Clinical Applications of Cardiac Magnetic Resonance Imaging in Pericardial Diseases
Quick Takes
- MRI plays a critical and complimentary role in the evaluation and surveillance of pericardial diseases, including pericarditis, pericardial effusion, and pericardial constriction.
- Key MRI sequences utilized include steady-state free precession cine sequence for function and effusion, free-breathing cine sequence for constriction, short-tau inversion recovery for edema, and late gadolinium enhancement sequence for inflammation/fibrosis.
- Sound fundamental understanding of the indications, strengths, and limitations of MRI in pericardial diseases is important for cardiologists and radiologists to interpret MRI findings and guide management of patients with pericardial diseases.
Introduction
Pericardial diseases are a heterogeneous group of clinical entities ranging from pericardial inflammation (pericarditis), pericardial effusion, pericardial constriction, masses and congenital anomalies, and often present diagnostic challenges in clinical practice.1 Multimodality imaging including echocardiography, computed tomography, and magnetic resonance imaging (MRI) have their own strengths and weaknesses but play complimentary roles in the assessment of pericardial diseases.2,3 MRI in particular needs to be performed and analyzed at a high standard to draw clinically meaningful information and guide management of these patients. This expert analysis article explores the main sequence clinical applications of MRI (Table 1) in the evaluation of pericardial diseases based on a recent review article.4
Table 1
| MRI sequence | Assess for | Implications for pericardial diseases |
| Steady state free precision (cine SSFP) | Pericardial effusion Tubular/conical deformity, tethering Ventricular diastolic/atrial systolic collapse, swinging heart Abnormal chamber function, and regional wall motion abnormalities |
Pericardial effusion, may also support pericarditis diagnosis, consider effusive-constrictive pericarditis if constrictive physiology also present Pericardial constriction Pericardial tamponade Concurrent cardiomyopathy process, including myocarditis and ischemic heart disease |
| Black blood spin echo | Increased pericardial thickness | Pericarditis and/or constriction |
| Free breathing cine (gradient echo) | Respirophasic septal shift | Pericardial constriction |
| T2 short tau inversion recovery (T2-STIR) | Increased pericardial signal Increased myocardial signal |
Pericarditis (acute/subacute) Myocarditis (acute/subacute) |
| Phase sensitive inversion recovery (PSIR) | Increased pericardial signal Increased myocardial signal -Subendocardial/transmural -Epicardial or mid-myocardial |
Pericarditis (all time-frames) Consider transient constriction if constrictive physiology also present Ischemic heart disease Non-ischemic cardiomyopathy (e.g., myocarditis, infiltrative heart diseases) |
| Optional: Radiofrequency tissue-tagging | Pericardial tethering | Pericardial constriction |
| Optional: Phase contrast | Respirophasic variation of mitral (>25%) and tricuspid inflow (>40%) | Pericardial constriction or tamponade |
| Optional: T1/T2 mapping | Increased pericardial native T1 and/or T2 mapping values | Pericardial inflammation/fibrosis and/or edema/respectively |
Pericarditis
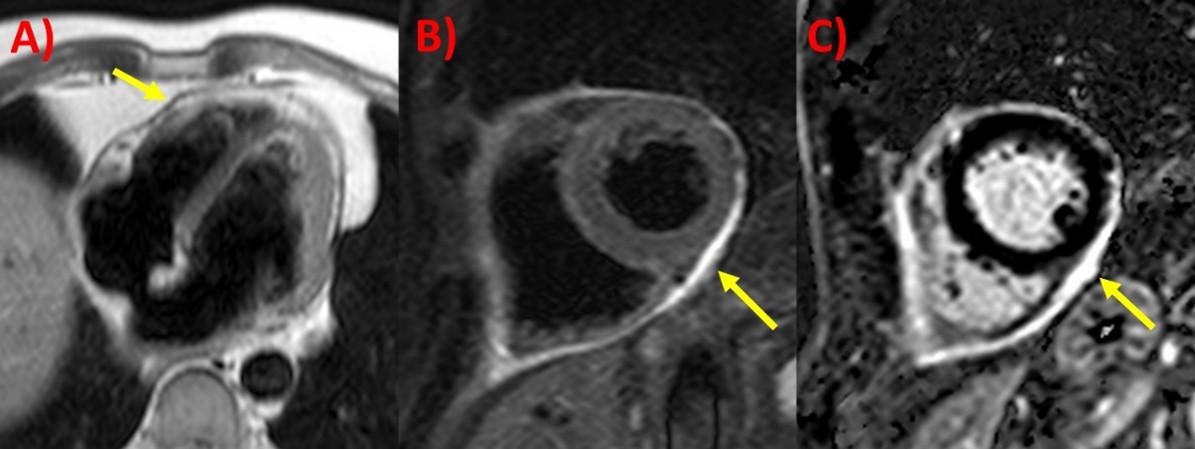
Pericardial inflammation is diagnosed based on at least two criterion including pericardic chest pain, pericardial rub on examination, new electrocardiogram (ECG) changes (widespread ST-elevation or PR depression) and new or worsening pericardial effusion on imaging, along with supportive findings such as elevated inflammatory biomarkers and pericardial inflammation on MRI. It is classified by its onset duration (acute, incessant, recurrent, or chronic) and etiologies (such as idiopathic, infective, iatrogenic/traumatic, autoimmune, neoplastic, metabolic, and drug-induced).1,5 Echocardiography, although routinely performed, actually has a limited role in pericarditis assessment, mainly to look for pericardial effusion as well as differentials like heart failure.2 The key MRI findings of pericarditis as indicated in Figure 1 include pericardial thickening on black-blood spin echo sequence (Figure 1A, can be T1 or T2-weighted),2,4 increased pericardial signal on T2 short tau inversion recovery sequence (T2-STIR) indicating edema (Figure 1B, typically present in acute but not late phase of pericarditis), and pericardial late gadolinium enhancement (LGE) on phase sensitive inversion recovery (PSIR) sequence (Figure 1C).
Figure 1
Phase sensitive inversion recovery (PSIR) sequence is central in the diagnosis of pericardial inflammation on MRI as well as surveillance such as evaluating response to anti-inflammatory therapies.6 Importantly, because epicardial fat may also enhance on PSIR sequence, fat-suppression pulse added to PSIR sequence is preferred.4 Severity of pericardial LGE on initial MRI is significantly associated with recurrent pericarditis flares and escalation of therapy, and quantitative methods of pericardial LGE recently developed in the research setting have potential future clinical applications.7 T1- and T2 mapping typically utilized in myocardial disease and tissue characterization assessment are starting to be applied to the pericardium, whereby elevated values may indicate pericardial fibrosis and edema respectively, however remains limited because of the thin pericardium and lack of reference ranges for the normal pericardium.4 Steady state free precession (SSFP) cine imaging is useful to assess for cardiac chamber size and function and regional wall abnormalities, and concomitant pericardial effusion with pericarditis, while PSIR sequence can also identify presence of myocardial LGE that may indicate concurrent myocarditis or other non-ischemic causes of scar-like sarcoidosis (epicardial or mid-myocardial distribution LGE) or ischemic heart disease (subendocardial or transmural LGE).4,8
Pericardial Effusion
Pericardial effusion is the abnormal excess accumulation of fluid in the pericardial sac, classified by size (<10mm mild, 10-20mm moderate and ≥20mm large), distribution (localized or circumferential), composition (transudate or exudate) and onset (acute, subacute, or chronic).1 Echocardiography is the primary imaging modality to diagnose and monitor pericardial effusion and assess for pericardial signs of tamponade, however MRI has unique features and advantages.2 If echocardiography views are suboptimal, MRI better delineates the distribution and extent of pericardial effusion, along with identifying features of tamponade such as chamber collapse (diastolic collapse of ventricle(s), late-diastolic/early-systolic collapse of right atrium for at least one-third of the cardiac cycle), plethoric inferior vena cava and swinging heart.4 Various MRI sequences contribute to the tissue characterization of pericardial effusion content.9,10 For example, simple transudate effusions appear as high signal on T2 weighted and bright blood cine imaging, and low signal on T2 weighted and LGE imaging, while exudative effusions or with blood products have higher signal on T1 weighted and intermediate signal on T2 weighted imaging, often with fibrinous components.
Constrictive Pericarditis
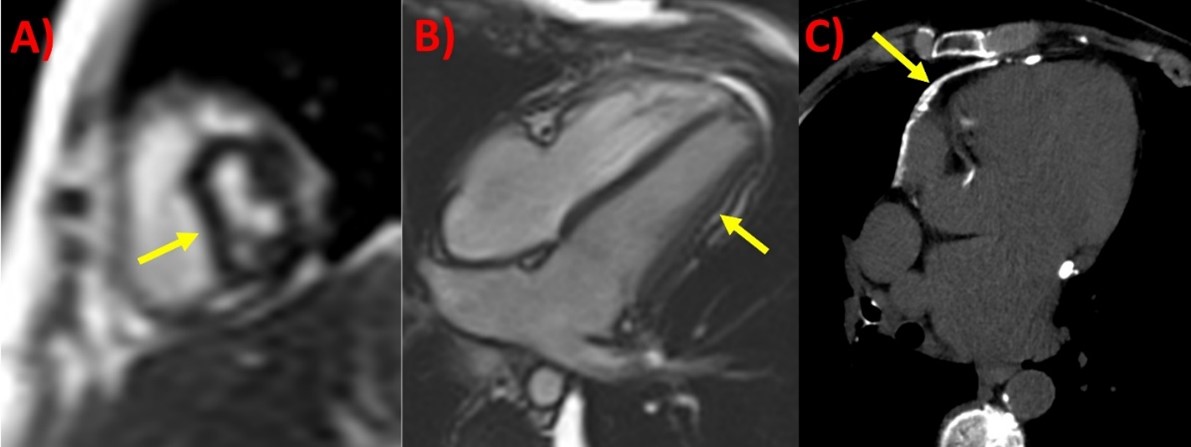
Constrictive pericarditis is usually caused by chronic or recurrent pericarditis leading to constraint of heart chambers and associated congestive heart failure symptoms.1 Echocardiography is also the first-line modality to diagnose pericardial constriction using the Mayo Clinic criteria, while computed tomography can identify pericardial calcifications less well seen on other imaging modalities including cardiac catheterization.2,11 MRI is mainly utilized if echocardiography is indeterminate, and the most important findings to support constrictive physiology are respirophasic interventricular septal excursion and bounce (free-breathing sequence), increased pericardial thickness (black-blood sequence), and conical or tubular deformity of the ventricles with wall tethering (SSFP cine and optional myocardial tagging sequences) (Figure 2).4,12
Figure 2
Phase contrast sequence when taken at the mitral and tricuspid valve inflows, whereby of ≥25% decrease and ≥40% increase in their velocities respectively during inspiration, is suggestive of pericardial constriction or tamponade, mimicking echocardiography.9 Two unique phenotypes are a) transient constriction, when the constrictive physiology is after a period of time with anti-inflammatory therapy or spontaneously; along with b) effusive-constrictive pericarditis, where there is concomitant pericardial effusion and even after removal of the effusion display constrictive physiology.1 Presence of pericardial LGE also increases the probability of transient constriction and improvement with medical treatments, and together with other findings help guide the need to initiate, escalate or withdraw anti-inflammatories along with considering pericardiectomy surgery.6,13
Conclusion
MRI is a valuable tool in the assessment and monitoring of pericardial diseases, including pericarditis, pericardial effusion, constrictive pericarditis, and outside the scope of this review, pericardial masses, and congenital anomalies as well. MRI sequences routinely performed for these indications include SSFP cine sequence for function and effusion, free-breathing cine sequence for constriction, T2-STIR for edema, PSIR sequence for LGE indicating inflammation/fibrosis, and other T1- and T2-weighted and perfusion imaging for tissue characterization of pericardial effusion and masses. Clinicians should have a sound understanding of MRI applications and limitations and use in conjunction with other clinical, biomarker and imaging modalities to help guide management for pericardial diseases.
References
- Adler Y, Charron P, Imazio M. et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the Task Force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC) Endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
- Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Ecocardiogr 2013;26:965-1012.e15.
- Leiner T, Bogaert J, Friedrich MG, et al. SCMR Position Paper (2020) on clinical indications for cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2020;22:76.
- Wang TKM, Ayoub C, Chetrit M, et al. Cardiac magnetic resonance imaging techniques and applications for pericardial diseases. Circ Cardiovasc Imaging 2022;Jul 05:[Epub ahead of print].
- Cremer PC, Kumar A, Kontzias A, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol 2016;68:2311-28.
- Chetrit M, Xu B, Kwon DH, et al. Imaging-guided therapies for pericardial diseases. JACC Cardiovasc Imaging 2020;13:1422-37.
- Kumar A, Sato K, Yzeiraj E, et al. Quantitative pericardial delayed hyperenhancement informs clinical course in recurrent pericarditis. JACC Cardiovasc Imaging 2017;10:1337-46.
- Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson 2020;22:17.
- Aldweib N, Farah V, Biederman RWW. Clinical utility of cardiac magnetic resonance imaging in pericardial diseases. Curr Cardiol Rev 2018;14:200-12.
- Rajiah P, Canan A, Saboo SS, Restrepo CS, Bolen MA. MRI of the pericardium. Radiographics 2019;39:1921-22.
- Welch TD, Ling LH, Espinosa RE, et al. Echocardiographic diagnosis of constrictive pericarditis: Mayo Clinic criteria. Circ Cardiovasc Imaging 2014;7:526-34.
- Bolen MA, Rajiah P, Kusunose K, et al. Cardiac MR imaging in constrictive pericarditis: multiparametric assessment in patients with surgically proven constriction. Int J Cardiovasc Imaging 2015;31:859-66.
- Cremer PC, Tariq MU, Karwa A, et al. Quantitative assessment of pericardial delayed hyperenhancement predicts clinical improvement in patients with constrictive pericarditis treated with anti-inflammatory therapy. Circ Cardiovasc Imaging 2015;8e003125.
Clinical Topics: Cardiac Surgery, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Pericardial Disease, Stable Ischemic Heart Disease, Vascular Medicine, Cardiac Surgery and Heart Failure, Cardiac Surgery and SIHD, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Interventions and Imaging, Interventions and Vascular Medicine, Computed Tomography, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Nuclear Imaging, Chronic Angina
Keywords: Pericarditis, Constrictive, Pericardial Effusion, Pericardiectomy, Contrast Media, Gadolinium, Cardiac Tamponade, Cicatrix, Constriction, Heart Ventricles, Myocarditis, Reference Values, ST Elevation Myocardial Infarction, Tricuspid Valve, Vena Cava, Inferior, Pericarditis, Pericardium, Inflammation, Magnetic Resonance Imaging, Echocardiography, Anti-Inflammatory Agents, Tomography, X-Ray Computed, Cardiac Catheterization, Heart Failure, Electrocardiography, Perfusion Imaging, Heart Atria, Sarcoidosis, Exudates and Transudates, Biomarkers, Chest Pain, Iatrogenic Disease, Phenotype, Tomography, Edema
< Back to Listings