favorable.19 These are supported by the results of the CONVERGE (Convergence of Epicardial and Endocardial Ablation for the Treatment of Symptomatic Persistent AF) prospective, multi-center, randomized clinical trial that demonstrated improved effectiveness of the hybrid Convergent procedure over endocardial catheter ablation.20
CONVERGE Clinical Trial
The CONVERGE trial was performed to evaluate the safety of combined epicardial endocardial ablation and compare its effectiveness to endocardial ablation alone for treatment of persistent and long-standing persistent AF.
Primary effectiveness was freedom from atrial arrhythmia absent new/increased dosage of previously failed/intolerant Class I/III antiarrhythmic drugs (AADs) through 12 months. Primary safety was major adverse events through 30 days.
The key secondary effectiveness measures included AF burden reduction, defined as the proportion of patients achieving at least 90% reduction in AF burden at 12 months (24-hour Holter monitor) and 18 months (7-day Holter monitor) compared with baseline, and AF freedom through 12 months and 18 months.
Pertinent Findings
A total of 153 patients was randomized (2:1) and treated with hybrid Convergent versus endocardial catheter ablation. In the Convergent arm, the mean ablation time was 42.9 ± 13.7 minutes for the epicardial portion and 135.8 ± 49.9 minutes for the endocardial portion of the procedure. In the catheter ablation arm, mean ablation time was 171.4 ± 59.7 minutes. The addition of epicardial ablation resulted in 35.6 minutes of saving to the endocardial ablation time.
The Convergent procedure had superior effectiveness compared with endocardial ablation alone. A significantly higher number of patients in the hybrid Convergent arm achieved ≥90% reduction in AF burden and freedom from AF at 12 months compared with the endocardial ablation arm, and this difference was sustained at 18 months. Additionally, a significantly higher number of patients in the hybrid Convergent arm remained free from cardioversion (Figures 1-3).
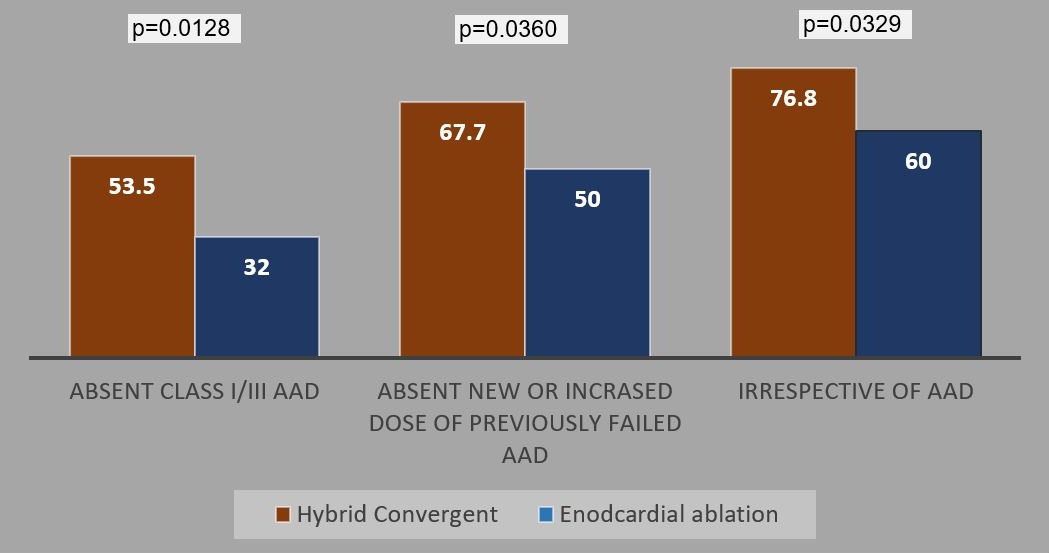
Figure 1: Effectiveness Through 12 Months Stratified by AAD Use
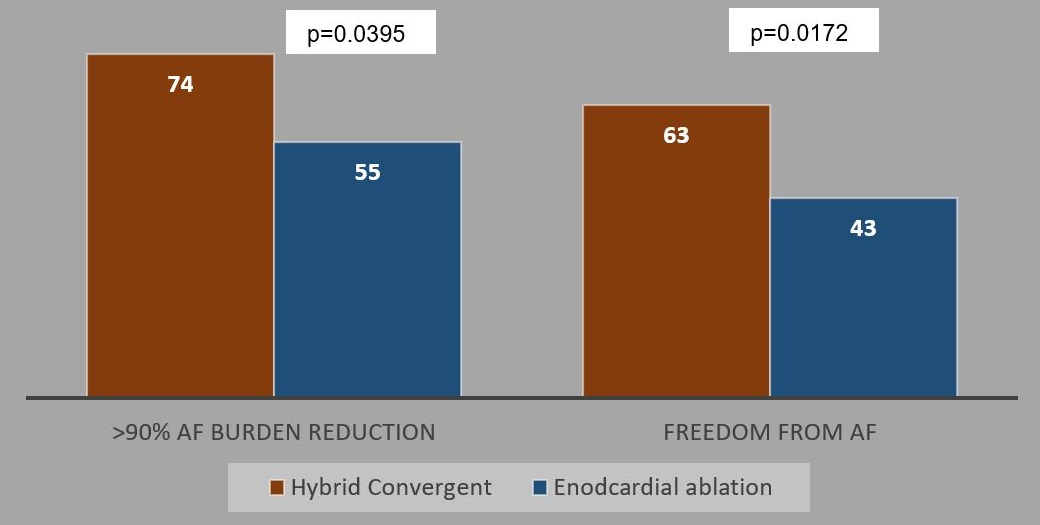
Figure 2: AF Burden Reduction and Freedom From AF Through 18 months Absent an Increased Dose or New Class I/III AADs
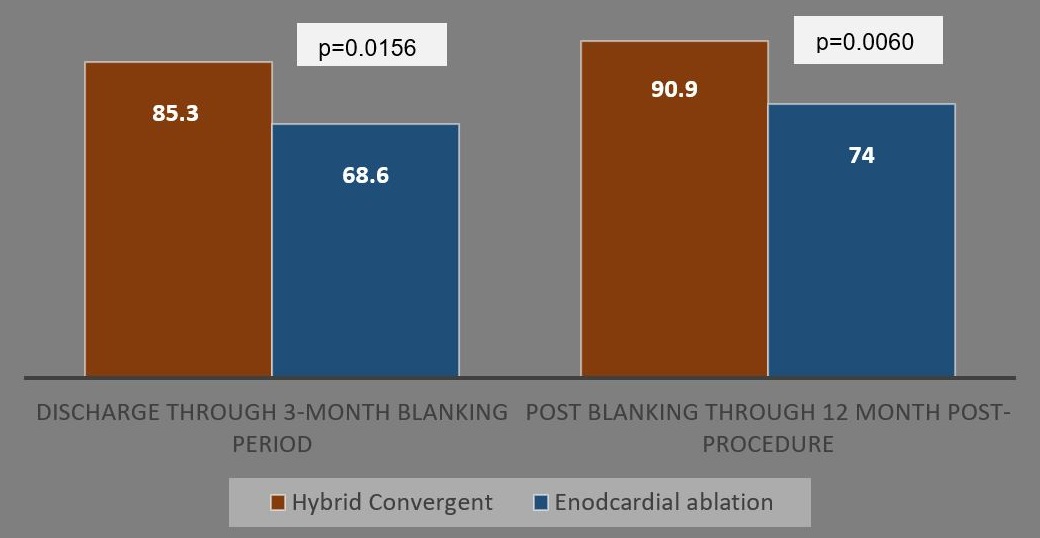
Figure 3: Freedom From Cardioversion
There were no deaths, cardiac perforations, or atrioesophageal fistulas. Three patients (2.9%; 3/102) reported safety events within 7 days post-procedure: 1 each of stroke, excessive bleeding, and excessive bleeding with late pericardial effusion. After day 7 and through 30 days, 5 patients (5/102; 4.9%) reported safety events: 3 pericardial effusions, 1 phrenic nerve injury, and 1 transient ischemic attack. These prespecified events were not reported in the endocardial ablation arm (Fisher exact p = 0.0525). The safety rate in the trial was largely driven by late pericardial effusions. These events were delayed inflammatory response to pericardiotomy and ablation. The symptoms included cough, fatigue, shortness of breath without significant hypotension and resolved with a planned pericardial drainage.
Discussion
The CONVERGE trial is the first multicenter, randomized clinical trial to compare the outcomes of combined epicardial and endocardial ablation to endocardial ablation alone for the treatment of persistent AF. The trial imposed no limits on the duration of AF and allowed patients with substantial LA dilation, making it the only ablation trial thus far to include a large portion of patients with long-standing persistent AF (42%), with a mean duration of persistent AF of 4.40 ± 4.71 years.
The trial demonstrates that addition of epicardial ablation to the endocardial ablation results in reduced endocardial ablation time and improved effectiveness outcomes in patients with persistent AF. This high-quality evidence supports transmural posterior wall ablation, in addition to PV isolation, as an effective strategy for treating advanced AF.
The safety of the hybrid Convergent procedure is acceptable. Best practices for management of pericardial effusions such as adequate drain management, anti-inflammatory prophylaxis, and patient monitoring should be implemented for improved safety. Lastly, the study emphasizes collaboration between electrophysiologists and cardiac surgeons for improved outcomes in patients with advanced AF.
Conclusion
The CONVERGE trial demonstrates that a hybrid epicardial endocardial ablation approach has superior effectiveness compared with endocardial-only ablation. These findings have important clinical implications for patients with advanced AF.
References
- Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 2014;129:837-47.
- Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol 2014;6:213-20.
- Scherr D, Khairy P, Miyazaki S, et al. Five-year outcome of catheter ablation of persistent atrial fibrillation using termination of atrial fibrillation as a procedural endpoint. Circ Arrhythm Electrophysiol 2015;8:18-24.
- Clarnette JA, Brooks AG, Mahajan R, et al. Outcomes of persistent and long-standing persistent atrial fibrillation ablation: a systematic review and meta-analysis. Europace 2018;20:f366-f376.
- Lim HS, Hocini M, Dubois R, et al. Complexity and Distribution of Drivers in Relation to Duration of Persistent Atrial Fibrillation. J Am Coll Cardiol 2017;69:1257-69.
- Di Biase L, Burkhardt JD, Mohanty P, et al. Left Atrial Appendage Isolation in Patients With Longstanding Persistent AF Undergoing Catheter Ablation: BELIEF Trial. J Am Coll Cardiol 2016;68:1929-40.
- Lin WS, Tai CT, Hsieh MH, et al. Catheter ablation of paroxysmal atrial fibrillation initiated by non-pulmonary vein ectopy. Circulation 2003;107:3176-83.
- Abdulla R, Blew GA, Holterman MJ. Cardiovascular embryology. Pediatr Cardiol 2004;25:191-200.
- Suenari K, Chen YC, Kao YH, et al. Discrepant electrophysiological characteristics and calcium homeostasis of left atrial anterior and posterior myocytes. Basic Res Cardiol 2011;106:65-74.
- Stavrakis S, Po S. Ganglionated Plexi Ablation: Physiology and Clinical Applications. Arrhythm Electrophysiol Rev 2017;6:186-90.
- Cochet H, Mouries A, Nivet H, et al. Age, atrial fibrillation, and structural heart disease are the main determinants of left atrial fibrosis detected by delayed-enhanced magnetic resonance imaging in a general cardiology population. J Cardiovasc Electrophysiol 2015;26:484-92.
- Burstein B, Nattel S. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J Am Coll Cardiol 2008;51:802-9.
- Yang F, Tiano J, Mittal S, Turakhia M, Jacobowitz I, Greenberg Y. Towards a Mechanistic Understanding and Treatment of a Progressive Disease: Atrial Fibrillation. J Atr Fibrillation 2017;10:1627.
- Verheule S, Eckstein J, Linz D, et al. Role of endo-epicardial dissociation of electrical activity and transmural conduction in the development of persistent atrial fibrillation. Prog Biophys Mol Biol 2014;115:173-85.
- Thiyagarajah A, Kadhim K, Lau DH, et al. Feasibility, Safety, and Efficacy of Posterior Wall Isolation During Atrial Fibrillation Ablation: A Systematic Review and Meta-Analysis. Circ Arrhythm Electrophysiol 2019;12:e007005.
- Markman TM, Hyman MC, Kumareswaran R, et al. Durability of posterior wall isolation after catheter ablation among patients with recurrent atrial fibrillation. Heart Rhythm 2020;17:1740-4.
- Bai R, Di Biase L, Mohanty P, et al. Proven isolation of the pulmonary vein antrum with or without left atrial posterior wall isolation in patients with persistent atrial fibrillation. Heart Rhythm 2016;13:132-40.
- Tahir KS, Mounsey JP, Hummel JP. Posterior Wall Isolation in Atrial Fibrillation Ablation. J Innov Card Rhythm Manag 2018;9:3186-94.
- Wats K, Kiser A, Makati K, et al. The Convergent Atrial Fibrillation Ablation Procedure: Evolution of a Multidisciplinary Approach to Atrial Fibrillation Management. Arrhythm Electrophysiol Rev 2020;9:88-96.
- DeLurgio DB, Crossen KJ, Gill J, et al. Hybrid Convergent Procedure for the Treatment of Persistent and Long-Standing Persistent Atrial Fibrillation: Results of CONVERGE Clinical Trial. Circ Arrhythm Electrophysiol 2020;13:e009288.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Pericardial Disease, Implantable Devices, EP Basic Science, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure
Keywords: Arrhythmias, Cardiac, Anti-Arrhythmia Agents, Pericardial Effusion, Endocardium, Pulmonary Veins, Atrial Remodeling, Ischemic Attack, Transient, Pericardiectomy, Electric Countershock, Phrenic Nerve, Dilatation, Prospective Studies, Catheter Ablation, Atrial Fibrillation, Pericardium, Anti-Inflammatory Agents, Stroke, Vagus Nerve, Fistula, Fibrosis, Hypotension, Surgeons, Inflammation, Monitoring, Physiologic, Fatigue, Reference Standards, Maintenance, Dyspnea, Electrophysiology, Dissociative Disorders, Neurons
< Back to Listings