From the Member Sections | Navigating the Future: Congenital Heart Disease Care From Childhood to Adulthood

February marks Congenital Heart Defect Awareness Week, an opportunity to reflect on the remarkable advancements in the care for congenital heart disease (CHD). Historically viewed with a grim outlook, CHD has journeyed from a potentially lethal condition to a chronic disease managed into adulthood.
A Look Back at CHD Care
Decades ago, CHD care was nearly synonymous with palliative care. Many individuals with moderate to severe CHD rarely survived past childhood. However, advancements in diagnosis, surgical interventions and comprehensive care strategies have significantly changed the landscape. Over the last half-century, there have been three major revolutionary innovations and paradigm shifts in CHD interventions that have fundamentally altered the prognosis and quality of life for individuals with CHD. These innovations include the heart-lung (cardiopulmonary bypass) machine, neonatal cardiac surgery and transcatheter therapy.
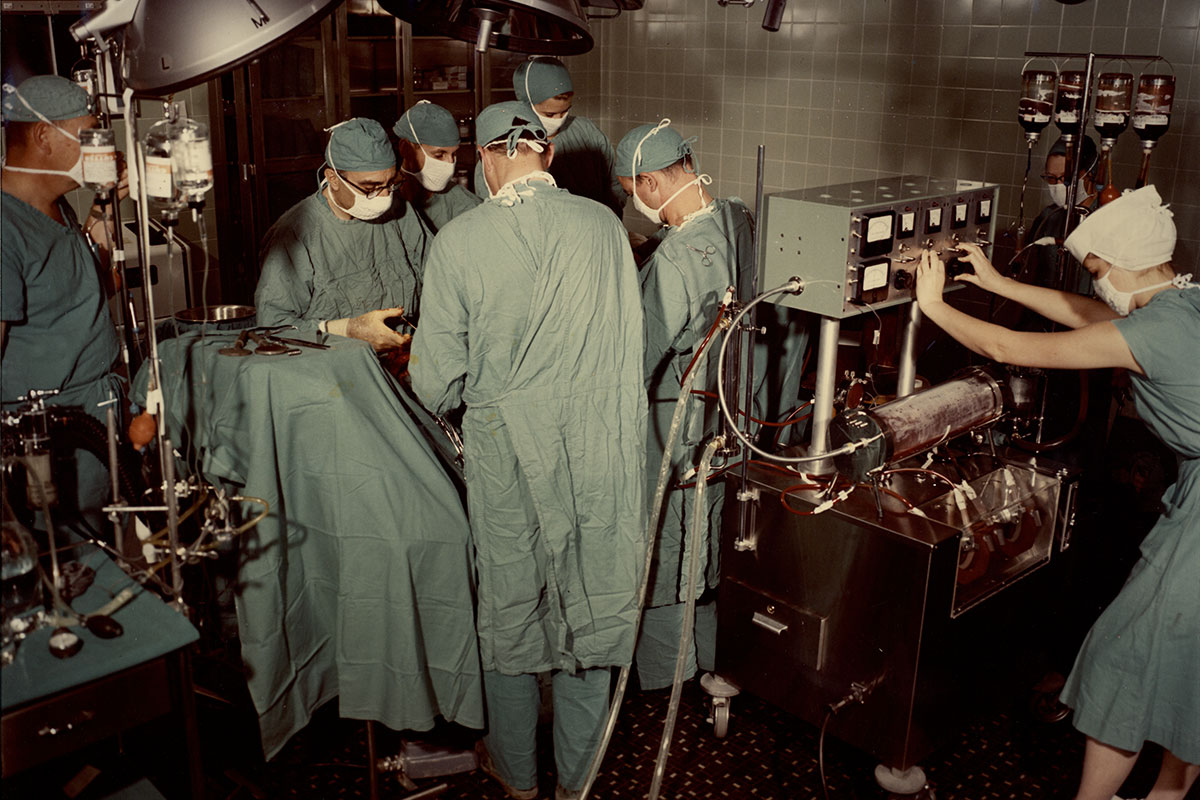 Credit: National Library of Medicine
Credit: National Library of Medicine
The heart-lung machine, introduced in the mid-1950s, marked the birth of modern cardiac surgery and the specialization of CHD treatment. This machine allowed for more complex and precise surgeries, vastly improving the outcomes of CHD interventions. For instance, the first intracardiac surgical procedure was performed in 1952 using the caval inflow occlusion technique, followed by the repair of several moderately complex CHD diagnoses using the cross-circulation technique. These early successes paved the way for the widespread establishment of open-heart surgical centers and the development of innovative surgical techniques for more complex lesions, such as the Senning operation, Mustard operation and Fontan operation.
Neonatal cardiac surgery was another pivotal innovation, allowing primary repair of complex congenital heart defects in infants, significantly reducing the need for staged surgical repair and its associated morbidity and mortality. The first successful transcatheter cardiac procedures, including balloon atrial septostomy and atrial septal defect closure, opened a new frontier in CHD interventions, offering less invasive options with quicker recovery times and less overall risk.
These advances have been accompanied by significant improvements in perioperative anesthesia and monitoring, neonatal and pediatric critical care, fetal echocardiography and interventions, echocardiography and cross-sectional imaging. The rise of biobanking, electronic health records and machine learning offer new avenues for personalized care and more efficient management of the disease. These advancements not only improve life expectancy but also the quality of life for those affected. As a result, the subspecialty of adult congenital heart disease has emerged, catering to the growing population of adults living with CHD.
Today, the increasing number of adults living with CHD reflects a demographic shift and underscores the success of medical advancements in extending lives.
The Transition Challenge: Pediatric to Adult-Oriented Care

The success in pediatric care necessitates a robust transition into adult health care systems. This transition is more than a mere transfer of care; it's a critical evolution in the patient's journey, requiring the development of autonomy in health management. Programs aimed at facilitating this transition focus on enhancing knowledge, self-management and the gradual shift of responsibility from caregivers to the individual. Despite these efforts, many gaps and challenges remain, particularly for underserved populations. Addressing these gaps is vital for the continuity and quality of care.
Societal and Individual Impact
The burgeoning population of adults with CHD represents both a triumph and a challenge. On one hand, it's a testament to the progress in medical care. On the other hand, it presents new complexities in managing long-term health, particularly as these individuals age and acquire additional comorbidities. The societal implications are profound, affecting public health planning, resource allocation and health care policy. For individuals, the continuous evolution in care means adapting to new challenges and maintaining an ongoing relationship with health care systems.
Looking Ahead: Future Directions in CHD Care
The future of CHD care is bright with possibilities. Ongoing research continues to push the boundaries of what's possible in treatment and management. Transition programs are becoming more sophisticated, integrating psychological support, digital tools and customized care plans. The role of artificial intelligence in predictive analytics, personalized medicine and patient management is expanding, offering the potential to revolutionize CHD care further.
Emphasizing a Multidisciplinary Approach
The complexity of CHD care necessitates a multidisciplinary approach. Cardiologists, surgeons, nurses, social workers and other health care professionals must collaborate to provide comprehensive care. This team approach ensures that all aspects of a patient's health are addressed, from the physical to the psychological, enhancing the overall treatment outcome.
Addressing Disparities and Ensuring Equity in Care
As we advance CHD care, addressing disparities in access and outcomes becomes increasingly important. Social determinants of health such as socioeconomic status, race and geographic location can significantly impact the quality and continuity of care. Efforts must be made to understand and mitigate these disparities, ensuring that all individuals with CHD have the opportunity for optimal health outcomes.
In summary, the journey of CHD care is a testament to the resilience of patients and the relentless progress of medical science. From a once fatal diagnosis to a manageable chronic condition, CHD care has come a long way. As we look to the future, our focus must remain on innovation, collaboration and a commitment to equity. By building on our past successes and pushing forward with new research and comprehensive care strategies, we can continue to improve the lives of those affected by CHD. As we mark the awareness week, let us renew our dedication to the CHD community, celebrating how far we have come and looking forward with hope to the future. Together, we can ensure that individuals with CHD lead fuller, healthier lives.

This article was authored by Tarek Alsaied, MD, FACC, on behalf of the Adult Congenital and Pediatric Cardiology Member Section, of which he is chair of the Communication and Publication Committee. He is a pediatric cardiologist at the UPMC Children's Hospital of Pittsburg, PA, where he is also an assistant professor of pediatrics.
Click here to learn more about the ACPC Section.
Clinical Topics: Congenital Heart Disease and Pediatric Cardiology, Noninvasive Imaging, Congenital Heart Disease, CHD and Pediatrics and Imaging, Echocardiography/Ultrasound
Keywords: Cardiology Magazine, ACC Publications, Heart Defects, Congenital, Cardiopulmonary Bypass, Echocardiography, Chronic Disease, Heart Septal Defects, Atrial