Medial Artery Calcification: The Silent Killer of the Leg
Quick Takes
- Medial artery calcification is associated with lower limb amputation in patients with diabetes and/or peripheral artery disease.
- The presence of infrapopliteal medial artery calcification identifies an at-risk limb.
Medial artery calcification (MAC) is a condition characterized by the presence of diffuse calcium deposits along the medial layer of the arterial wall resulting in a typical "railroad-track" appearance on plain x-ray imaging.1
MAC was first described in 1903 by Mönckeberg, who wrote "I am unable to prove that calcification can lead to obliteration of the vessel, but some of my anatomical findings make it likely".2 Despite this advice, in the last century MAC has been traditionally considered by most authors as a non-occlusive arterial disease and a benign condition, not requiring any treatment.3 However, in the last decades, it has been extensively shown that MAC is strongly associated with cardiovascular events and death in patients with diabetes mellitus (DM) and/or chronic kidney disease (CKD).1,4-7 In their study on patients with DM, Niskanen et al. found that "surprisingly, the impact of MAC to cardiovascular mortality was substantially stronger than that of intimal artery calcifications".6
The mechanism by which MAC has been traditionally linked to adverse cardiovascular events is an indirect non-occlusive effect consisting in arterial wall stiffening and increase in pulse pressure resulting in left ventricular strain, hypertrophy and decreased myocardial perfusion during diastole.8,9 While this mechanism explains the adverse effects of MAC on cardiac events, it appears to be an insufficient explanation for the peripheral vascular outcomes correlated to MAC. Specifically, MAC has been shown to be strongly associated with peripheral arterial disease (PAD) and chronic limb threatening ischemia, and frequently abundant in the distal arterial bed of amputees for vascular causes.10-13 Moreover, a recent work from our group showed that MAC is strongly associated with small artery disease, a condition defined by the occlusion of small, below-the-ankle arteries, thus jeopardizing the fate of the limb (Figure 1).14
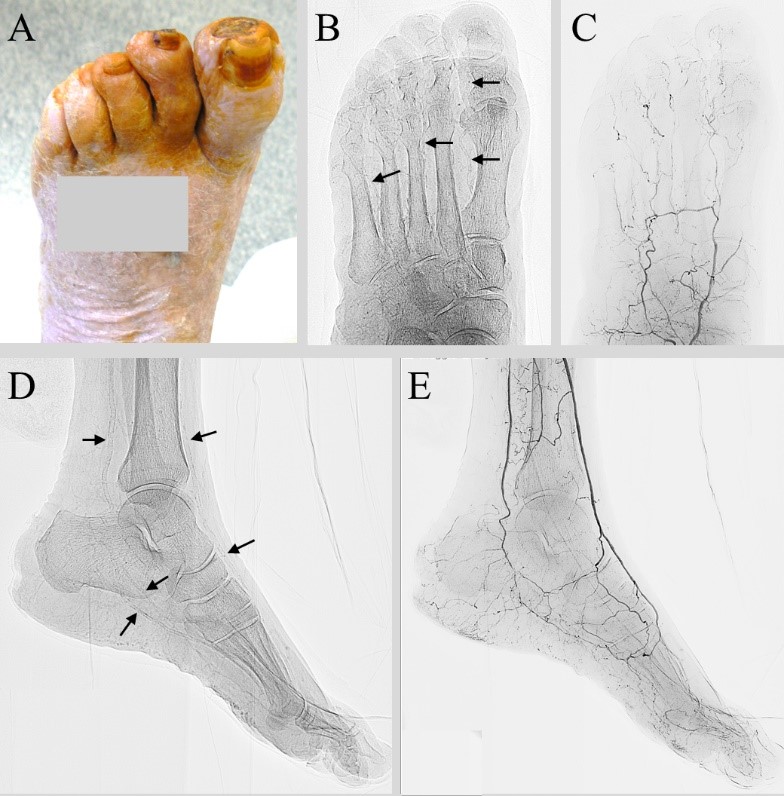
Figure 1
A: apical necrosis of the first and second toes
B: antero-posterior radiograph of the forefoot: metatarsal and digital arteries show the typical railroad calcification pattern (black arrows)
C: antero-posterior forefoot angiography: extreme poverty of the metatarsal and digital arteries
D: latero-lateral radiograph of the foot: anterior tibial, posterior tibial, dorsalis pedis and plantar arteries are calcified (black arrows)
E: latero-lateral angiography of the foot: diffuse disease of the plantar arteries, extreme poverty of the metatarsal and calcaneal branches
These data suggest that infrapopliteal MAC, defined as MAC affecting below-the-knee and/or below-the-ankle arteries, might be a potential risk factor for lower limb amputations (LLAs).
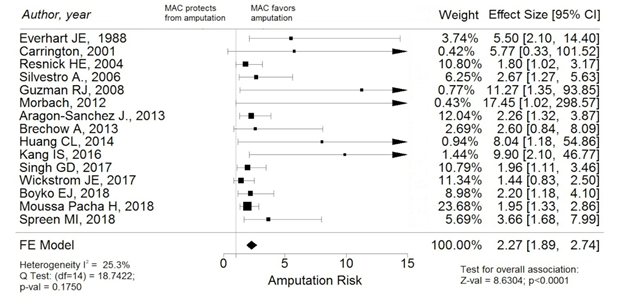
To investigate this hypothesis, we conducted in January 2020 a systematic review of the literature looking for prospective or retrospective observational studies reporting estimates of the association between infrapopliteal MAC and LLAs in patients with either DM or PAD or both.15 We identified fifteen articles eligible for inclusion in the meta-analysis that collectively included 6,489 patients with a median follow up time of 36 months. The presence of MAC was assessed by either direct visualization of calcifications on imaging tests or indirectly by finding a high ankle-brachial-index score, a condition known to be associated with MAC.16 Pooling together original studies' measure of association between MAC and LLAs in a fixed-effect model based meta-analysis, we found a significantly increased risk of undergoing any kind of LLA for patients with infrapopliteal MAC compared to patients without evidence of MAC (pooled adjusted Risk Ratio [RR] 2.27, 95% Confidence Interval [95% CI]: 1.89-2.74; p<0.0001; I2 25.3%), (Figure 2).
Figure 2
Black boxes and black lines: single study effect size and 95% CI (the size of the black box corresponds to the study meta-analytic weight); black diamond: pooled estimated effect size (the diamond width corresponds to 95% CI bounds).
Abbreviations: MAC, medial arterial calcification; LLAs, lower-limb amputations; CI, Confidence Interval; FE, fixed-effect. Reprinted with permission from Losurdo F, Ferraresi R, Ucci A, Zanetti A, Clerici G, Zambon A. Association of infrapopliteal medial arterial calcification with lower-limb amputations in high-risk patients: a systematic review and meta-analysis. Vasc Med 2021;26:164-73.
This association was maintained when restricting the analysis to studies recruiting primarily patients with DM (RR: 2.37; 95% CI: 1.76-3.20, p < 0.0001; I2 = 17%) as well as to studies recruiting primarily patients with PAD (RR: 2.48; 95% CI: 1.72-3.58, p < 0.001; I2 = 43%). The association was still significant when considering as outcome only major amputations (RR: 2.21; 95% CI: 1.65–2.96, p<0.001; I2 = 17%).
In conclusion, our meta-analysis confirms something that several empirical observations have already suggested over the last decades: having significant infrapopliteal MAC is associated with a worse limb outcome, thus providing a further marker of the at-risk limb. In view of this, MAC carriers might be considered as a further group that would benefit from more aggressive follow up, aiming to optimize primary prevention strategies and enable early diagnosis of foot lesions.
References
- Lau WL, Ix JH. Clinical detection, risk factors, and cardiovascular consequences of medial arterial calcification: a pattern of vascular injury associated with aberrant mineral metabolism. Semin Nephrol 2013;33:93-105.
- Mönckeberg JG. Über die reine Mediaverkalkung der Extremitätenarterien und ihr Verhalten zur Arteriosklerose. Virchows Arch Path 1903;171:141-67.
- Silbert S, Lippmann HI, Gordon E. Mönckeberg's arteriosclerosis. AMA Arch Intern Med 1956;97:378-83.
- Rocha-Singh KJ, Zeller T, Jaff MR. Peripheral arterial calcification: prevalence, mechanism, detection, and clinical implications. Catheter Cardiovasc Interv 2014;83:E212-20.
- Lehto S, Niskanen L, Suhonen M, Rönnemaa T, Laakso M. Medial artery calcification. A neglected harbinger of cardiovascular complications in non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol 1996;16:978-83.
- Niskanen L, Siitonen O, Suhonen M, Uusitupa MI. Medial artery calcification predicts cardiovascular mortality in patients with NIDDM. Diabetes Care 1994;17:1252-56.
- London GM, Guérin AP, Marchais SJ, Métivier F, Pannier B, Adda H. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant 2003;18:1731-40.
- Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension 2001;38:938-42.
- London GM, Safar ME, Pannier B. Aortic aging in ESRD: structural, hemodynamic, and mortality implications. J Am Soc Nephrol 2016;27:1837-46.
- Chantelau E, Lee KM, Jungblut R. Distal arterial occlusive disease in diabetes is related to medial arterial calcification. Exp Clin Endocrinol Diabetes 1997;105:11-13.
- Soor GS, Vukin I, Leong SW, Oreopoulos G, Butany J. Peripheral vascular disease: who gets it and why? A histomorphological analysis of 261 arterial segments from 58 cases. Pathology 2008;40:385-91.
- Narula N, Dannenberg AJ, Olin JW, et al. Pathology of peripheral artery disease in patients with critical limb ischemia. J Am Coll Cardiol 2018;72:2152-63.
- Mustapha JA, Diaz-Sandoval LJ, Saab F. Infrapopliteal calcification patterns in critical limb ischemia: diagnostic, pathologic and therapeutic implications in the search for the endovascular holy grail. J Cardiovasc Surg 2017;58:383-401.
- Ferraresi R, Ucci A, Pizzuto A, et al. A novel scoring system for small artery disease and medial arterial calcification is strongly associated with major adverse limb events in patients with chronic limb-threatening ischemia. J Endovasc Ther 2021;28:194-207.
- Losurdo F, Ferraresi R, Ucci A, Zanetti A, Clerici G, Zambon A. Association of infrapopliteal medial arterial calcification with lower-limb amputations in high-risk patients: a systematic review and meta-analysis. Vasc Med 2021;26:164-73.
- Aboyans V, Ho E, Denenberg JO, Ho LA, Natarajan L, Criqui MH. The association between elevated ankle systolic pressures and peripheral occlusive arterial disease in diabetic and nondiabetic subjects. J Vasc Surg 2008;48:1197-1203.
Clinical Topics: Heart Failure and Cardiomyopathies, Prevention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD)
Keywords: Peripheral Arterial Disease, Calcium, Ankle Brachial Index, Amputees, Blood Pressure, Odds Ratio, Retrospective Studies, Diastole, Prospective Studies, Follow-Up Studies, X-Rays, Arteries, Amputation, Diabetes Mellitus, Risk Factors, Renal Insufficiency, Chronic, Ischemia, Early Diagnosis, Primary Prevention, Hypertrophy, Perfusion
< Back to Listings