Randomized Trial of Left Bundle Branch Versus Biventricular Pacing For Cardiac Resynchronization Therapy
Quick Takes
- Left bundle branch pacing (LBBP) has emerged as a novel physiological pacing modality.
- LBBP overcomes left bundle branch block (LBBB) and improves left ventricular function.
- Based on trial results, LBBP might be a promising first-line resynchronization strategy alongside BiVP-CRT in clinical practice for patients with non-ischemic cardiomyopathy and LBBB.
Introduction
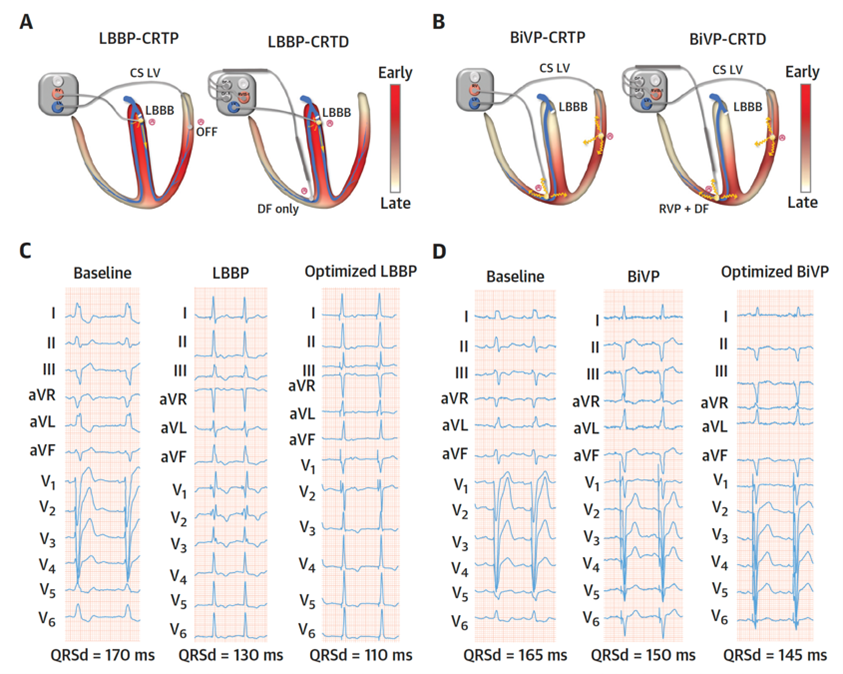
Cardiac resynchronization therapy (CRT) using biventricular pacing (BiVP) is a well-established therapy for patients with cardiomyopathy, heart failure (HF), reduced left ventricular ejection fraction (LVEF), and left bundle branch block (LBBB). However, up to one-third of patients treated with BiVP showed no response to CRT. Recently, His-Purkinje conduction system pacing including His bundle pacing (HBP) and left bundle branch pacing (LBBP) has emerged as a physiological pacing modality which engages the intrinsic cardiac conduction system and can achieve favorable electrical and mechanical synchrony of the left ventricle (LV).1-3 Several previous studies showed that both HBP and LBBP can correct LBBB and improve cardiac function for HF patients.4-8 However, HBP failed to exhibit clear advantages in CRT over BiVP due to the low success rates of His corrective pacing (His-SYNC).9 Compared with HBP, LBBP can produce stable pacing thresholds, adequately sensed R-wave amplitude, and higher likelihood to correct LBBB by pacing more distal to the site of conduction block (Figure 1).10
Figure 1
LBBP has the potential advantages of backup left ventricular septal capture in addition to LBB capture. Although these promising results have led to growing enthusiasm of utilizing LBBP as an alternative CRT modality, there are no prospective randomized trials comparing the efficacy of these two techniques on improvement of LVEF and other measures of cardiac function among patients with non-ischemic cardiomyopathy (NICM) and LBBB.
Design of LBBP-RESYNC Trial
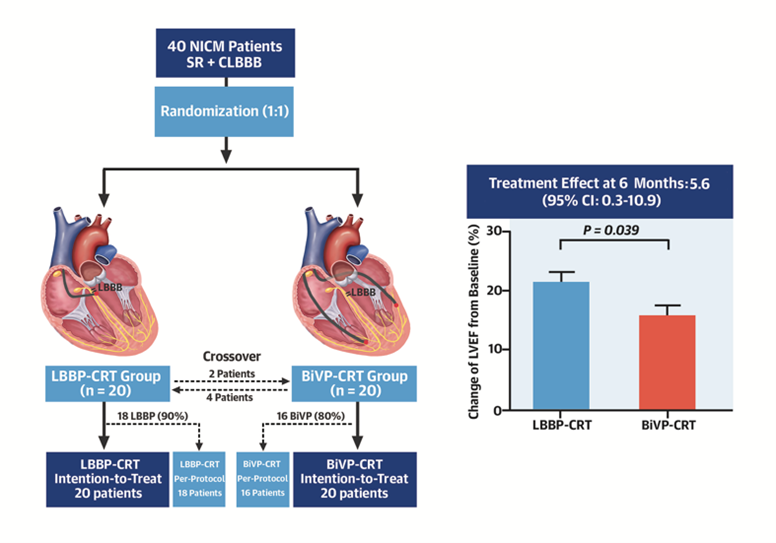
LBBP-RESYNC (Left Bundle Branch Pacing Versus Biventricular Pacing for Cardiac Resynchronization Therapy) was an investigator-initiated, prospective, randomized, controlled pilot trial.11 LBBP-RESYNC randomized (1:1) the patients with NICM, LBBB meeting Strauss's standard definition (QRSd >140 ms for male or >130 ms for female), LVEF ≤40%, and NYHA class II to IV into two groups of LBBP-CRT and BiVP-CRT. All enrolled patients underwent at least 3-month guideline-directed medical therapy (GDMT). Crossovers were allowed if LBBP or BiVP were unsuccessful. LBBP was performed using the SelectSecure™ pacing lead (model 3830, Medtronic) as previously described.12 Successful LBB capture is confirmed when 1) LBBB morphology disappeared and paced RBBB pattern was observed; 2) LVAT (stimulus to peak of R wave in V5-V6) was ≤100 ms at low pacing output; AND at least one of the following was achieved: a) abrupt shortening of LVAT by >10 ms with increasing output and remained short and constant at high and low output; b) transition from nonselective to selective LBBP; c) transition from nonselective LBBP to left ventricular septal pacing (LVSP). BiVP was implanted by a standard-of-care procedure. All patients were planned for 6-month follow-up. The primary endpoint was the difference in change of LVEF from baseline to 6-month follow up between two groups. The secondary endpoints included changes in echocardiographic measurements, N-terminal pro-B-type natriuretic peptide (NT-proBNP) concentration, NYHA class, 6-minute walk distance (6MWD). The paced QRSd and echocardiographic response to CRT were also compared between two groups.
Main Results
The study included 40 consecutive patients (20 males, mean age 63.7 years, LVEF 29.7 ± 5.6%). Crossovers occurred in 10% of LBBP-CRT and 20% of BiVP-CRT. Intention-to-treat analysis showed significantly higher LVEF improvement at 6 months after LBBP-CRT than BiVP-CRT (mean difference 5.6%, 95% CI, 0.3 - 10.9; P = 0.039) (Figure 2).
Figure 2
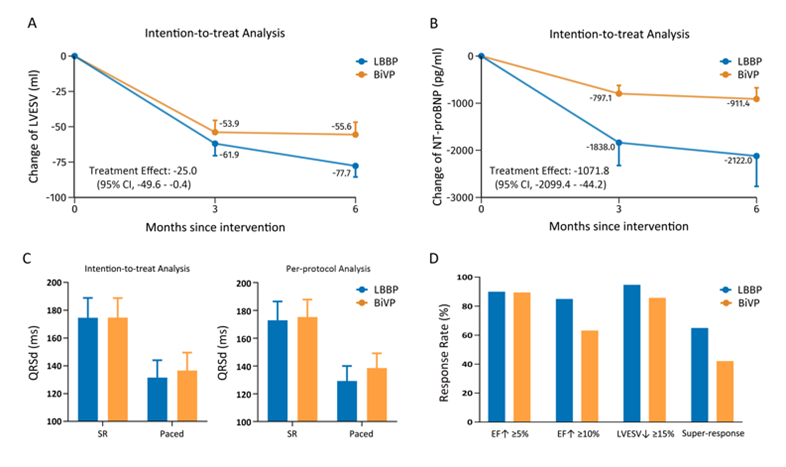
LBBP-CRT also appeared to have greater reductions in LV end-systolic volume (-24.97 ml, 95% CI, -49.58 - -0.36) and NT-proBNP (-1071.80 pg/ml, 95% CI, -2099.40 - -44.20), and comparable changes in NYHA class, 6MWD, QRS duration, and rates of CRT response compared with BiVP-CRT (Figure 3).
Figure 3
Conclusion
This randomized pilot study of LBBP-CRT versus BiVP-CRT demonstrated superiority of LBBP-CRT in LVEF improvement. Favorable reduction in left ventricle end-systolic volume (LVESV) and NT-proBNP were observed in LBBP-CRT group, and QRS narrowing were comparable between two groups. LBBP and BiVP might be effective and complementary resynchronization strategies for CRT in patients with non-ischemic cardiomyopathy and LBBB.
Future Perspectives
LBBP overcomes LBBB and often improves LV function. LBBP might be a promising first-line resynchronization strategy alongside BiVP-CRT in clinical practice for patients with non-ischemic cardiomyopathy and LBBB. Both LBBP and BiVP could be unsuccessful in some challenging cases. Future larger-scale prospective randomized trials are needed to compare the long-term effects of LBBP and BiV pacing on functional status and survival in patients with HF and LBBB.
References
- Zhang JL, Guo JH, Hou XF, et al. Comparison of the effects of selective and non-selective His bundle pacing on cardiac electrical and mechanical synchrony. Europace 2018;20:1010-17.
- Hou XF, Qian ZY, Wang Y, et al. Feasibility and cardiac synchrony of permanent left bundle branch pacing through the interventricular septum. Europace 2019;21:1694-1702.
- Qian ZY, Hou XF, Wang Y, et al. Physiological left bundle branch pacing validated by ultra-high density ventricular mapping in a swine model. Circ Arrhythm Electrophysiol 2020;13:e007898.
- Sharma PS, Dandamudi G, Herweg B, et al. Permanent His-bundle pacing as an alternative to biventricular pacing for cardiac resynchronization therapy: a multi-center experience. Heart Rhythm 2018;15:413-20.
- Huang WJ, Su L, Wu SJ, et al. A novel pacing strategy with low and stable output: pacing the left bundle branch immediately beyond the conduction block. Can J Cardiol 2017;33:1736.e1-1736.e3.
- Zhang WW, Huang JJ, Qi YD, et al. Cardiac resynchronization therapy by left bundle branch area pacing in patients with heart failure and left bundle branch block. Heart Rhythm 2019;16:1783-90.
- Vijayaraman P, Ponnusamy S, Cano Ó, et al. Left bundle branch area pacing for cardiac resynchronization therapy. Results from the International LBBAP collaborative study group. JACC Clin Electrophysiol 2021;7:135-47.
- Chen XY, Ye Y, Wang ZK, et al. Cardiac resynchronization therapy via left bundle branch pacing vs. optimized biventricular pacing with adaptive algorithm in heart failure with left bundle branch block: a prospective, multi-centre, observational study. Europace 2022;24:807-16.
- Upadhyay GA, Vijayaraman P, Nayak HM, et al. His corrective pacing or biventricular pacing for cardiac resynchronization in heart failure. J Am Coll Cardiol 2019;74:157-59.
- Li XF, Li H, Ma WT, et al. Permanent left bundle branch area pacing for atrioventricular block: feasibility, safety, and acute effect. Heart Rhythm 2019;16:1766-73.
- Wang Y, Zhu HJ, Hou XF, et al. Randomized trial of left bundle branch vs biventricular pacing for cardiac resynchronization therapy. J Am Coll Cardiol 2022;80:1205-16.
- Huang WJ, Chen XY, Su L, Wu S, Xia X, Vijayaraman P. A beginner's guide to permanent left bundle branch pacing. Heart Rhythm 2019;16:1791-96.
Clinical Topics: Arrhythmias and Clinical EP, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Implantable Devices, EP Basic Science, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Echocardiography/Ultrasound
Keywords: Cardiac Resynchronization Therapy, Pilot Projects, Prospective Studies, Heart Ventricles, Intention to Treat Analysis, Functional Status, Bundle of His, Bundle-Branch Block, Cardiomyopathies, Natriuretic Peptide, Brain, Stroke Volume, Follow-Up Studies, Ventricular Function, Left, Electrocardiography, Heart Failure, Echocardiography
< Back to Listings