Cover Story | Collaborative Care a Critical Piece in the Hypertension Puzzle
Elevated blood pressure (BP) is a major modifiable risk factor for stroke and cardiovascular disease. Yet progress on controlling hypertension and reducing death and disability from stroke and cardiovascular disease has stalled.
Hypertension affects nearly half of all adults in the U.S., based on the ACC/AHA guideline definition of a systolic BP >130 mm Hg on two separate occasions or taking antihypertensive drugs. Only about one in four adults have BP that is well controlled and many more remain unaware they even have hypertension.1
With so much on the line for the health of so many individuals, along with clear indications that the standard physician-led, office-based approach to BP control lacks real-world effectiveness, a fresh approach that involves coordinated effort among various health care professionals to provide comprehensive and patient-centered care is well worth considering.
"We as physicians have come to think we need to be able to tackle everything. One thing we need to recognize is that medicine is so complicated that if we try to address everything, we may end up addressing nothing," says Joseph E. Ebinger, MD, FACC, from Cedars-Sinai Medical Center in Los Angeles.
"How do we ensure all aspects of patient care are taken care of? Leverage the team around us, and make sure we're allowing all individuals to contribute to helping our patients gain control of their BP."
It Takes a Village
Team-based care engages health professionals across the spectrum, including physicians, pharmacists, PAs, nurses, dietitians, social workers, behavioral health, lay care coordinators and more to deliver comprehensive, effective care. This collaborative approach improves communication and coordination among team members and provides better opportunities to engage patients in their own care, resulting in personalized, timely, empowered and protocol-driven care.
– Donald (Trey) Clark III, MD, MPH
Most importantly, hypertension management that involves two or more caregivers (e.g., pharmacist and nurse) improves BP control over usual care, as shown in several studies and systematic reviews.2 Collaborative care also appears to be particularly effective in underresourced settings serving underrepresented racial and ethnic minority groups who are disproportionately impacted by hypertension.
In a large systematic review and meta-analysis, team-based care with nonphysician medication titration (−7.1 mm Hg decrease in systolic BP) and team-based care with physician medication titration (−6.2 mm Hg) were both found to be effective.3 So were strategies that targeted more than one of the typical barriers to hypertension control (e.g., lack of adherence to guidelines by physicians or lack of adherence to treatment by patients) but did not qualify as team-based care (−5.0 mm Hg). These included approaches like patient health coaching combined with provider training (Figure).

Notably effective patient-level strategies included health coaching (−3.9 mm Hg) and home BP monitoring (−2.7 mm Hg). Similar trends were observed for diastolic BP.
The meta-analysis, which included 121 comparisons from 100 published articles and encompassed data from 55,920 patients, found that multilevel multicomponent strategies were the most effective for systolic BP reduction.
– Joseph E. Ebinger, MD, FACC
While the meta-analyses to date reveal only modest reductions in systolic and diastolic BP with team-based care, an examination of individual programs tailoring specific interventions to specific populations demonstrate better effectiveness (see sidebar "Trimming Risk For Black Men").
One example is a study conducted by Donald (Trey) Clark III, MD, MPH, and colleagues from the University of Mississippi Medical Center, that combined home blood pressure monitoring (HBPM) with remote pharmacist-led hypertension management.4

The Economics Support Team-Based Care
Hypertension in 2021 was a primary or contributing cause of 691,095 deaths in the U.S. and the condition is estimated to cost the U.S. more than $130 billion each year. Clearly, a large number of health care dollars and lives can be saved with better BP control.6
A just-published economic evaluation showed both cost-effectiveness for team-based care and significant health benefit.7
The analysis, encompassing 35 studies from January 2011 to January 2021 in the U.S. and other high-income countries, showed a median team-based care intervention cost per patient per year of $438 for U.S. studies and $299 for all studies. Cost-effectiveness was readily shown with a median cost per quality-adjusted life year (QALY) gained of $12,897 for U.S. studies and $15,202 for all studies, both of which were well below the conservative threshold for cost-effectiveness of $50,000.
Modeled nationwide, a pharmacist-led team-based intervention could prevent 22.9 to 36.8 million person-years of uncontrolled BP and 77,200 to 230,900 heart attacks and strokes over five years. In 20 years, these numbers increased to preventing 83.8 to 174.8 million person-years of uncontrolled BP and 393,200 to 922,900 heart attacks and strokes, respectively.

Implementation among patients with persistently uncontrolled BP showed the most significant health and economic benefits. For instance, in patients with persistent, uncontrolled hypertension, (defined as SBP >140 mm Hg for ≥one year), team care reduced myocardial infarctions by 91,900, strokes by 139,000 and cardiovascular disease deaths by 115,400 over five years. The net cost per person enrolled with uncontrolled hypertension was about half the cost for newly diagnosed hypertension ($322).
Individuals with uncontrolled BP were provided an iPad tablet and a Bluetooth BP monitor and instructed on how to properly measure their BP at home, says Clark. Readings were transmitted directly to an electronic medical record (EMR), which was reviewed every three weeks by a clinical pharmacist. Medication changes were made according to a prespecified algorithm based on current guidelines and were communicated to the patient's primary care team through the EMR.
At six months, with more than 85% of participants completing the study protocol, the mean reduction in systolic and diastolic BP change from baseline was 14.1 mm Hg and 7.9 mm Hg, respectively (both p<0.001).
"A landmark study that showed HBPM with pharmacist case management was superior to usual care was reported in 2013 by Margolis and colleagues, but that study was in a mostly White population in an integrated health system.5 We wanted to know if this approach can be applied to a rural low-income minority population," says Clark.
Of the 120 participants in their study, 59.2% were Black, 65% were women, 27.5% did not complete high school and 46.7% reported an annual household income <$30,000. Participants lived a mean of 33 miles from the hypertension clinic and 29.2% resided in a federally designated rural county.
"Our findings are consistent with a lot of the other work showing that if you monitor BP and you connect it with a prespecified protocol that can be applied either by a nurse or pharmacist, it tends to be a better way to manage hypertension," says Clark. He emphasizes the importance of combining monitoring and protocol-driven medication titration to achieve the best results.
– Joseph E. Ebinger, MD, FACC
"It's important to get accurate BP measures, whether at home or in the office. But what I think really makes a difference is having an established protocol, so the numbers are acted on by whomever is given the responsibility for medication management." In fact, part of a team-based strategy, he notes, should be to formally define who is responsible for antihypertensive medication management.
Providing Better Care Today
"Managing hypertension is a team sport," says Ebinger. "No matter your practice setting, every member of the health care team that your patients interact with can and should be engaged in helping patients gain control of their BP."
This engagement might mean leveraging a nurse who has been trained in motivational interviewing around medical adherence or leveraging a pharmacist to help identify potential drug-drug interactions that may cause side effects and reduce adherence, he adds.
"Team care is about valuing all the care team members and allowing everyone to practice at the top of their license," says Leslie L. Davis, PhD, RN, FACC. Importantly, she adds, there is no one approach that appears to offer a magic bullet. Rather, each clinician needs to assess the capabilities and capacity of their team and then develop a process that works for them.
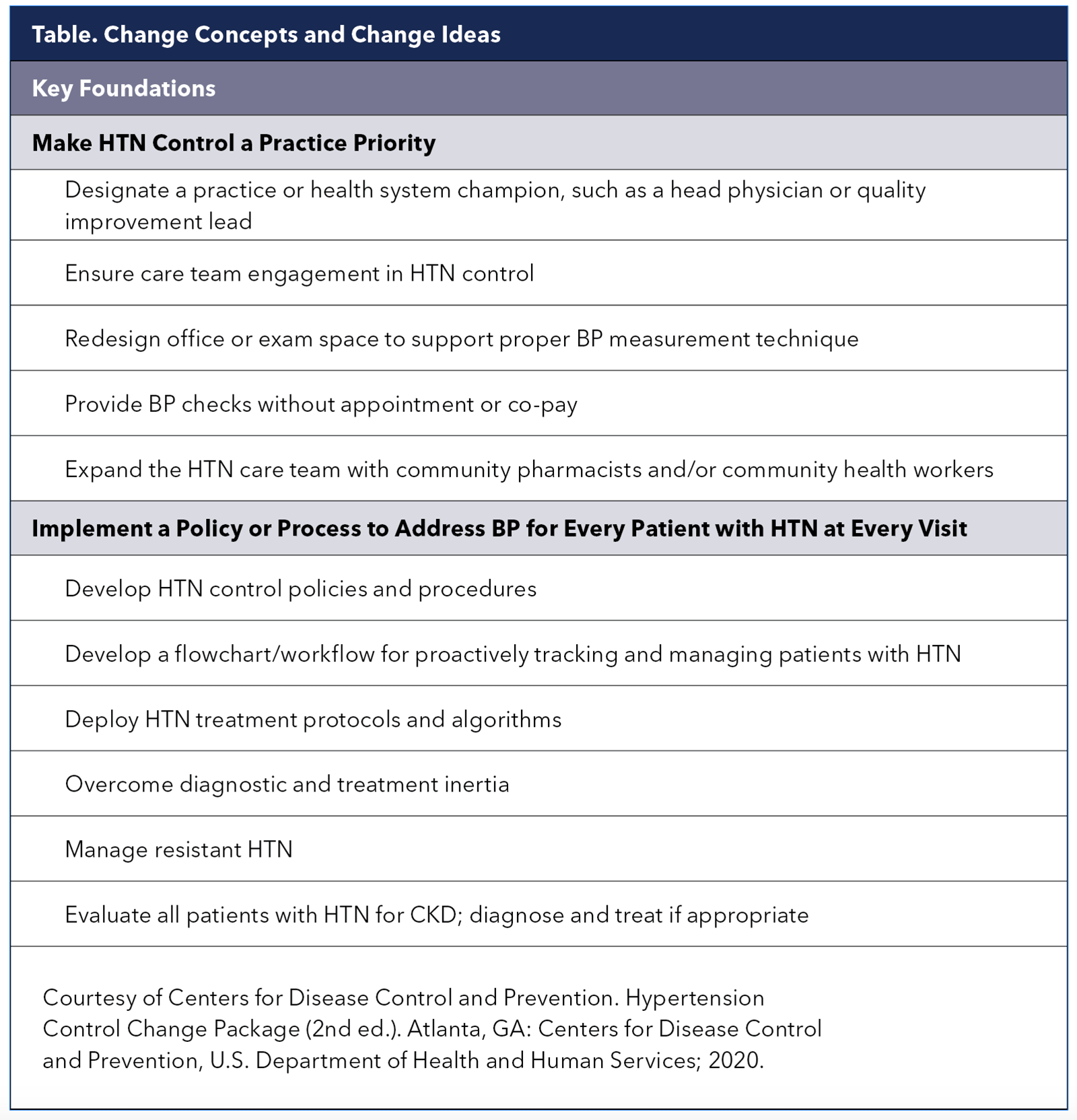
Help with process improvement appropriate for outpatient clinical settings to promote better BP control is available through the Million Hearts initiative's "Hypertension Control Change Package." Along with key foundations to establish strategies to prioritize hypertension control at the practice level (Table 1), it also offers strategies for equipping care teams, population health management and individual patient supports.
 Available here.
Available here.
"Part of making hypertension a practice priority is making it salient for people. Patients might know they have high BP, but very often they don't understand the contribution of BP to stroke, heart attack and all the rest. I try to provide them with insight about why I am so worried about their high BP and the impact it can have on them," says Ebinger.
Ebinger also makes sure patients with hypertension have scheduled follow-up. "Regular follow-up helps keep them engaged, monitoring their BP, monitoring their diet and sodium intake, and so on," he adds.
Proper measurement of BP too often remains a challenge, even in cardiology practices, says Davis. The first thing her team does in the hypertension clinic at the University of North Carolina is ensure that patients have proper BP measurement in the office and know how to monitor their BP properly at home, if only to understand if the patient has difficult to control hypertension or truly resistant hypertension.
"I know everyone has heard it a million times, but it bears repeating: if you're not measuring BP properly, you need to start doing that," says Davis, who is a professor of nursing, board certified nurse practitioner, and an American Society of Hypertension-certified hypertension clinician.
– Leslie L. Davis, PhD, RN, FACC
This means regular staff meetings, "at least quarterly," to ensure that everyone who measures BP is properly trained on best practices endorsed by the ACC/AHA guideline. "With labor shortages and the amount of turnover in many practices today, it's really important to stay on top of making sure all your rooming staff is measuring BP properly."
Perhaps key to better collaborative care of patients with hypertension and, in fact, many other lifestyle-based risk factors, is creating that meaningful connection that compels greater self-care, adherence and focus. This is reinforced with insights from a qualitative analysis of interviews with participants in the Barbershop study that Ebinger's group presented at ACC.23.
"We found that the secret sauce behind the success of that program was, first of all, the relationship between the men and their barbers. These are relationships rooted in trust so having an interaction in the barbershop with a member of the health care community – a person their barber is vouching for in the moment – really helped people get engaged in their own care. And that's where the magic happens."
Trimming Risk For Black Men

As with so much else, hypertension and its related health consequences disproportionately affect Black American men and women. Indeed, the prevalence of hypertension in Black people in the U.S. is among the highest in the world, at 55.85% and 56.9% for non-Hispanic Black men and women, respectively (vs. 54.2% and 45.4% for men and women, overall).8
Recognizing the marked disparities in hypertension care among Black men, the Los Angeles Barbershop Blood Pressure Study, conceived and first led by Ronald G. Victor, MD, screened men in Black-owned barbershops and enrolled those with systolic BP levels ≥140 mm Hg.
In some shops, barbers promoted follow-up with specialty-trained pharmacists (intervention group), whereas in other shops, barbers were trained to encourage lifestyle modification and doctor appointments (control group).
In the intervention group, two full-time doctorate-level ASH-certified pharmacists met regularly with participants at the barbershops and prescribed and monitored an antihypertensive drug regimen and encouraged lifestyle changes.
The pharmacist-led program significantly improved BP control with a mean BP reduction of 21 mm Hg vs. usual care at six months.9 Retention in the study was 95% and a BP level <130/80 mm Hg was achieved among 63.6% of participants vs. 11.7% of controls (p<0.001).
Importantly, these benefits were maintained at 12 months.10 At 10 years, the intervention was projected to cost an average of $2,356 more per participant than the control arm and gain 0.06 QALYs.11
The barbershop-based, pharmacist-led intervention was deemed cost-effective, with a mean cost of $42,717 per QALY gained, falling to $17,162 if only generic drugs were used. The investigators even found ways to make the program more efficient, by substituting virtual visits for in-person visits after BP control was achieved.
Scaling up the barbershop program across the U.S. using a cardiovascular risk model and projecting outcomes and costs over 10 years could avert 8,600 major cardiovascular events annually at an implementation cost of ≤$1,440 per patient-year enrolled.12 The program could potentially benefit about 941,000 Black men annually.
Pro Tips to Measure BP Correctly

Cuff size and many other factors affect proper BP measurement. Click here for an expert analysis and table of best practices for training the entire team.
Learn More at ACC.24
Take advantage of ACC.24 in Atlanta this April to get up to speed on the latest clinical guidance related to hypertension and BP management. Also, don't miss the chance to honor Suzanne Oparil, MD, FACC, during Convocation when she receives the 2024 Lifetime Achievement award for her pioneering contributions to the hypertension field. And stay for the party celebrating ACC's 75th anniversary. Visit ACCScientificSession.ACC.org to register today!

Understanding Hypertension Among Hispanic Americans
Hispanic Americans constitute the largest ethnic minority in the U.S., representing roughly 20% of the population. However, this diverse group is not homogeneous when it comes to hypertension.
"Traditionally, Hispanics have been aggregated into one group despite the fact that the Hispanic population in the U.S. is highly heterogeneous," says Tali Elfassy, PhD, an epidemiologist from the University of Miami, Miller School of Medicine in Florida. "They come from Central America, South America and the Caribbean – all regions with very different customs and cultures, as well as different racial backgrounds.
Most epidemiological studies tend to either lump all Hispanic groups together or focus mainly on Mexican Americans, the largest Hispanic subgroup in the U.S.
Elfassy's research leveraged data from the Hispanic Community Health Study/Study of Latinos, and sheds light on the varying incidence of hypertension among Hispanic/Latino individuals.15
The study analyzed 6,171 participants aged 18 to 74 years who were initially free from hypertension during the period of 2008-2011 and were reexamined during the period of 2014-2017.
A striking finding was the higher incidence of hypertension among Caribbean Hispanics, with men of Cuban and Dominican descent having a 27.1% and 28.1% age-adjusted probability of developing hypertension, respectively. This contrasted with a 17.6% age-adjusted probability among Mexican American men.
Women showed similar trends, with Cuban (22.6%) and Puerto Rican (23.3%) women having a higher likelihood compared with their Mexican American counterparts (16.0%).
One explanation could lie in the genetic makeup, as Caribbean Hispanics often have a higher degree of African admixture. However, Elfassy points out that genetics account for only about 1% of the variability in BP. Instead, she suggests that social and psychosocial factors, or "racialized aspects of life" may play a more substantial role in predisposing individuals to hypertension.
"It's possible that darker skin Hispanics have a much different experience than lighter skinned Hispanics and may be more prone to race-based discrimination based on skin color, which we know in and of itself is a very powerful contributor to high BP and could partially explain the higher rates of hypertension seen in Caribbean Hispanics."
Elfassy's study is a call to action for culturally sensitive health care approaches to manage and prevent hypertension, ensuring that the largest ethnic minority in the U.S. receives the nuanced care it requires. For physicians, recognizing these distinctions is essential to target prevention and treatment more effectively, improving patient outcomes and reducing health disparities.
Don't Forget Rehab!

Medicare covers cardiac rehab for referred patients who have had a recent acute myocardial infarction, PCI, CABG or valvular surgery; a recent episode of decompensated systolic heart failure or stable angina with symptoms. Yet too many patients aren't being sent to rehab, says Sherrie Khadanga, MD, director of cardiac rehabilitation at the University of Vermont Medical Center.
"There is still a lot of physician bias, particularly against older women, because their physicians think they are too frail to exercise so they don't send them for cardiac rehab," says Khadanga.
Those referred benefit from, among other things, a prime opportunity to get their hypertension better controlled. Indeed, suggested exit criteria for cardiac rehab are resting BP and heart rate within normal limits.
"One thing we do in cardiac rehab – and keep in mind we're seeing patients up to twice a week – is measure and log their BP as soon as they walk through the door. If we notice a trend, we can either change their medications ourselves or send them back to primary care or their cardiologist to make medication changes," says Khadanga.
Particularly in patients post PCI or post heart failure decompensation, maintaining good BP levels is important. "It's important to tailor your treatment to the situation. Some patients really should not be left uncontrolled for long periods of time," she adds.
Cuffless BP Monitoring

Finger-cuff devices, wristband wearables and other cuffless BP measuring devices represent an exciting advance in medical technology. Their allure is obvious: continuous, 24-hour BP monitoring provides a far more comprehensive picture of a patient's cardiovascular health compared with random office measures and can increase adherence with BP monitoring and management. However, at this time, the lack of rigorous validation means cuffless devices are not recommended for HBPM.14
"There are hundreds of wearable devices on the market that claim to measure BP, but none of them have been properly validated and accuracy and reliability have been a challenge," says Eugene Yang, MD, FACC, from the University of Washington School of Medicine.
Yang, who is also chair of the ACC Prevention of Cardiovascular Disease Section, is conducting research on cuffless BP monitors. He says while cuffless devices are "cleared" for use based on a 501K submission to the U.S. Food and Drug Administration (FDA), they are not "validated" – a nuance he suggests many patients don't fully understand.
"FDA clearance basically means that you meet the standards of devices that are similar and have already been approved, which in this case means cuff-based BP measures," he says. But he explains that the validation protocols used were not tailored to cuffless devices and, in fact, are not adequate for testing cuffless devices. "The assumption is that the technologies are very similar, which in this case is not true, so it's not comparing apples to apples but rather apples to oranges."
Yang says that, for now, clinicians need to emphasize to patients that none of the cuffless devices have been put through rigorous validation protocols and should be used with caution. Yet, he still has hopes for overcoming the challenges in the years to come.
"I'm a technology person, so I'm very excited about cuffless BP devices. Some colleagues don't think we'll overcome some of the barriers. I think eventually we'll figure out how to make the technology accurate and we'll be able to validate it," he says.
Two websites provide lists of validated BP monitors for home use: validatebp.org, initiated by the American Medical Association, and stridebp.org, which is affiliated with the European Society of Hypertension, International Society of Hypertension and World Hypertension League.
This article was authored by Debra L. Beck, MSc.
References
- Centers for Disease Control and Prevention. Million Hearts. Estimated hypertension prevalence, treatment, and control among US adults. May 12, 2023. Accessed Jan. 2, 2024. Available here.
- Abdalla M, Bolen SD, Brettler J, et al. Implementation strategies to improve blood pressure control in the United States: A scientific statement from the American Heart Association and American Medical Association. Hypertens 1979;2023;80:e143-e157.
- Mills KT, Obst KM, Shen W, et al. Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients: A systematic review and meta-analysis. Ann Intern Med 2018;168:110-20.
- Clark D, Woods J, Zhang Y, et al. Home blood pressure telemonitoring with remote hypertension management in a rural and low-income population. Hypertens 2021;78:1927-9.
- Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013;310:46-56.
- Centers for Disease Control and Prevention. Facts About Hypertension. July 6, 2023. Accessed Jan. 4, 2024. Available here.
- Jacob V, Reynolds JA, Chattopadhyay SK, et al. Economics of team-based care for blood pressure control: Updated community guide systematic review. Am J Prev Med 2023;65:735-54.
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Nov. 20, 2023. Accessed Nov. 29, 2023. Available here.
- Victor RG, Lynch K, Li N, et al. A cluster-randomized trial of blood-pressure reduction in Black barbershops. N Engl J Med 2018;378:1291-1301.
- Victor RG, Blyler CA, Li N, et al. Sustainability of blood pressure reduction in Black barbershops. Circulation 2019;139:10-9.
- Bryant KB, Moran AE, Kazi DS, et al. Cost-effectiveness of hypertension treatment by pharmacists in Black barbershops. Circulation 2021;143:2384-94.
- Kazi DS, Wei PC, Penko J, et al. Scaling up pharmacist-led blood pressure control programs in Black barbershops: Projected population health impact and value. Circulation 2021;143:2406-8.
- Stergiou GS, Mukkamala R, Avolio A, et al. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens 2022;40:1449-60.
- Elfassy T, Al Hazzouri Z A, Cai J, et al. Incidence of hypertension among US Hispanics/Latinos: The Hispanic community health study/study of Latinos, 2008 to 2017. J Am Heart Assoc 2020;912:e015031.
Clinical Topics: Prevention, Hypertension
Keywords: Cardiology Magazine, ACC Publications, Antihypertensive Agents, Blood Pressure, Hypertension, Stroke
< Back to Listings