Pericarditis in Athletes: Approach to Exercise Restriction
Quick Takes
- Exercise and elevated heart rates have been postulated to promote inflammation and exacerbate pericarditis. Exercise restriction is recommended for all patients based on expert consensus and limited data.
- Exercise restriction is recommended until complete resolution of the acute pericarditis phase based on clinical parameters. While guidelines suggest a minimum of 1-3 months of restriction, an individualized approach is reasonable given variability in disease severity and course.
- Resumption of exercise should ideally take place in a graduated fashion with monitoring for recurrent pericarditis. Exercise testing can be considered prior to return to high intensity or competitive sport for further risk stratification, particularly if there is suspicion for myocardial involvement.
Pericarditis is an inflammatory disease of the pericardial layers, often due to an unclear inciting agent, with a subsequent immune response. The diagnosis is made clinically with characteristic features including pleuritic chest pain, pericardial friction rub, electrocardiographic (ECG) changes, and/or a new pericardial effusion.1-3 Multimodality imaging as well as inflammatory markers such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), elevated in up to 80% of cases, help to confirm the diagnosis and track the course of the disease.2 The incidence amongst athletes is unclear but pericarditis is estimated to account for 5% of all cardiac chest pain presentations amongst the general population.1,2
In developed nations, the majority of cases are due to a viral etiology or idiopathic in origin. The onset of the COVID-19 pandemic raised concerns regarding the possibility of myocarditis and pericarditis due to SARS-CoV-2 infection, particularly in athletes. Early screening cardiac magnetic resonance imaging (MRI) studies in student-athletes suggested significant rates of subclinical pericardial changes post COVID-19 infection.4 However, the significance of these findings were unclear in the absence of clinical features for pericarditis and further clouded by lack of controls and small sample sizes. Additionally, the high prevalence of pericardial involvement after COVID-19 infection has not been replicated in follow-up studies. A subsequent large prospective study of collegiate athletes demonstrated low (0.7%) incidence of myocardial or pericardial disease post COVID-19 illness.5 Similarly low rates of cardiac involvement have since been reported in other competitive athlete cohorts.6 Additionally, pericarditis and myocarditis related to COVID-19 vaccination have been reported but are quite rare (0.5 to 1 case per 100,000 individuals) with higher occurrence in younger ages (16-29 years) and male sex.7,8
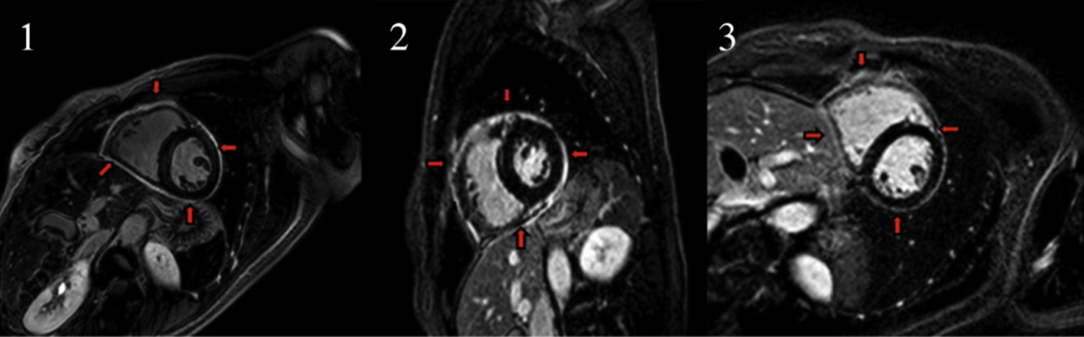
Exercise restriction, in combination with pharmacotherapy, is mainstay in the management of pericarditis. It is postulated that elevated heart rates lead to increased shear stress across the pericardial layers promoting inflammation and extending the course of disease. Prolonged disease course raises risk for constrictive physiology and in cases with myocardial involvement, increases risk of cardiomyopathy and exercise-induced arrhythmias. While plausible, it is important to note that there are no robust data to demonstrate the benefits of exercise restriction during acute pericarditis. Anecdotal data have shown disease progression on cardiac MRI in those who continue to exercise during the acute phase with regression on subsequent abstinence from exercise (Figure 1).9 Pragmatically, restriction is also logical as exercise during acute exacerbation is generally uncomfortable and athletic performance is limited by symptoms. Therefore, it seems reasonable to abstain from exercise until resolution of an acute event.
Figure 1
[1] Cardiovascular magnetic resonance (CMR) demonstrating pericardial late gadolinium enhancement (LGE); [2] with continued exercise, there is progression of LGE; [3] and with restriction in activity, there is improvement in LGE. LGE is an important prognosticator of pericarditis, and with a sensitivity of up to 94%, it is vital in providing additional information that includes severity and potential complications. Reprinted with permission from Shah NP, Verma BR, Ala CK, et al. Exercise is good for the heart but not for the inflamed pericardium? JACC Cardiovasc Imaging 2019;12:1880-81.
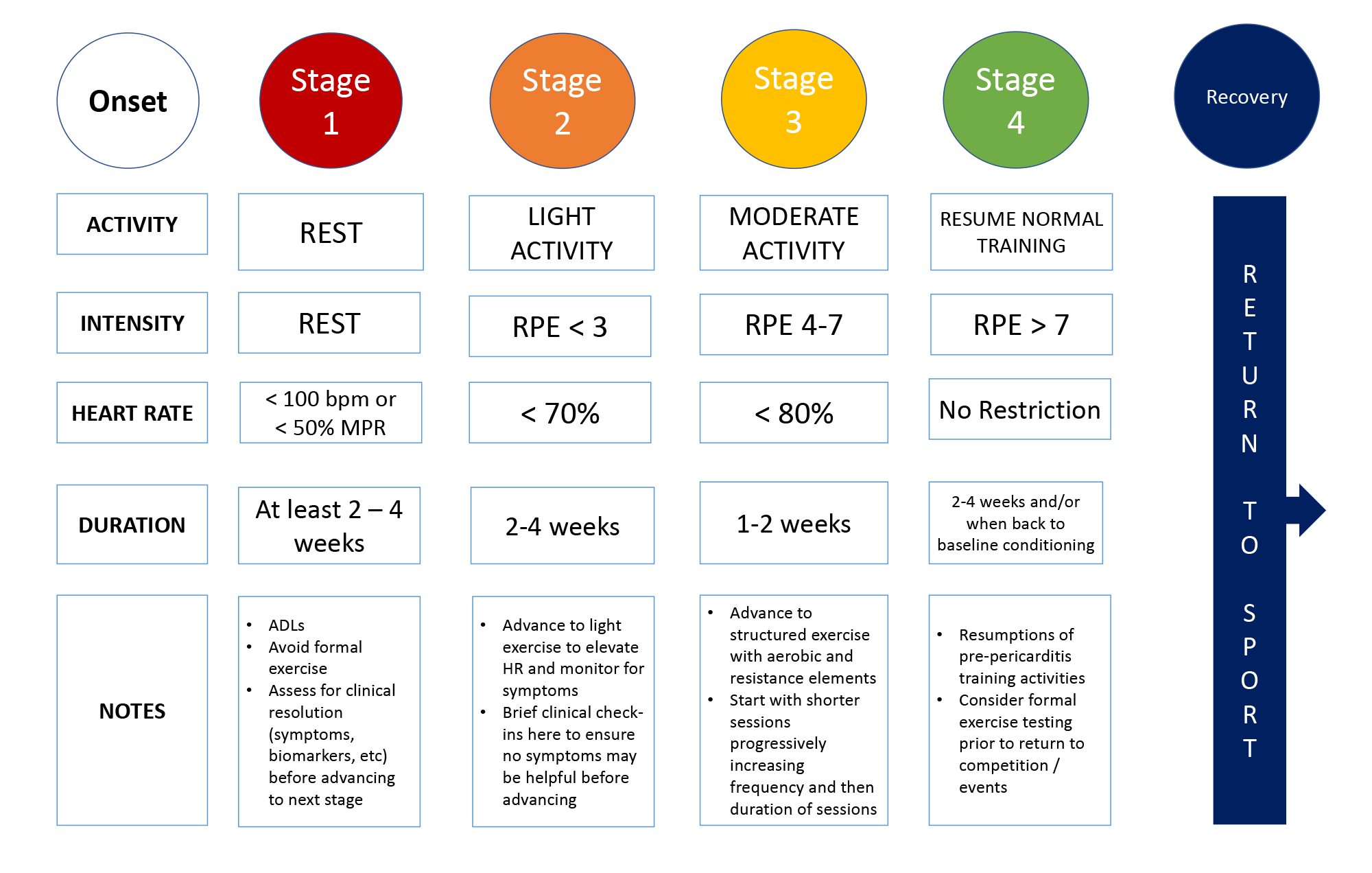
Historically, 3-6 months of restriction was recommended with more recent guidelines suggesting a minimum of 1-3 months of rest.10 Longer periods of exercise restriction have implications regarding deconditioning, mental health, and potential financial loss for competitive athletes. Further, the course and severity of pericarditis is variable amongst individuals likely attributable to genetic factors as well as the inciting etiology.2 In light of this, a tailored approach with shared decision-making and integration of clinical factors to determine the duration of restriction (Figure 2) seems appropriate.
Figure 2
A suggested approach to management of pericarditis with guidance on exercise restriction. The goal is to create an approach that is appropriate for the individual athlete. RPE: rate of perceived exertion, HR: heart rate, MHR: maximum heart rate, ECG: electrocardiogram. Courtesy of Sivalokanathan S, Chokshi NP.
In our opinion, at least 2-4 weeks of abstinence from intense activity is generally useful to assess benefits of pharmacotherapy and ensure resolution of symptoms. Also, a graduated approach to resumption of training with respect to intensity and duration is advisable (Figure 3). This facilitates clinical check-ins at each stage for recurrent symptoms and early intervention if necessary. Patient guidance for appropriate intensity of exercise at each stage can be provided using the self-assessed rate of perceived exertion (scale 1-10), heart rate parameters, or based on symptom onset. Before return to high intensity or competitive sport, exercise testing and remote rhythm monitoring can be considered for further risk stratification, particularly if there is concern for myocardial involvement.
Figure 3
A sample approach to graduated exercise after onset of acute pericarditis. Each program and duration within a particular stage should ideally be tailored to the patient's clinical features taking into consideration their benefit to risk ratio for exercise and involvement of the patient in shared decision making when appropriate. RPE: rate of perceived exertion, HR: heart rate, MHR: maximum heart rate, ADL: activities of daily living. Courtesy of Sivalokanathan S, Chokshi NP.
The pharmacological approach to athletes with pericarditis is similar to the general population. High dose non-steroidal anti-inflammatory drugs (NSAIDs) are the first line of treatment until resolution of symptoms and normalization of biomarkers. Colchicine is beneficial in treatment of the acute phase and longer term for prevention of recurrence. In athletes, it may be helpful to pursue a slower taper of NSAIDs with overlap during ramp-up of exercise regimens to ensure resolution. A similar strategy with longer durations of colchicine during return to sport may help with preventing recurrence.
As with many cardiovascular conditions, the evaluation and management of pericarditis in athletes requires examination from the lens of exercise and sport. It is a challenging scenario given that exercise may exacerbate the condition. Given the premium placed on exercise by these patients, the variability in clinical presentations, and lack of randomized trial data, a tailored approach to each athlete is reasonable.
References
- Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA 2015;314:1498-506.
- Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC State-of-the-Art Review. J Am Coll Cardiol 2020;75:76-92.
- Imazio M, Gaita F. Diagnosis and treatment of pericarditis. Heart 2015;101:1159-68.
- Brito D, Meester S, Yanamala N, et al. High prevalence of pericardial involvement in college student athletes recovering from COVID-19. JACC Cardiovasc Imaging 2021;14:541-55.
- Moulson N, Petek BJ, Drezner JA, et al. SARS-CoV-2 cardiac involvement in young competitive athletes. Circulation 2021;144:256-66.
- Alosaimi B, AlFayyad I, Alshuaibi S, et al. Cardiovascular complications and outcomes among athletes with COVID-19 disease: a systematic review. BMC Sports Sci Med Rehabil 2022;14:74.
- Simone A, Herald J, Chen A, et al. Acute myocarditis following COVID-19 mRNA vaccination in adults aged 18 years or older. JAMA Intern Med 2021;181:1668-70.
- Witberg G, Barda N, Hoss S, et al. Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med 2021;385:2132-39.
- Shah NP, Verma BR, Ala CK, et al. Exercise is good for the heart but not for the inflamed pericardium? JACC Cardiovasc Imaging 2019;12:1880-81.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC) endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, COVID-19 Hub, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Pericardial Disease, Prevention, Sports and Exercise Cardiology, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Heart Failure and Cardiac Biomarkers, Magnetic Resonance Imaging, Sports and Exercise and ECG and Stress Testing, Sports and Exercise and Imaging
Keywords: Activities of Daily Living, Sports, Sports Medicine, Return to Sport, Athletes, COVID-19, SARS-CoV-2, Pericardial Effusion, C-Reactive Protein, COVID-19 Vaccines, Contrast Media, Gadolinium, Heart Rate, Prospective Studies, Exercise Test, Physical Exertion, Blood Sedimentation, Decision Making, Shared, Follow-Up Studies, Mental Health, Myocarditis, Pandemics, Pericarditis, Pericardium, Electrocardiography, Colchicine, Anti-Inflammatory Agents, Magnetic Resonance Imaging, Athletic Performance, Disease Progression, Risk Assessment, Magnetic Resonance Spectroscopy, Immunity, Inflammation, Vaccination, Arrhythmias, Cardiac, Chest Pain, Biomarkers, Anti-Inflammatory Agents, Non-Steroidal
< Back to Listings