Poll Results: Falls in Older Adults with Cardiovascular Diseases: Yup, It's a Thing!
Mr. P is a 73-year-old male with history of Parkinson's disease diagnosed within the past 1-2 years. He presented to a hospital after a ground-level fall that resulted in a small subdural hematoma.
The geriatric consult service was contacted the morning after admission for recommendations regarding routine geriatric care post-trauma. The geriatric team recommended cardiology consultation for discussion of a patient-centered management plan and recommendations for an optimal blood pressure range that would address his Parkinson's disease, frequent falls, heart failure, and low blood pressures.
Click here for original clinical vignette.
The answers to two poll questions based on the clinical vignette are noted below:
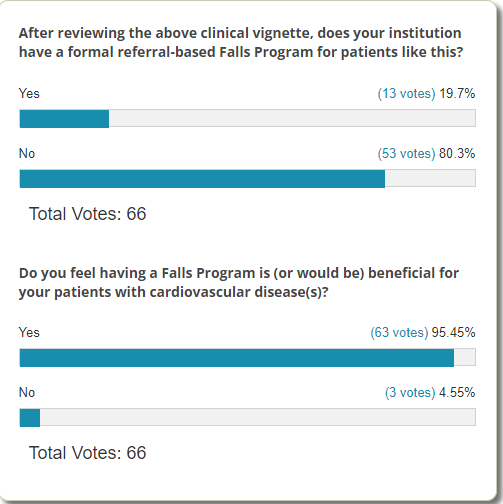
The results of this ACC.org poll, on a topic that is not commonly addressed by the clinical cardiovascular team, clearly recognizes the necessity of increasing individual knowledge and having an institutional-level Falls Program.
The Prevention of Falls Network Europe definition of a fall is: ''an unexpected event in which the participants come to rest on the ground, floor, or lower level".1
This is a simple definition that addresses the reality of often not knowing whether the patient did or didn't lose consciousness (true for unwitnessed falls and falls in someone with cognitive impairment). The caveat is that investigation is still needed for ascertainment of the etiology of the fall, assessing the presence or absence of loss of consciousness/syncope, and working up the underlying cause.
The cardiovascular clinical team is sometimes consulted to assess falls in older adults and should be cognizant of current knowledge and available tools to contribute to the discussion and management. In general, risk factors for falls are categorized as intrinsic (e.g., decreased vision, cognitive deficits, multiple chronic conditions, individual illnesses, abnormal gait or balance, sarcopenia), extrinsic (polypharmacy), and environmental (e.g., home hazards such as loose rugs, stairs, or poor lighting).2
Common domain assessments, strategies and possible interventions are shown below:3
- Domain – Balance, gait and strength
- Strategies -Watch patient walk into the clinic, rise from a chair (unassisted, without using arms to push off). Consider a Short Physical Performance Battery test.4
- Possible interventions
- Consider referral to physical therapy for gait and stability evaluation.
- Simple home-based exercise for leg-strengthening and balance can be prescribed.
- Go4Life From The National Institute On Aging
- NIH/Prevent Falls and Fractures
- Strategies -Watch patient walk into the clinic, rise from a chair (unassisted, without using arms to push off). Consider a Short Physical Performance Battery test.4
- Domain – Vision
- Strategy – Ask patient whether an eye examination was performed in the past 1-2 years.
- Intervention - Consider referral to optometry and/or ophthalmology.
- Strategy – Ask patient whether an eye examination was performed in the past 1-2 years.
- Domain(s) – Orthostatic hypotension (OH) & hypotension
- Strategy – Obtain orthostatic vital signs.
- Possible interventions
- Taper or discontinue medications that contribute to OH or hypotension (see medications domain).
- Pharmacological treatment in severe cases of OH.
- Strategy – Obtain orthostatic vital signs.
- Domain – Medications
- Strategy – Assess for potentially inappropriate medications based on underlying patient clinical status. In particular, recognize harms of cardiovascular medications in general5 and particularly for falls;6 assess balance of benefits and harms for cardiovascular and non-cardiovascular medications;7 recognize lower blood pressure goals decrease major adverse cardiovascular events (MACE) but increase serious adverse events (SAE).8
- Intervention(s) – In patients with multiple geriatric conditions, have a shared decision-making discussion of the optimal blood pressure goal based on potential MACE reduction and SAE increase. Review goals periodically and adjust treatment plan based on review.
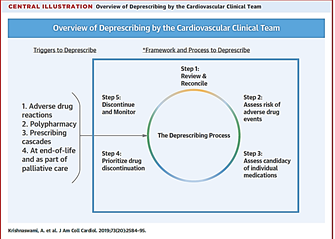
- Consider triggers to deprescribe and initiate deprescribing if indicated.5
- Of note, vitamin D to specifically target fall prevention is not recommended.3
- Domain – Environment
- Strategies – Assess basic and instrumental activities of daily living. Consider home safety evaluation.
- Intervention(s) – Home modification and equipment adaptation
- Strategies – Assess basic and instrumental activities of daily living. Consider home safety evaluation.
- Domain – Cognitive and psychological health
- Strategies – Consider cognition (including delirium) and depression screening tools (Confusion Assessment Method, Mini-Cog, Patient Health Questionnaire-92).
- Intervention(s) – Consider referral to primary care physician for concerns regarding depression and cognition.
References
- Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc 2005;53:1618-22.
- Reuben DB, Herr, KA, Pacala JT, Pollock BG, Potter JF, Semla TP, eds. Geriatrics At Your Fingertips. 23rd Edition. New York: The American Geriatrics Society; 2021; 2021.
- Ganz DA, Latham NK. Prevention of falls in community-dwelling older adults. N Engl J Med 2020;382:734-43.
- Afilalo J, Alexander KP, Mack MJ, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol 2014;63:747-62.
- Paradissis C, Cottrell N, Coombes I, Scott I, Wang W, Barras M. Patient harm from cardiovascular medications. Ther Adv Drug Saf 2021;12:20420986211027451.
- de Vries M, Seppala LJ, Daams JG, van de Glind EMM, Masud T, van der Velde N. Fall risk-increasing drugs: a systematic review and meta-analysis: I. cardiovascular drugs. J Am Med Dir Assoc 2018;19:371.e1-e9.
- Krishnaswami A, Steinman MA, Goyal P, et al. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol 2019;73:2584-95.
- Krishnaswami A, Peterson ED, Kim DH, Goyal P, Rich MW. Efficacy and safety of intensive blood pressure therapy using restricted mean survival time-insights from the SPRINT trial. Am J Med 2020;133:e369-e70.
Clinical Topics: Cardiovascular Care Team, Heart Failure and Cardiomyopathies, Vascular Medicine, Acute Heart Failure, Geriatric Cardiology
Keywords: Activities of Daily Living, Goals, Accidental Falls, Hypotension, Orthostatic, Cardiovascular Diseases, Blood Pressure, Multiple Chronic Conditions, National Institute on Aging (U.S.), Ophthalmology, Parkinson Disease, Physicians, Primary Care, Polypharmacy, Potentially Inappropriate Medication List, Sarcopenia, Risk Factors, Cognitive Dysfunction, Physical Functional Performance, Hematoma, Subdural, Patient-Centered Care, Physical Therapy Modalities, Heart Failure, Hospitals, Mental Status and Dementia Tests, Syncope
< Back to Listings