Poll Results: Baseline Diagnostic Angiography in STEMI
Questions recently arose regarding how can or should physicians document preexisting heart failure prior to Primary percutaneous coronary intervention (PCI) in a ST-elevation myocardial infarction (STEMI) to avoid heart failure being documented post procedure and appearing to be a consequence of the procedure.
Significant variation in the approach to angiography prior to Primary PCI for STEMI has been noted in the past1 but preferences have not been analyzed recently. This poll was undertaken for a relook at practices related to the approach to angiography and ventriculography prior to Primary PCI.
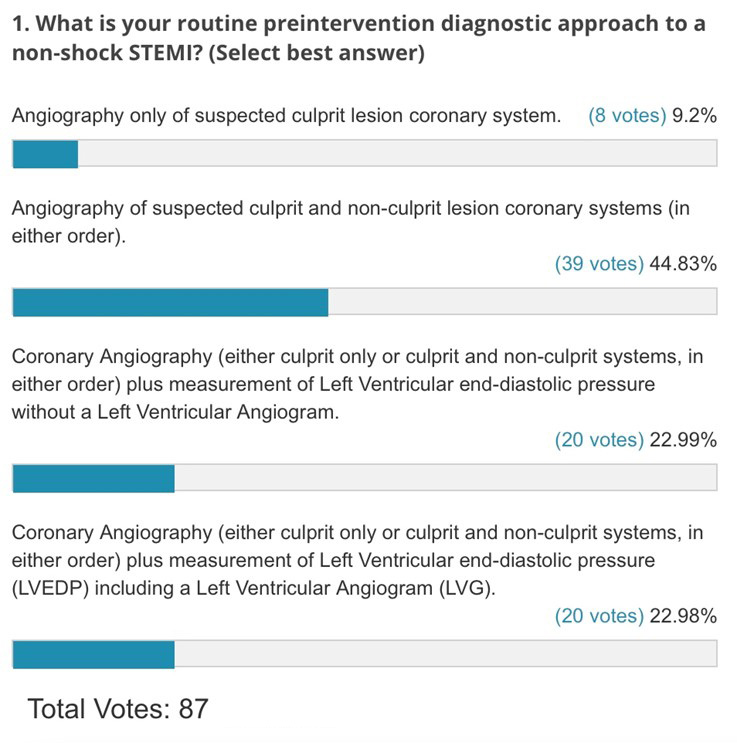
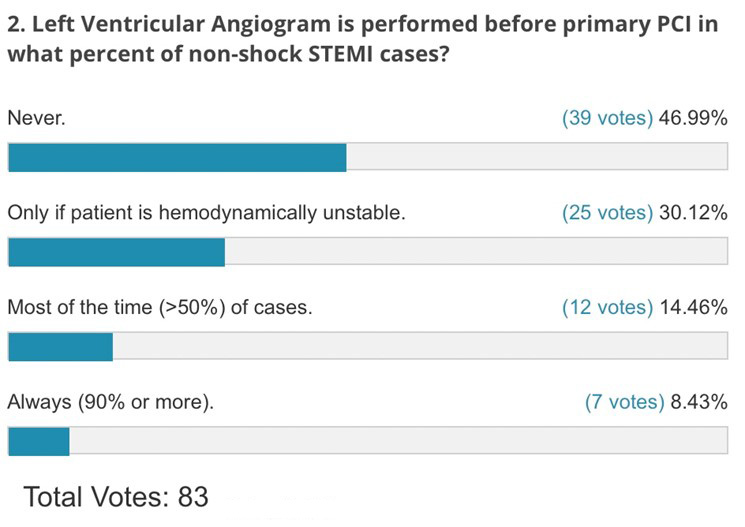
The results are below:
Summary of Results:
- It is important to note that these results focus on management of patients not thought to be in shock at the time of angiography before the Primary PCI procedure.
- The results demonstrate significant variation in the approach to angiography and invasive assessment of left ventricular function.
- Only 10% of operators perform culprit only angiography for the suspected infarct artery prior to PCI.
- Nearly half of operators perform PCI without ventriculography with less than a quarter measuring ventricular pressure without ventriculography while less than a quarter perform a ventriculogram.
- Nearly one-half of operators never perform a ventriculogram while 30% do so based on hemodynamic instability.
- Approximately one-third of operators perform ventriculography all or most of the time.
Compared to a survey by the Society for Cardiovascular Angiography and Interventions (SCAI) nearly 10 years ago, variation persists with similar areas of discordance between operators. In the prior survey1 58% of respondents visualized the non-culprit artery prior to PCI including using a diagnostic catheter for both the culprit and non-culprit systems by an additional 23% of respondents. Only 19% went directly with a guide catheter for the culprit artery to perform Primary PCI prior to angiography of the contralateral, non-culprit artery. Regards ventriculography, only 9% performed left ventriculography prior to PCI, but interestingly 66% performed ventriculography at some time. Only 25% reported rare or no use of left ventriculography. Thus, it appears that ventriculography use has declined over time, likely in part as an opportunity to reduce contrast burden as well as relying on echo assessment of left ventricular function post revascularization.
While these results represent reasonable clinical management, they do not offer the opportunity to systematically assess baseline severity of left ventricular function with an opportunity to assess baseline dysfunction and relative improvement or deterioration post revascularization.
References
- Chiang A, Gada H, Kodali SK, et al. Procedural variation in the performance of primary percutaneous coronary intervention for ST-elevation myocardial infarction: a SCAI-based survey study of US interventional cardiologists. Catheter Cardiovasc Interv 2014;83:721-26.
Clinical Topics: Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Stable Ischemic Heart Disease, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Acute Heart Failure, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Chronic Angina
Keywords: ST Elevation Myocardial Infarction, Percutaneous Coronary Intervention, Ventricular Function, Left, Ventricular Pressure, Surveys and Questionnaires, Heart Failure, Angiography, Catheters, Arteries, Myocardial Infarction, Coronary Artery Disease
< Back to Listings
