New Evidence Supporting Selective Use of Coronary Artery Calcium Scoring for Adults at Borderline 10-Year ASCVD Risk
Quick Takes
- CAC scoring significantly improves risk stratification in the borderline risk (5% to <7.5%) group.
- About one third of adults with borderline risk had CAC = 0, while about a quarter had at least moderate CAC.
- CAC testing can facilitate shared decision making in the important group of borderline risk patients.
Commentary based on Uddin SMI, Osei AD, Obisesan O, et al. Coronary artery calcium scoring for adults at borderline 10-year ASCVD risk: the CAC Consortium. J Am Coll Cardiol 2021;78:537-38.1
Introduction
The 2018 American Heart Association/American College of Cardiology/Multisociety (AHA/ACC/MS) guideline on blood cholesterol management recommends using the pooled cohort equations (PCE) to estimate 10-year atherosclerotic cardiovascular disease (ASCVD) risk in patients aged 40-75 years without diabetes and an LDL-C level of 70-189 mg/dL for primary ASCVD prevention.2 According to the guideline, the 10- year ASCVD risk is categorized as low risk (<5%), borderline risk (5% to <7.5%), intermediate risk (7.5% to <20%), and high risk (≥20%).
Coronary artery calcium (CAC) scoring has emerged as a highly specific marker for atherosclerotic plaque burden and is a widely available and cost-effective tool for CV risk classification.3,4 CAC measurements significantly improve risk classification for ASCVD events among statin recommended (intermediate risk) individuals from the Multi-Ethnic Study of Atherosclerosis (MESA) study with about 40% of individuals with a CAC score of 0 having their risk category down-classified.5 The 2018 AHA/ACC/MS guideline recommended CAC scoring only in "selected" borderline risk adults with risk-enhancing factors to aid in decision making regarding statin therapy.2 The recent study by Uddin et al. tested the clinical utility of CAC in guide-based ASCVD risk stratification among adults classified as borderline risk over the next decade.1
Methods
The authors included 8,854 adults aged 40-75 years free of clinical CVD with a 10-year ASCVD risk of 5% to 7.5% from the CAC Consortium, a retrospective multicenter clinical cohort.1,4 Participants were categorized into three CAC score groups: CAC = 0, CAC 1-99 and CAC ≥100.
The associations between CAC and CVD and coronary heart disease (CHD) mortality were examined using Cox proportional-hazards regression models adjusting for traditional risk factors. The incremental predictive value of CAC beyond traditional CV risk factors was assessed using categorical net reclassification index (NRI) analyses using cut points of 0.53% and 1.18% for CVD mortality and 0.22% and 0.58% for CHD mortality. Area under curve (AUC) analyses were performed from fully adjusted logistic regression models, with and without CAC.
Study Results
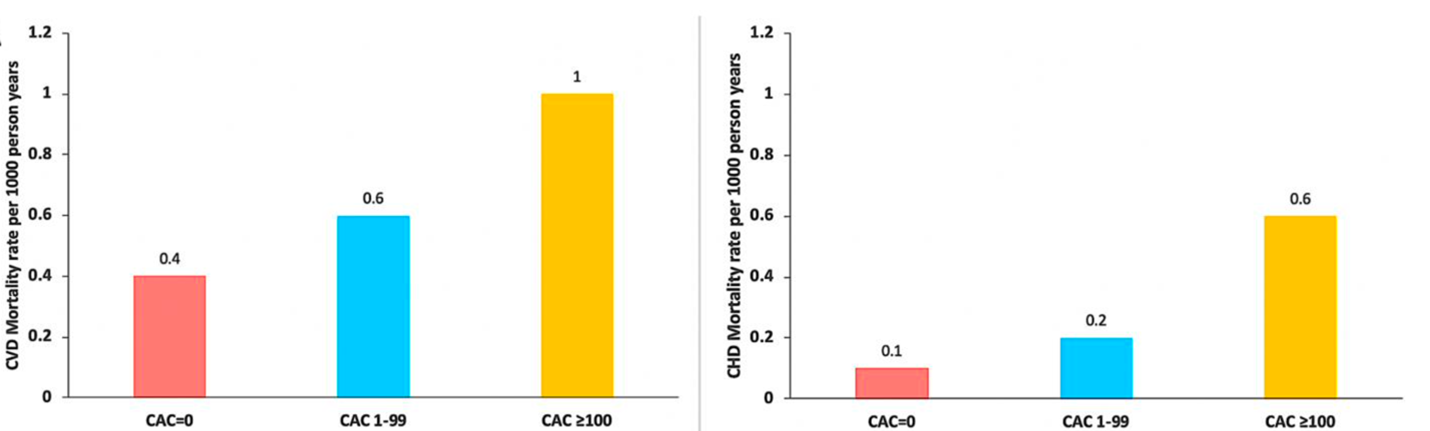
A wide heterogeneity of CAC scores was noted among the borderline risk adults. About 35% of adults with borderline risk had CAC = 0, 38% had CAC 1-99, and 27% CAC ≥100. Higher CVD and CHD death rates were observed in adults with higher CAC scores, and a similar pattern was observed in sex-stratified analysis. Addition of CAC showed significant improvement in NRI calculations.
CAC reclassified many participants; about 26% with CVD deaths were reclassified to higher and 13% to lower risk. In participants with no CVD deaths, 15% were reclassified to higher and 23% to lower risk. In those with CHD deaths, 34% were reclassified to higher and 16% to lower risk, and in participants with no CHD death, 18% were reclassified higher and 33% to lower risk. The addition of CAC to the fully adjusted model improved the AUC for CVD and CHD deaths compared to those without CAC – 0.69 versus 0.65 and 0.69 versus 0.61 for CVD and CHD deaths, respectively.
Summary and Future Directions
In a multicenter cohort of individuals free of baseline CVD, CAC scoring significantly improved risk stratification in individuals identified as borderline risk (5% to <7.5%) according to the 2018 AHA/ACC/MS guideline. CAC scoring differentiated high versus low risk for CVD and CHD mortality. About one third of the participants had CAC = 0 and had the lowest CVD and CHD mortality rates, thus, identifying individuals who likely do not need to start a statin at that point in time.
A provocative 2018 study by Mitchell6 showed no reduction in the risk of major adverse cardiovascular events with statin therapy in patients with CAC = 0 over a mean follow-up of 10 years. In addition, a 2019 study published in Circulation7 demonstrated that CAC may be a valuable tool for aspirin allocation in primary prevention. The recent study by Uddin et al. adds further evidence supporting the use of CAC testing in optimizing shared decision making, incorporating patient preferences, values, and concerns about potential adverse effects.
Recently, the National Lipid Association8 provided updates on the evidence-based optimal use of CAC scoring and made recommendations for use of CAC scoring in primary prevention treatment decision making. The guideline recommends CAC scoring to aid clinicians in determining the need for and the intensity of preventive therapies in borderline to intermediate risk adults. Recommendations for the selective use of CAC scoring were also provided for those with diabetes, metabolic syndrome, severe hypercholesterolemia, and in those taking statins, including recommendations for its use in allocation of aspirin and anti-hypertensive therapy.
These findings have important implications in terms of making treatment decisions in the borderline risk group (5% to <7.5%) and in helping identify patients who will most likely benefit from statin therapy in primary prevention. The information from a CAC scan can inform the clinician-patient risk discussion in the large group of borderline-risk patients. It supports the concept that selective use of CAC to improve risk reclassification as part of shared decision make in the large segment of adults who have a 5-20% 10-year estimated risk of an ASCVD event.
Figure 1: Absolute Event Rates for CVD and CHD mortality among adults with ASCVD risk. Courtesy of Rajan T, Blumenthal RS, Dzaye O.
References
- Uddin SMI, Osei AD, Obisesan O, et al. Coronary artery calcium scoring for adults at borderline 10-year ASCVD risk: the CAC Consortium. J Am Coll Cardiol 2021;78:537-38.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:e285-e350.
- Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol 2018;72:434-47.
- Blaha MJ, Whelton SP, Al Rifai M, et al. Rationale and design of the coronary artery calcium consortium: a multicenter cohort study. J Cardiovasc Comput Tomogr 2017;11:54-61.
- Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines. J Am Coll Cardiol 2015;66:1657-68.
- Mitchell JD, Fergestrom N, Gage BF, et al. Impact of statins on cardiovascular outcomes following coronary artery calcium scoring. J Am Coll Cardiol 2018;72:3233-42.
- Cainzos-Achirica M, Miedema MD, McEvoy JW, et al. Coronary artery calcium for personalized allocation of aspirin in primary prevention of cardiovascular disease in 2019: the MESA Study (Multi-Ethnic Study of Atherosclerosis). Circulation 2020;141:1541-53.
- Orringer CE, Blaha MJ, Blankstein R, et al. The National Lipid Association scientific statement on coronary artery calcium scoring to guide preventive strategies for ASCVD risk reduction. J Clin Lipidol 2021;15:33-60.
Clinical Topics: Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Homozygous Familial Hypercholesterolemia, Lipid Metabolism, Nonstatins, Novel Agents, Statins
Keywords: Hydroxymethylglutaryl-CoA Reductase Inhibitors, Hypercholesterolemia, Area Under Curve, Calcium, Antihypertensive Agents, Cholesterol, LDL, Plaque, Atherosclerotic, Retrospective Studies, Logistic Models, American Heart Association, Metabolic Syndrome, Coronary Vessels, Aspirin, Cardiovascular Diseases, Cost-Benefit Analysis, Patient Preference, Decision Making, Shared, Follow-Up Studies, Risk Factors, Diabetes Mellitus, Atherosclerosis, Coronary Disease, Primary Prevention, Cardiology, Decision Making, Risk Assessment, Resource Allocation
< Back to Listings