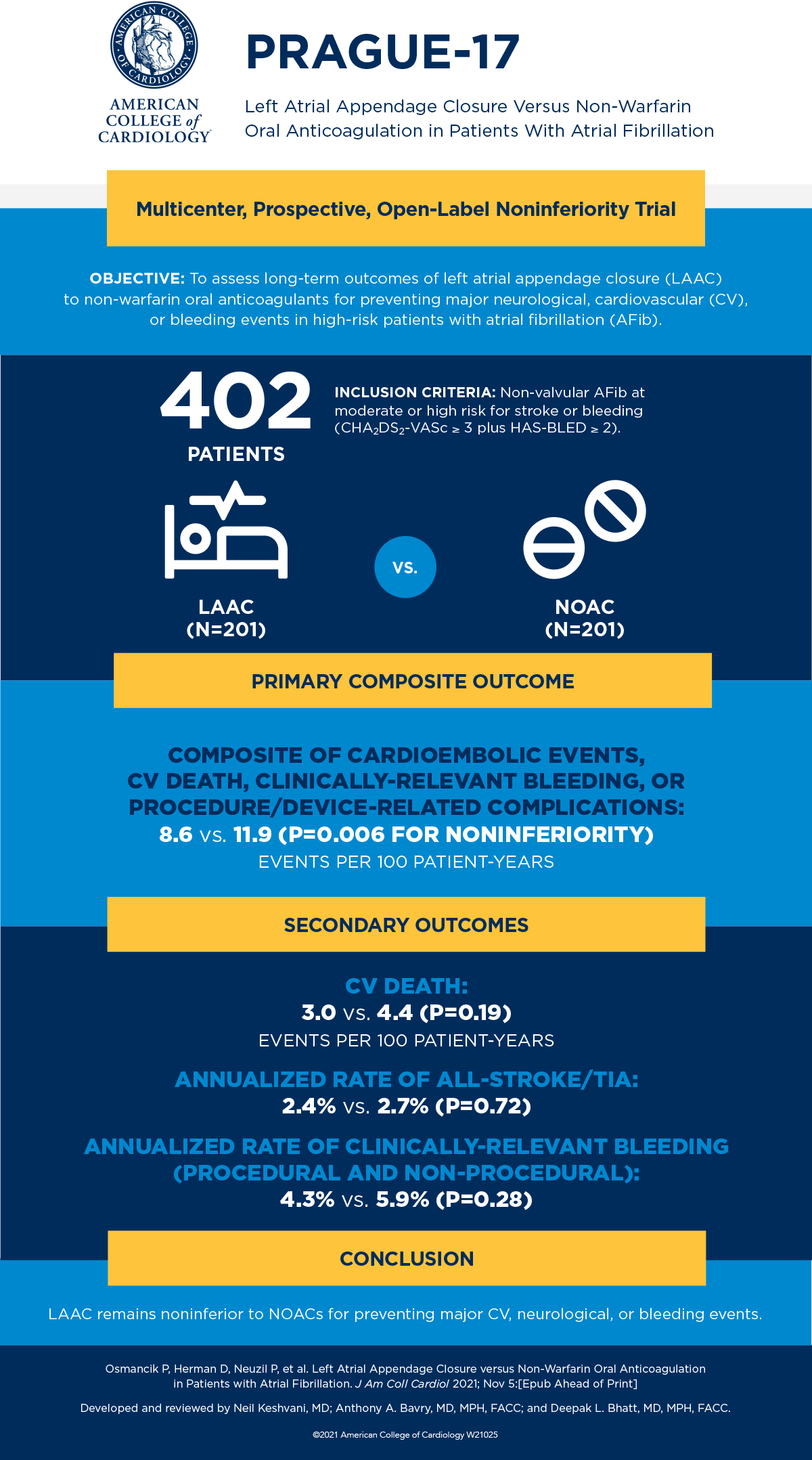
PRAGUE-17: LAAC Noninferior to NOACs For Major AFib-Related CV, Neurological Events Longer-Term
Left atrial appendage closure (LAAC) was noninferior to non-warfarin oral anticoagulants (NOAC) for major atrial fibrillation (AFib)-related cardiovascular or neurological events, based on pre-specified long-term outcomes from the PRAGUE-17 trial presented Nov. 5 during TCT 2021 and simultaneously published in the Journal of the American College of Cardiology. LAAC was also associated with less post-procedural bleeding.
Researchers, led by Pavel Osmancik, MD, PhD, randomized 402 patients with non-valvular AFib and a history of cardioembolism, clinically-relevant bleeding, or both CHA2DS2-VASc > 3 and HASBLED > 2 to either LAAC (n=201) or NOAC (n=201). The median age was 73 years and 65.7% were male. Median follow-up time was 3.5 years. The primary endpoint was a composite of cardioembolic events (stroke, transient ischemic attack, or systemic embolism), cardiovascular death, clinically-relevant bleeding or procedure/device-related complications (LAAC group only). The primary analysis was modified intention-to-treat (mITT).
Overall results found LAAC was non-inferior to NOACs for the primary endpoint (sHR 0.81, 95% CI 0.56-1.18; p=0.27; p for non-inferiority=0.006). Non-procedural clinically-relevant bleeding was reduced with LAAC (sHR 0.55, 95% CI 0.31-0.97; p=0.039). Researchers noted that the curves of clinically-relevant bleeding appeared to separate at approximately six months.
“Among non-valvular patients with AFib and at high risk for stroke and bleeding, the non-inferiority of LAAC to NOAC relative to the composite of cardioembolic events, [cardiovascular] death, significant procedure/device-related complications, or clinically-relevant bleeding, was maintained during long-term follow-up,” the researchers said. “The rate of non-procedural clinically-relevant bleeding was significantly reduced with LAAC compared with NOAC therapy, but the study was underpowered to detect differences in stroke rate.”
In a related editorial comment, Faisal M. Merchant, MD, FACC, raises the question of whether percutaneous LAAC can “stand the test of time.” He writes: “Given the large number of patients with AFib who merit stroke prevention therapy, it is incumbent upon us to really understand which therapies are most effective at preventing the endpoints which are most important to patients. But until such data are available, the longer-term results from PRAGUE-17 provide an important perspective on the challenges of evaluating late risks associated with [stroke/systemic embolism] and bleeding in patients with AFib.”
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Invasive Cardiovascular Angiography and Intervention, Anticoagulation Management and Atrial Fibrillation, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Interventions and Imaging, Angiography, Nuclear Imaging
Keywords: Transcatheter Cardiovascular Therapeutics, TCT21, Atrial Fibrillation, Atrial Appendage, Cardiac Surgical Procedures, Anticoagulants, Angiography
< Back to Listings