Heart Transplantation in Adriamycin-Associated Cardiomyopathy: An UNOS Analysis
Quick Takes
- In a large UNOS (United Network for Organ Sharing) analysis of heart transplant recipients, there was no difference in short-term and long-term survival for patients with end-stage adriamycin-associated cardiomyopathy compared to patients with ischemic or dilated cardiomyopathy.1
- Patients with adriamycin-associated cardiomyopathy were younger, more likely women, with higher pulmonary vascular resistance (PVR) but received fewer bridge-to-transplant left ventricular assist devices (LVADs) despite an overall increase in LVAD use during the study period.
- There was no difference in death from malignancy up to 5 years post-transplant.
Objectives
This study sought to provide post-cardiac-transplant survival data in patients with adriamycin-associated cardiomyopathy in the contemporary era of mechanical circulatory support and cardiac transplantation.
Methods
This study included adults ≥18 years of age at listing and undergoing a first-time single-organ heart transplantation from the publicly available UNOS dataset. Patients with physiology that could be supported with an LVAD, including dilated cardiomyopathy, ischemic cardiomyopathy, and the study group (adriamycin-associated cardiomyopathy), were included in the analysis. The study excluded UNOS patients with a previous heart transplant, congenital heart disease, restrictive cardiomyopathy, hypertrophic cardiomyopathy, or valvular heart disease. UNOS patients with biventricular assist devices, right ventricular assist devices, or total artificial hearts at the time of cardiac transplant were also excluded. The primary outcome was time to all-cause mortality after cardiac transplantation. All patients with follow-up times after transplant of >5 years were censored at 5 years.
Results
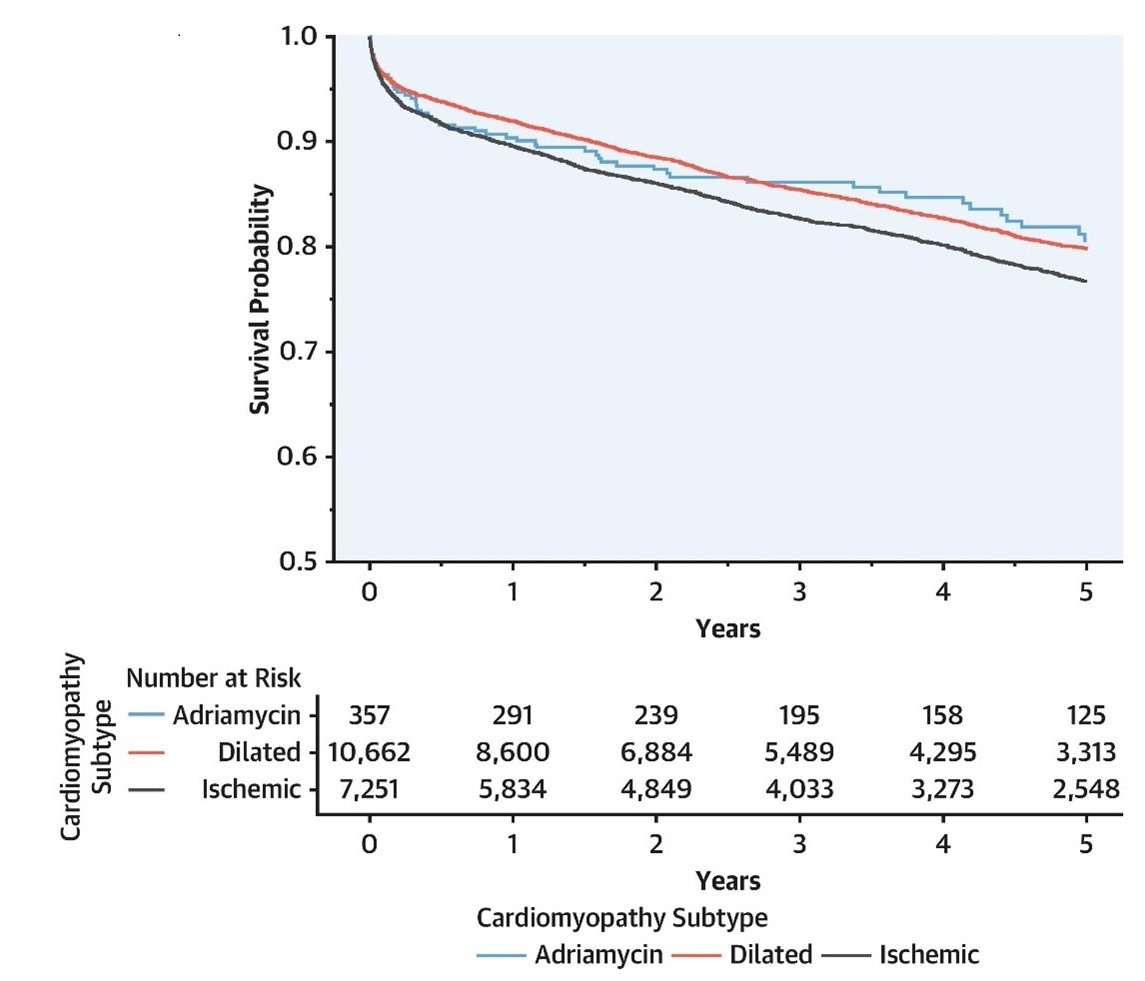
The study cohort included 18,270 patients who underwent cardiac transplantation between October 18, 2008, and October 18, 2018 (adriamycin-associated cardiomyopathy: 357; dilated cardiomyopathy: 10,662; ischemic cardiomyopathy: 7,251). Compared to patients in the dilated cardiomyopathy and ischemic cardiomyopathy cohorts, patients with adriamycin-associated cardiomyopathy were younger and more likely to be female and had lower rates of diabetes and lower body mass indices. They also had higher PVR and slightly longer ischemic times and were less likely to have a male recipient with a female donor. Despite the higher PVR, they underwent fewer bridge-to-transplant LVADs, although they had a similar degree of temporary support at the time of transplant (Figure 1).
Figure 1: Kaplan-Meier Survival After Cardiac Transplantation by Cardiomyopathy Subtype
In the multivariable analysis, patients with adriamycin-associated cardiomyopathy did not experience an increase in post-cardiac-transplant mortality compared to those with dilated cardiomyopathy (adjusted hazard ratio [HR] 0.96; 95% confidence interval [CI], 0.79-1.40; p = 0.764) or ischemic cardiomyopathy (adjusted HR 0.85; 95% CI, 0.60-1.20; p = 0.304). When limiting the multivariable analysis to patients who did not have an LVAD at the time of transplant, adriamycin-associated cardiomyopathy was not associated with increased post-transplant mortality (adriamycin-associated cardiomyopathy vs. dilated cardiomyopathy: adjusted HR 1.08; 95% CI, 0.80-1.50; p = 0.651; adriamycin-associated cardiomyopathy vs. ischemic cardiomyopathy: adjusted HR 0.97; 95% CI, 0.70-1.40; p = 0.884). In sensitivity analyses excluding patients who had prior cancer history in the dilated cardiomyopathy (6.7%) and ischemic cardiomyopathy groups (6.9%), adriamycin-associated cardiomyopathy was not associated with statistically increased post-transplant mortality (adriamycin-associated cardiomyopathy vs. dilated cardiomyopathy: adjusted HR 1.04; 95% CI, 0.78-1.40; p = 0.775; adriamycin-associated cardiomyopathy vs. ischemic cardiomyopathy: adjusted HR 1.15; 95% CI, 0.85-1.55; p = 0.369).
The percentage of deaths by cause at each timepoint (30 days, 1 year, 3 years, and 5 years) within each cardiomyopathy subgroup were noted. The adriamycin-associated cardiomyopathy group had a higher percentage of deaths that were cardiovascular related (adriamycin-associated cardiomyopathy: 30.8%; dilated cardiomyopathy: 12.7%; ischemic cardiomyopathy: 13.4%) and stroke related (adriamycin-associated cardiomyopathy: 23.1%; dilated cardiomyopathy: 8.7%; ischemic cardiomyopathy: 7.0%) at 30 days. At the 1-year, 3-year, and 5-year timepoints, death from graft failure was higher in the dilated cardiomyopathy and ischemic cardiomyopathy groups.
Perspective
This study adds to previous published reports2,3 by demonstrating the safety of heart transplantation in patients with adriamycin-associated cardiomyopathy in the contemporary era of advanced heart failure therapies.4 Patients with adriamycin-associated cardiomyopathy received fewer bridge-to-transplant LVADs despite an overall increase in LVAD use during the study period. Further studies are needed to evaluate the impact of conventional and newer cancer therapies on outcomes of patients with end-stage heart failure.
References
- Ramu B, Masotti M, Tedford RJ, Cogswell RJ. Heart Transplantation in Adriamycin-Associated Cardiomyopathy in the Contemporary Era of Advanced Heart Failure Therapies. JACC CardioOncol 2021;3:294-301.
- Lenneman AJ, Wang L, Wigger M, et al. Heart transplant survival outcomes for adriamycin-dilated cardiomyopathy. Am J Cardiol 2013;111:609-12.
- Oliveira GH, Hardaway BW, Kucheryavaya AY, Stehlik J, Edwards LB, Taylor DO. Characteristics and survival of patients with chemotherapy-induced cardiomyopathy undergoing heart transplantation. J Heart Lung Transplant 2012;31:805-10.
- Kittleson MM. Heart Transplantation for Adriamycin Cardiomyopathy: The Plural of Anecdote and the Power of Registries. JACC CardioOncol 2021;3:302-4.
Clinical Topics: Cardiac Surgery, Cardio-Oncology, Congenital Heart Disease and Pediatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Valvular Heart Disease, Aortic Surgery, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Acute Heart Failure, Heart Transplant, Mechanical Circulatory Support, Interventions and Structural Heart Disease
Keywords: Heart-Assist Devices, Cardiomyopathy, Dilated, Cardiomyopathy, Restrictive, Doxorubicin, Follow-Up Studies, Confidence Intervals, Neoplasms, Biometry, Heart Transplantation, Heart Failure, Myocardial Ischemia, Cardiomyopathy, Hypertrophic, Heart Defects, Congenital, Heart Valve Diseases, Diabetes Mellitus, Stroke
< Back to Listings