We Need a Bigger Tent: Expanding the Reach and Coverage of Training in Advanced Heart Failure
Quick Takes
- There is an increasing demand for heart failure specialists, but the number of fellows applying into Advanced Heart Failure and Transplant Cardiology (AHFTC) training programs is declining.
- De-centering AHFTC training from heart replacement therapies and expanding the breadth of the curriculum to cover the growing needs of the heart failure field may attract more trainees to the field.
- Exposing trainees early and often to the breadth and depth of career opportunities and mentors under the tent of heart failure will help grow the heart failure workforce.
In 2008, the American Board of Internal Medicine's (ABIM) proposal to recognize Advanced Heart Failure and Transplant Cardiology (AHFTC) as a cardiovascular (CV) subspecialty was approved. Five years later, the Accreditation Council for Graduate Medical Education formally acknowledged the specific skills and knowledge required to care for patients with advanced heart failure (HF).1 Since then, AHFTC has experienced tremendous growth with regard to diagnostics and therapeutics relevant to the care of patients with HF. Despite this rapid innovation, patients with HF remain underrecognized and undertreated — from missed opportunities for HF prevention to delayed initiation of guideline-directed medical therapy and referrals for advanced therapies.2,3 Moreover, the burden of HF in the United States (US) continues to grow; over eight million Americans are projected to have HF by 2030.4 As such, AHFTC specialists are in high demand; however, the number of AHFTC fellowship matriculants is declining, with an increasing number of unfilled positions each cycle.5 Strategies to address this disconnect between the supply of and demand for a well-trained AHFTC workforce are urgently needed.
Barrier: Lack of Exposure to AHFTC Careers
A 2018 survey of CV fellowship program directors provided insight into general fellows' lack of exposure to AHFTC careers.6 Of the 130 program directors who responded, approximately 40% reported lacking program expertise in cardiac transplantation, and about 30% reported lacking expertise in both ventricular assist devices and pulmonary hypertension. Strikingly, 62% did not have subspecialty AHFTC training programs at their institutions. As the majority of programs represented in this survey are unable to provide AHFTC exposure to their trainees, alternative educational experiences to ensure that trainees meet at least COCATS 4 Level I competency in AHFTC should be more widely explored. One such successful partnership in Tennessee was described by Dr. JoAnn Lindenfeld et al. in 2017.7 In this initiative, the AHFTC program at Vanderbilt University Medical Center hosted three rotating fellows from East Tennessee State University, which has a CV fellowship training program without co-localized AHFTC training. The visiting fellows reviewed the rotation experience very positively and endorsed that their clinical skills and knowledge related to AHFTC significantly improved as a result of the rotation.
Barrier: Overemphasis on Heart Replacement Therapies in Training
For general trainees on AHFTC rotations, the early evaluation and management of patients with Stages A-C HF is often outshone by the allure of cardiac transplantation and mechanical circulatory support (MCS). Trainees may consider AHFTC fellowship because of interests in other aspects of HF but may be deterred by the focus on heart replacement therapies. Additionally, trainees perceive a saturated job market with a majority of available AHFTC positions in any given year at academic MCS/transplant centers. Fear of job insecurity or dissatisfaction after many years of postgraduate training is a relevant consideration.
Opportunity: Expand AHFTC Curriculum Beyond MCS and Transplantation
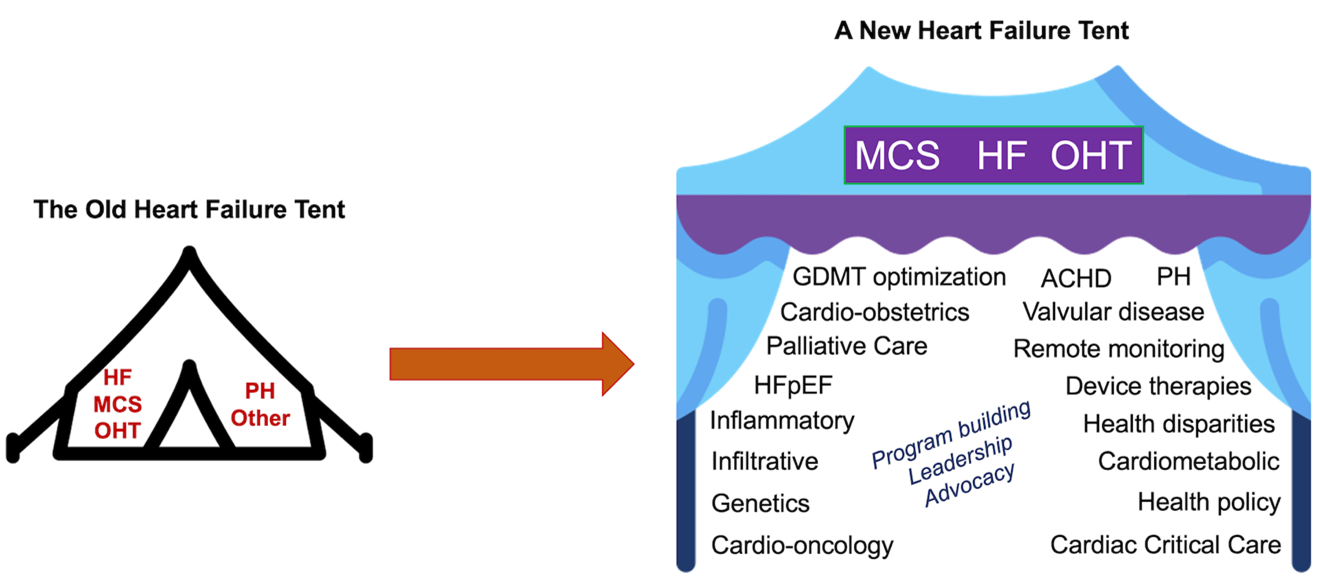
Broadening the AHFTC curriculum beyond transplantation and MCS offers opportunities to nurture clinicians equipped to address the emerging clinical needs in genetics, cardio-oncology, cardio-obstetrics, cardiac critical care, cardiometabolic disorders, invasive HF, pulmonary hypertension, adult congenital heart disease, valvular disease, device therapies, health disparities, and palliative care. Accomplishing this may require de-centering AHFTC training from transplantation and MCS management but may ultimately attract more trainees to the field by expanding the coverage of the ambulatory curriculum to address these growing needs (Figure 1).
Figure 1: The Need for a Bigger Heart Failure Tent
Abbreviations: ACHD, Adult Congenital Heart Disease; GDMT, Guideline-directed Medical Therapy; HF, Heart Failure; HFpEF, Heart Failure with Preserved Ejection Fraction; MCS, Mechanical Circulatory Support; OHT, Orthotopic Heart Transplant; PH, Pulmonary Hypertension.
Opportunity: Encourage Personalized AHFTC Training
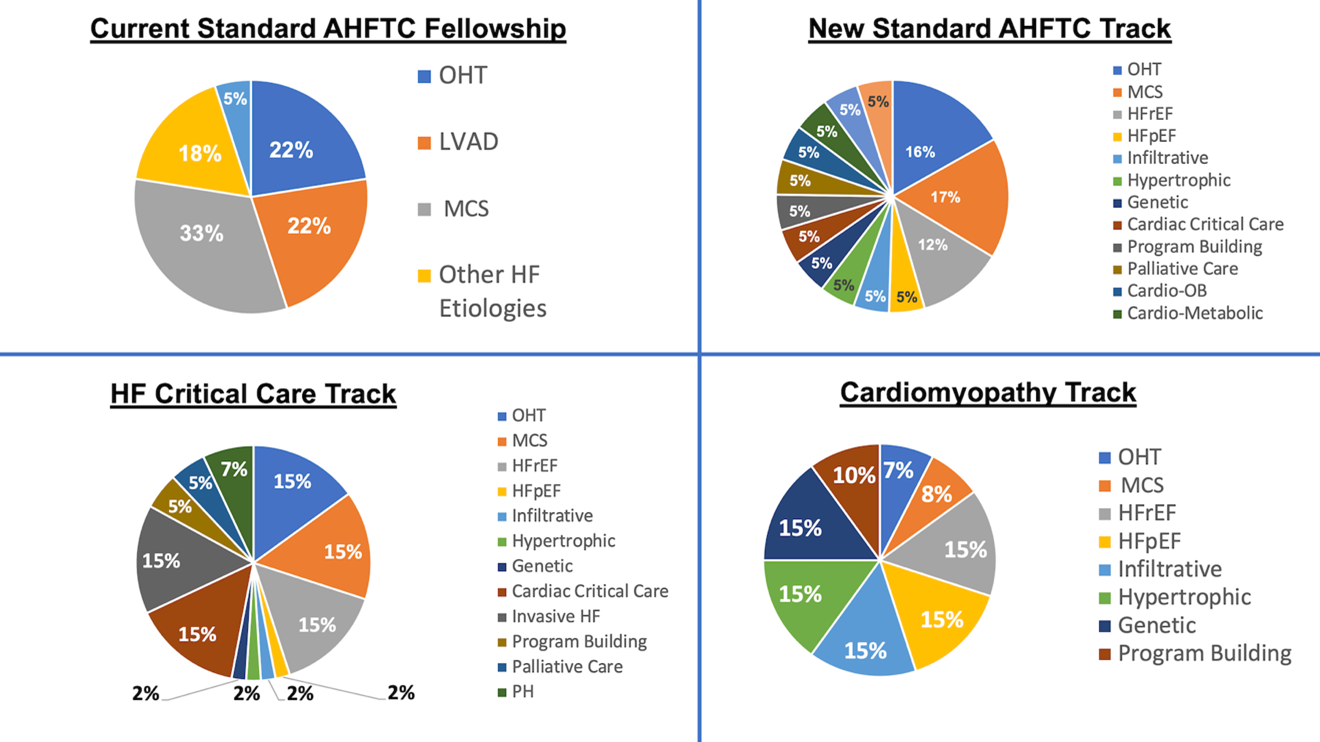
One year of AHFTC fellowship may not provide adequate time to acquire wide-ranging proficiency, and every AHFTC training program may not excel at each subspecialty. One potential solution is to allow elective time during the third year of CV fellowship to focus on a trainee's area of interest. Opportunities to acknowledge this dedicated training, similar to COCATS Level II certification without an additional ABIM certification exam, has been recently discussed in the context of cardiac critical care and invasive HF.3,8-12 Similarly, for those completing AHFTC training at a different institution, trainees and program directors could collaborate to match trainees' specific career interests with programmatic strengths. Programs could subsequently develop personalized curricula while ensuring that the foundational AHFTC curriculum remains. Separate tracks will allow trainees to hone skills in a few specific areas of HF that best serve their clinical and research interests (Figure 2).
Figure 2: Example Changes to the AHFTC Curriculum to Incorporate New Personalized Tracks
Abbreviations: AHFTC, Advanced Heart Failure and Transplant Cardiology; Cardio-OB, Cardio-Obstetrics; HF, Heart Failure; HFpEF, Heart Failure with Preserved Ejection Fraction; HFrEF, Heart Failure with Reduced Ejection Fraction; MCS, Mechanical Circulatory Support; OHT, Orthotopic Heart Transplant; PH, Pulmonary Hypertension.
Opportunity: Incorporate Education on Program Building, In-reach, and Outreach
In addition to broadening the AHFTC curriculum, a focus on program building is needed to prepare trainees for the changing career landscape. Many tertiary and quaternary HF centers serve as the "hub" in a "hub-and-spoke" model for needs ranging from cardiogenic shock and advanced HF therapy referrals to long-term transplant and MCS management.13 Many new AHFTC graduates take positions at "spoke" hospitals, with expectations to establish or grow HF programs in remote monitoring, medication titration, or disease-specific clinics. Additionally, these positions often include in-reach – educating practitioners within their health systems on appropriate HF treatment options and referral strategies. Traditional AHFTC fellowship paradigms do not adequately provide training in-program development. Incorporating dedicated didactics on practice development and inclusion of trainees into ongoing program-building efforts at training centers are strategies to address this shortcoming. For the more clinically focused trainees, a program-building project could be done in lieu of more traditional research, which would benefit both the trainee, the training center, and the future practice in which the trainee is employed.
Opportunity: Diversify the AHFTC Workforce
A diverse clinician workforce has been shown to improve clinical care and research efforts for historically underserved populations, who have higher HF-related mortality.14,15 In 2021, the proportion of AHFTC fellowship applicants who self-identified as Black/African American or Hispanic/Latino/of Spanish Origin was just 10.5%, and no applicants identified as American Indian or Alaska Native or Native Hawaiian or Other Pacific Islander.16 Strategies to recruit a diverse workforce, from medical school to subspecialty and faculty positions, have been previously discussed.15,17 Open and honest discussions on work-life integration in AHFTC, including family planning, for trainees of all genders and sexual orientations is imperative to the field's growth.5
Open-minded and visionary leadership is critical to expanding the HF tent. Welcoming trainees to the diverse career opportunities in AHFTC will grow the HF workforce and ultimately better serve and shelter our widely diverse patients.
References
- Jessup M, Drazner MH, Book W, et al. 2017 ACC/AHA/HFSA/ISHLT/ACP advanced training statement on advanced heart failure and transplant cardiology (revision of the ACCF/AHA/ACP/HFSA/ISHLT 2010 clinical competence statement on management of patients with advanced heart failure and cardiac transplant): a report of the ACC Competency Management Committee. J Am Coll Cardiol 2017;69:2977-3001.
- Morris AA, Khazanie P, Drazner MH, et al. Guidance for timely and appropriate referral of patients with advanced heart failure: a scientific statement from the American Heart Association. Circulation 2021;144:e238-e250.
- Echols MR, Ogunniyi MO. Role and contribution of the general heart failure cardiologist: further expansion of the multidisciplinary heart failure approach. J Card Fail 2021;Dec 31:[Epub ahead of print].
- Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation 2021;143:e254-e743.
- Chuzi S, Reza N. Cultivating interest in heart failure careers: can we reverse the current trend?: cultivating interest in heart failure careers. J Card Fail 2021;27:819-21.
- Weissman G, Auseon AJ, Arrighi JA, et al. Perceptions and utilization of the U.S. Core Cardiovascular Training Statement. J Am Coll Cardiol 2019;73:2896-99.
- Sivagnanam K, Mendes LA, Schlendorf KH, et al. Bridge to transplantation: advanced heart failure and transplant cardiology training for cardiovascular disease fellows. J Am Coll Cardiol 2017;70:1413-16.
- Jessup M, Ardehali R, Konstam MA, et al. COCATS 4 Task Force 12: training in heart failure. J Am Coll Cardiol 2015;65:1866-76.
- Carnicelli AP, Blumer V, Genovese L, et al. The road not yet traveled: distinction in critical care cardiology through the advanced heart failure and transplant cardiology training pathway. J Card Fail 2022;28:339-42.
- Il'Giovine ZJ, Menon V. The intersection of heart failure and critical care: the contemporary cardiac intensive care unit and the opportunity for a unique training pathway. J Card Fail 2021;27:1152-55.
- Kassi M. The dawn of the invasive heart failure specialist. JACC Case Rep 2021;3:1336-38.
- Belkin MN, Karpenshif Y, Dugan E, Ambinder DI, Desai K, Goyal A. Letter to the Editor. J Card Fail 2022;28:348.
- Tehrani BN, Truesdell AG, Psotka MA, et al. A standardized and comprehensive approach to the management of cardiogenic shock. JACC Heart Fail 2020;8:879-91.
- Khan MS, Kumar P, Sreenivasan J, et al. Preventable deaths from heart disease and stroke among racial and ethnic minorities in the United States. Circ Cardiovasc Qual Outcomes 2021;14:e007835.
- Capers Q 4th, Johnson A, Berlacher K, Douglas PS. The urgent and ongoing need for diversity, inclusion, and equity in the cardiology workforce in the United States. J Am Heart Assoc 2021;10:e018893.
- ERAS Statistics (aamc.org). 2022. Available at: https://www.aamc.org/data-reports/interactive-data/eras-statistics-data. Accessed 02/10/2022.
- Njoroge JN, Youmans QR, Chuzi S. How cardiovascular disease fellows can promote diversity and inclusion in cardiology: doing our part. J Am Coll Cardiol 2021;78:1188-92.
Clinical Topics: Cardiac Surgery, Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Valvular Heart Disease, Vascular Medicine, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Acute Heart Failure, Heart Transplant, Mechanical Circulatory Support, Pulmonary Hypertension, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Hypertension
Keywords: Heart Failure, Motivation, Clinical Competence, Family Planning Services, Fellowships and Scholarships, Leadership, African Americans, Alaskan Natives, Heart-Assist Devices, Hypertension, Pulmonary, Obstetrics, Palliative Care, Program Development, Schools, Medical, Shock, Cardiogenic, Stroke Volume, Universities, Vulnerable Populations, Heart Defects, Congenital, Certification, Curriculum, Education, Medical, Graduate, Heart Transplantation, Heart Valve Diseases, Accreditation, Employment, Critical Care, Workforce, Hospitals, Referral and Consultation, Faculty, Sexual and Gender Minorities
< Back to Listings