Healthy Lifestyle Reduces Leading Causes of Death Worldwide
Quick Takes
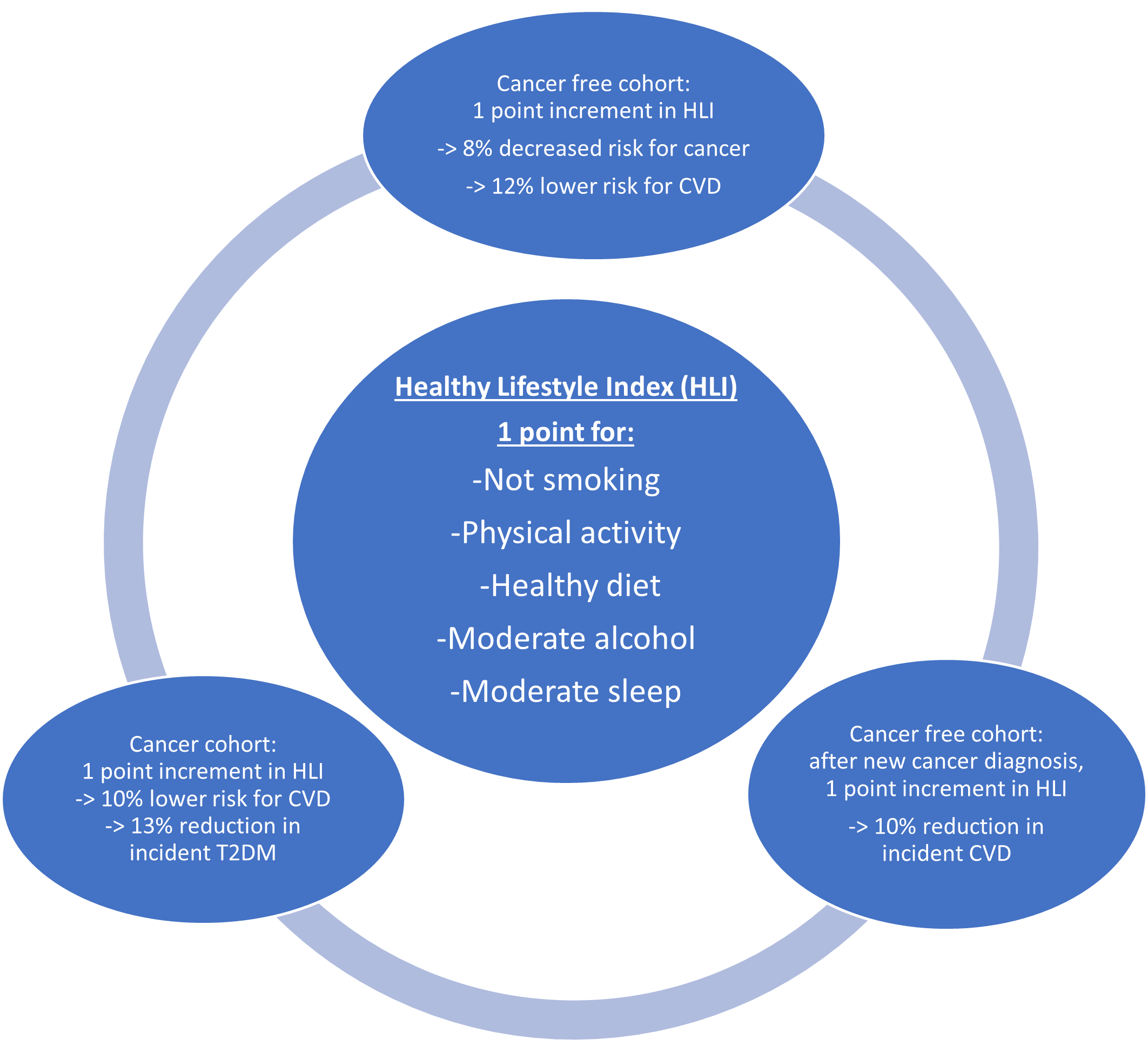
- Adherence to a healthy lifestyle is associated with a lower risk for developing new onset cancer, CVD, and T2DM in a healthy population and significantly attenuates risk for subsequent CVD and T2DM in those with new diagnosis of cancer or history of cancer.
- Targeting shared risk factors and shared mechanistic causes of CVD and cancer should be the focus of preventative strategies to target these leading causes of death worldwide.
Cancer, cardiovascular disease (CVD), and type 2 diabetes mellitus (T2DM) share many of the same risk factors and are leading causes of death in the United States (US) and globally.1 Preventable risk factors account for more than 90% of myocardial infarctions,2 and individuals with healthy lifestyles have 75% lower risk of incident T2DM compared to individuals with less healthy lifestyles.3 Moreover, the leading comorbidities in patients with cancer are CVD and T2DM.4,5 Accordingly, the cardiovascular and oncology guidelines promote the importance of a healthy lifestyle in the primary prevention of these outcomes.6,7
Cao et al. conducted a prospective, population-based study involving both a healthy and cancer prevalent cohort from the general population enrolled in the UK Biobank.8 Investigators evaluated the effect of a healthy lifestyle on the incidence of cancer as well as CVD and T2DM among the cohort of 397,136 healthy participants. They also assessed the effect of healthy lifestyle on development of CVD and T2DM among the cohort of 35,564 individuals with cancer but no pre-existing CVD or T2DM. Healthy lifestyle index (HLI) was measured for each participant and 1 point was added for 1) no current smoking, 2) regular physical activity, 3) healthy dietary habits, 4) moderate alcohol consumption, and 5) sleep duration of 6-8 hours.
In the healthy cohort, over 15 years of follow-up, 10.1% of subjects developed cancer, and 6.38% and 4.18% of those patients with incident cancer developed CVD and T2DM respectively. Subjects with only 0 or 1 healthy lifestyle measure were designated as the reference group. For each 1-point increment in HLI compared to the reference, the risk of transitioning from cancer to subsequent CVD and T2DM was decreased by 10% (hazard ratio [HR]: 0.90, 95% confidence interval [CI]: 0.86-0.94) and 16% (HR: 0.84, 95% CI: 0.79-0.89) respectively. In the cohort of cancer survivors, 8.2% and 3.6% of subjects developed CVD and T2DM respectively. Each 1-point increment in HLI compared to reference was associated with 10% lower risk for CVD (HR: 0.90; 95% CI: 0.87-0.93) and 13% lower risk for T2DM (HR: 0.87; 95% CI: 0.83-0.91). These findings were stronger in women than men, were independent of age, and were dose-dependent (cancer survivors who achieved all 5 measures of a healthy lifestyle were at 44% and 38% reduced risk for subsequent CVD and T2DM, respectively, compared to the reference).
A major strength of this trial is the large sample size comprising two separate cohorts of healthy participants and cancer survivors. Long-term follow-up allowed for a significant number of events to be analyzed. Multistate models and sensitivity analyses allowed for robust assessment and reduced potential confounding or contribution of reverse causality to the outcomes. Observational design of this study limits its implication of causality. Limited diversity of the study population impacts the generalizability of the findings. Additionally, analysis of the HLI in an increment fashion compared to a reference of 0 or 1 healthy lifestyle factors excludes a comparison between risk factors on the risks of CVD and T2DM. Still, associations can be drawn, and the authors did provide an analysis of the impact of each lifestyle factor on the transition from a healthy to a disease state. A further limitation of this trial is that healthy lifestyle factors were only collected at baseline disregarding changes over time which may have biased the results.
As noted by Drs. Michos and Marshall in their editorial on the study, the inclusion of moderate alcohol consumption as a healthy lifestyle in this study is surprising and controversial.9 Though light alcohol consumption was found to be favorable in some studies, moderate alcohol use is associated with increased CVD risk and is a risk factor for many cancers. Furthermore, the American Heart Association (AHA) and American Society of Clinical Oncology (ASCO) do not recommend alcohol as a preventative strategy for CVD or cancer.6,10 Another surprising finding was that a healthy lifestyle was associated with elevated risk for prostate cancer and melanoma, though as Drs. Michos and Marshall point out, this may be related to screening practices and ultraviolet exposure with outdoor physical activity.
The trial highlights the critical importance of a healthy lifestyle to prevent CVD and T2DM both in healthy subjects and cancer survivors. While adherence to a healthy lifestyle is associated with a lower risk for developing new onset cancer, CVD, and T2DM in a healthy population, it is empowering to recognize that the effect of a healthy lifestyle on the prevention of CVD and T2DM is not attenuated by a cancer diagnosis. Preventative strategies are synergistically beneficial in mitigating these most common causes of morbidity and mortality in the US and globally. To reduce the global burden of cancer, CVD, and T2DM, we should target shared risk factors and emphasize a healthy lifestyle for prevention. To further augment these efforts, they should be supported by appropriate screening measures and policy interventions.
Figure 1
References
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88.
- Joseph P, Leong D, McKee M, et al. Reducing the global burden of cardiovascular disease, Part 1: the epidemiology and risk factors. Circ Res 2017;121:677-94.
- Zhang Y, Pan XF, Chen J, et al. Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. Diabetologia 2020;63:21-33.
- Florido R, Daya NR, Ndumele CE, et al. Cardiovascular disease risk among cancer survivors: the Atherosclerosis Risk in Communities (ARIC) study. J Am Coll Cardiol 2022;80:22-32.
- Masson R, Titievsky L, Corley DA, et al. Incidence rates of cardiovascular outcomes in a community-based population of cancer patients. Cancer Med 2019;8:7913-23.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:e177-e232.
- LoConte NK, Gershenwald JE, Thomson CA, Crane TE, Harmon GE, Rechis R. Lifestyle modifications and policy implications for primary and secondary cancer prevention: diet, exercise, sun safety, and alcohol reduction. Am Soc Clin Oncol Educ Book 2018;38:88-100.
- Cao Z, Xu C, Yang H, Li S, Wang Y. The role of healthy lifestyle in cancer incidence and temporal transitions to cardiometabolic disease. JACC CardioOncol 2021;3:663-74.
- Michos ED, Marshall CH. Healthy lifestyle benefits both cancer and cardiovascular disease. JACC CardioOncol 2021;3:675-77.
- LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and cancer: a statement of the American Society of Clinical Oncology. J Clin Oncol 2018;36:83-93.
Clinical Topics: Cardio-Oncology, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Prevention, Exercise, Smoking
Keywords: Follow-Up Studies, Healthy Volunteers, Cardiovascular Diseases, Diabetes Mellitus, Type 2, Prospective Studies, American Heart Association, Cancer Survivors, Confidence Intervals, Sample Size, Life Style, Healthy Lifestyle, Risk Factors, Primary Prevention, Alcohol Drinking, Tobacco Smoking, Smoking, Exercise, Myocardial Infarction, Medical Oncology, Cardio-oncology, Cardiotoxicity, Prostatic Neoplasms, Early Detection of Cancer
< Back to Listings