Feature | Rethinking the Meaning of IHD: Invasive Assessment of ANOCA

Ischemic cardiovascular disease (IHD) continues to be a significant public health problem in the U.S. Typically, ischemia is associated with epicardial coronary artery obstruction caused by atherosclerotic plaque.1 Angina pectoris, the most common symptom of IHD, affects approximately 112 million people globally.2
However, in up to two-thirds of patients undergoing coronary angiography because of angina and evidence of myocardial ischemia, there is no proof of obstructive coronary artery diseases (CAD).3
In the past, many of these patients would then receive a clean cardiovascular bill of health, and a diagnostic pathway to identify possible noncardiac etiologies was often sought. The link between angina, myocardial ischemia and underlying coronary flow abnormalities in the absence of obstructive CAD has, thankfully, finally been established and multiple clinical phenotypes have been identified.
The most common phenotypes are angina and nonobstructive coronary arteries (ANOCA) and ischemia with nonobstructive coronary arteries (INOCA). Coronary microvascular dysfunction (CMD) and epicardial vascular dysfunction are frequent pathophysiologic etiologies of ANOCA/INOCA and nonobstructive IHD.4
ANOCA or INOCA?
Fundamentally, a mismatch of oxygen supply and demand may lead to transient or recurrent cardiac chest pain related to ischemia due to inadequate cellular availability of adenosine-5'-triphosphate.5 Although obstructive CAD is a frequent and well-acknowledged cause of myocardial ischemia, many stenoses judged as severe on visual assessment are not flow-limiting.6,7
ANOCA/INOCA are familiar yet under-addressed clinical entities. Diagnosis and management of ANOCA/INOCA have presented challenges for physicians: treatment does not follow guideline-directed clinical pathways for obstructive atherosclerotic disease; diagnosis requires new systems and techniques; and data are limited regarding the relationships between various treatments and outcomes.8
The Microvascular Network is a community of physicians and advanced practice providers (academic and community-based) focused on developing a common language and standardized strategy for advancing the diagnosis and treatment of patients with microvascular dysfunction and associated coronary disorders.
Recently this group suggested the term ANOCA may be preferred to INOCA because, while ischemia is implied, it may not be readily identified (although a recently published article in JACC raises the possibility that stress testing may be more valuable in these situations than previously believed).9
While evidence of obstructive CAD or regional inducible myocardial ischemia may be seen on traditional nuclear stress testing and anatomic imaging with coronary computed tomography angiography (CCTA), their presence does not exclude the presence of CMD, coronary vasospasm or a hemodynamically significant myocardial bridge in symptomatic patients.10,11
CMD, believed to be present in at least half of ANOCA/INOCA cases, is defined as endothelial dysfunction, vascular smooth muscle, or both.4 Additionally, increased epicardial or microvascular coronary vasoreactivity is present in approximately 25% of these patients.1
Comprehensive Assessment of ANOCA
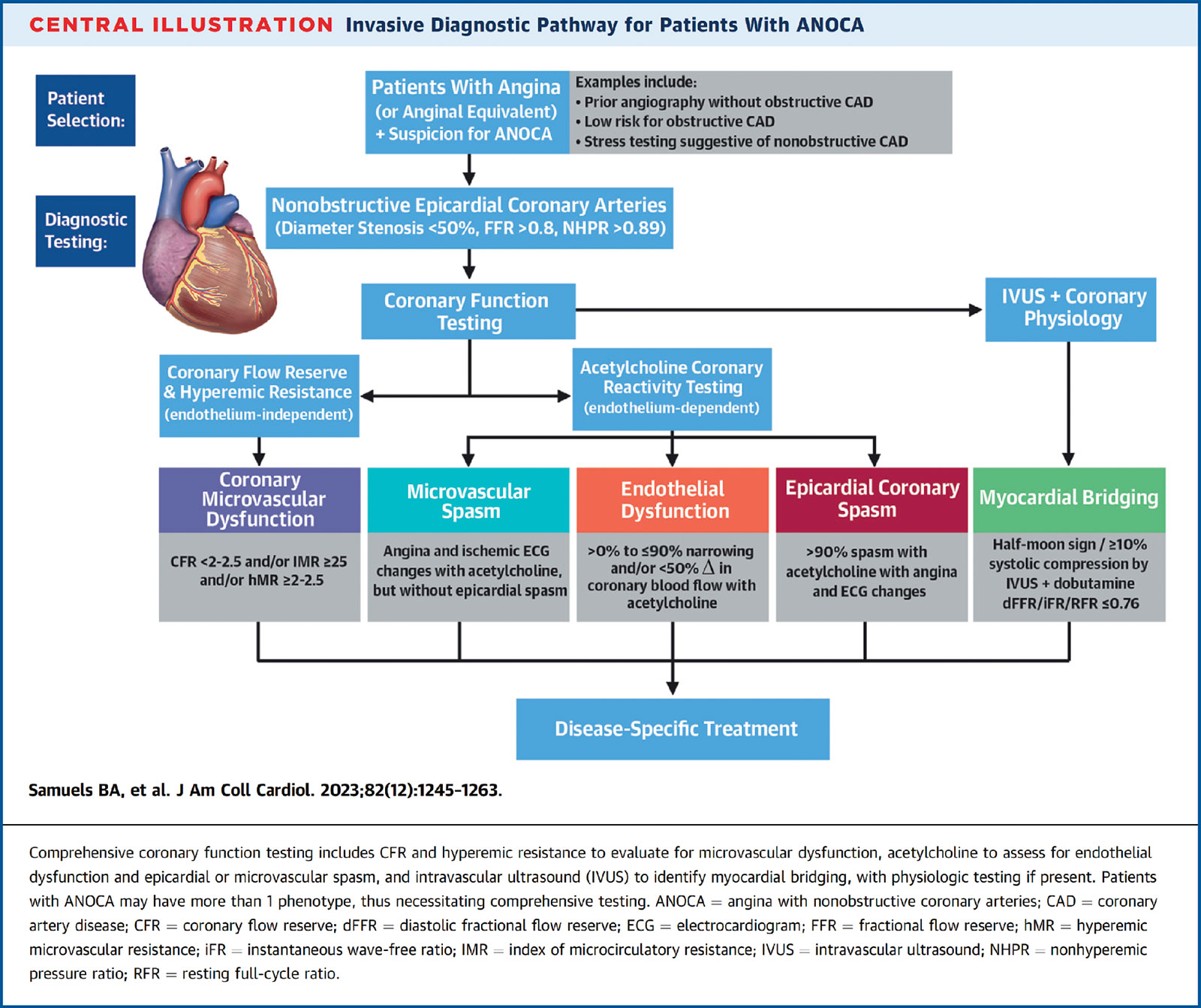
The comprehensive assessment of ANOCA should be tailored to testing the microcirculation for evidence of CMD, endothelial dysfunction and increased vasoreactivity, as well as, in some patients, determining the potential contribution of a myocardial bridge to the patient's symptoms.
Testing for CMD is performed with an endothelial-independent vasodilator such as adenosine to induce hyperemia, whereas testing for endothelial dysfunction and vasospasm (microvascular and epicardial) is performed with an endothelium-dependent vasodilator such as acetylcholine (Ach). Because myocardial bridging is often missed by angiography alone, intravascular imaging (or advanced CCTA) is needed for detection, as well as to obtain critical anatomical measurements. If bridging is present, hemodynamic significance can be assessed with dobutamine stress and a flow wire.8
Coronary flow wire technology has made it possible to perform testing during invasive coronary angiography that can more reliably assess patients with ANOCA and provide the specific etiology of anginal symptoms. Diagnostic options include coronary thermodilution using a pressure-temperature sensor guidewire (Pressure Wire X, Abbott Vascular, Santa Clara, CA, USA) or a Doppler technique (ComboWire, Philips Corporation, San Diego, CA, USA).3,8
Coronary flow reserve (CFR) can be calculated by using thermodilution or Doppler flow velocity. The optimal cutoff has been in the range of 2-2.5, depending on the system utilized.12,13
Microcirculatory resistance can be calculated by combining pressure and flow measurements. With a thermodilution system, the index of microvascular resistance (IMR) is calculated as the product of distal coronary pressure at maximal hyperemia multiplied by the hyperemic mean transit time.14 An IMR >25 is indicative of microvascular dysfunction. The hyperemic myocardial velocity resistance (hMR) index is a Doppler-based index calculated by dividing intracoronary pressure by hyperemic flow velocity. An hMR ≥2-2.5 indicates microvascular dysfunction.15,16
Details on the various interventional steps regarding coronary testing for ANOCA are described masterfully by the Microvascular Network in its JACC State-of-the-Art review (Figure).8 Ideally, patients should be counseled to discontinue caffeine, long-acting nitrates, beta-blockers, calcium-channel blockers, and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for ≥24 hours before the procedure.
This can make coronary functional testing challenging as an ad hoc procedure, particularly as the administration of intraarterial calcium-channel blockers is often routine during radial approach catheterization. With an increasing number of diagnostic angiograms being performed as "radial first," most patients undergoing angiography for angina/ischemia will likely receive a cocktail containing nitroglycerine and a calcium-channel blocker. The latter could, in theory, prevent vasospasm during vasoreactivity testing, making interpretation of results problematic.
Alternatives are to use nitroglycerine alone for radial catheterization, as it has a very short half-life, thus making it unlikely to affect the incidence of coronary spasm after >10 minutes following administration,17 or to perform femoral puncture. Decisions on vascular access must, then, be individualized on a patient-by-patient basis, weighing the individual risks and benefits, including the risk of significant radial artery spasm, vascular complications, bleeding complications, patient comfort, and the potential need for a repeat catheterization for a complete assessment of ANOCA.
While there are limited available randomized data examining an invasive approach to assessing coronary flow and vasoreactivity in individuals with angina and nonobstructive CAD, the CorMicA investigators demonstrated this strategy, coupled with medical therapy, led to a significant improvement in angina.18
Interpreting Findings From ANOCA Assessment
Distinct scenarios emerging from invasive assessment of patients with angina and suspected ANOCA are described by the European Association of Percutaneous Cardiovascular Interventions (EAPCI) expert consensus document on INOCA as well as the recent comprehensive review by the Microvascular Network.3,8 While the nomenclature differ between the two documents, the principles are the same (Table).
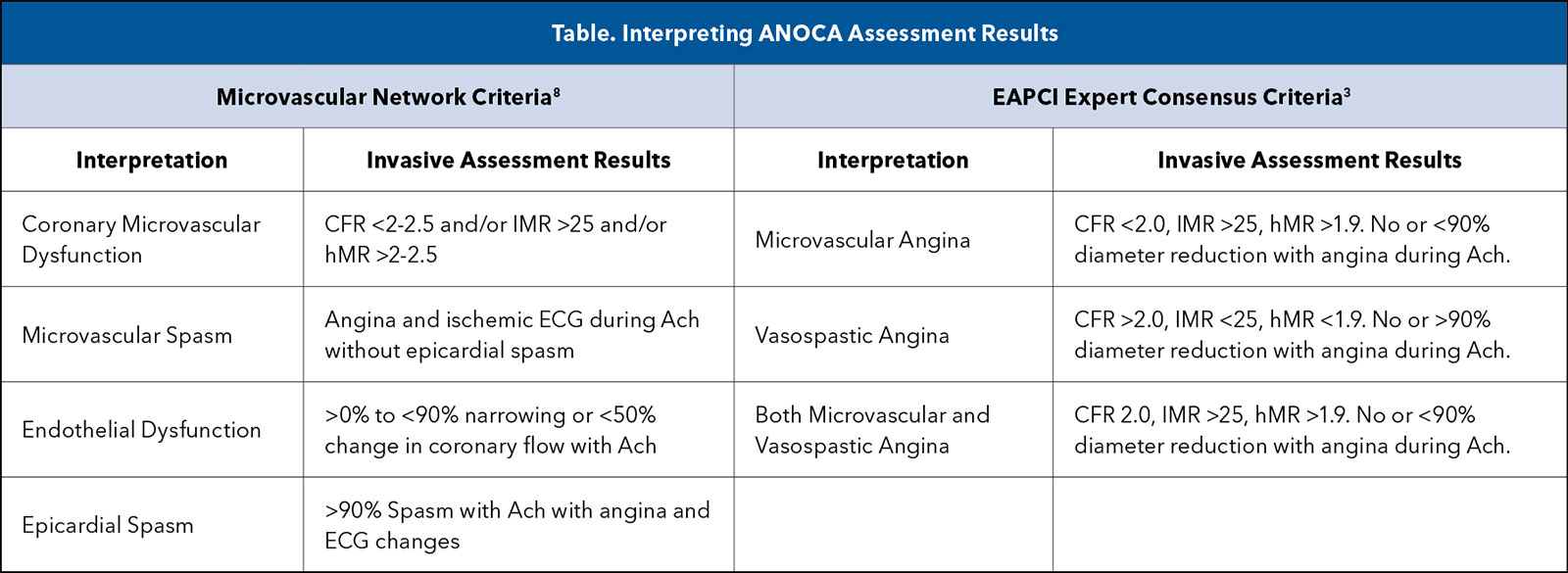
The Microvascular Network describes several scenarios based on the mechanistic explanation of findings when interpreting CFR/IMR. One, CMD, an endothelium-independent condition, is diagnosed for a CFR <2-2.5 and IMR ≥25 and/or hMR ≥2-2.5 (both abnormal).
Two, the opposite can also occur where both CFR and IMR are normal, indicating there is no evidence for disruption of endothelium-independent dilation of the coronary microvasculature. Lastly, isolated abnormalities of CFR and IMR can occur but are less well understood; their significance is not completely clear and requires further investigation.
Coronary vasoreactivity testing is frequently performed using an intracoronary infusion of Ach.18,19 Acetylcholine influences coronary vascular tone via muscarinic receptors on endothelial and vascular smooth muscle cells. This agent is helpful, as the presence of endothelial dysfunction and impaired release of nitric oxide results in smooth muscle-mediated constriction.20
The dose of Ach for coronary testing varies widely in the literature and in clinical practice (from very low doses to a very high dose of 200 mcg). Over a dozen protocols have been published. However, it is consistently administered via graded increases of administered Ach, monitoring of ECG and clinical symptoms, and performance of coronary angiography in a consistent view between doses to allow for assessment of epicardial spasm before dose escalation.
The Microvascular Network recommends starting an infusion dose of Ach at 20 mcg followed by another infusion dose of 100 mcg if necessary.8 Based on the responses to Ach infusion and the associated underlying pathophysiology, the Network proposed these diagnoses as the source of the angina:
- Microvascular Vasospasm: Ach-induced angina and ischemic ECG changes without angiographic evidence of epicardial coronary vasospasm.
- Epicardial Spasm: A >90% reduction in vessel diameter after infusion of Ach associated with angina and ECG change.
- Endothelial Dysfunction: A minor degree of vasospasm reduction (<90%) in coronary diameter.
Detecting and Characterizing Myocardial Bridging

Myocardial bridging is another underrecognized cause of angina in patients with ANOCA.8 Although usually visible during angiography, intravascular ultrasound (IVUS) is the gold standard, demonstrating compression >10% by invasive angiography.21
Taranini, et al., prospectively enrolled 20 patients with angina and/or positive noninvasive stress test, absence of significant coronary artery stenosis, and angiographic suspicion/evidence of myocardial bridge in the left anterior descending artery.22 All patients underwent functional intracoronary evaluation with fractional flow reserve (FFR) at rest and after dobutamine (up to 20 mcg) and atropine (1 mg) intravenous infusion.
Measurement of instantaneous wave-free ratio (iFR) at baseline and dobutamine-induced hyperemic wave-free period pressure ratio were also recorded. Their study suggests that physiological evaluation of a possible myocardial bridge with iFR seems more consistent with patient symptoms and noninvasive test results than FFR.
CCTA presents another noninvasive means for detecting and characterizing muscle bridging.23,24 The ability to assess structures adjacent to the coronaries, along with spatial resolution, provides a valuable diagnostic platform. The high incidence of detected muscle bridges by CCTA can present a challenge regarding functional significance.
The functional significance of a possible myocardial bridge can be evaluated by quantification of diastolic coronary flow parameters in the setting of intravenous dobutamine-induced myocardial stress. Intravenous dobutamine is administered using the accelerated dosing protocol used in the echocardiography laboratory: initial dobutamine dose of 20 mcg/kg/min, increasing to 40 mcg/kg/min after 3 minutes, and then increasing to 50 mcg/kg/min after another 3 minutes, with up to 1 mg of intravenous atropine as needed, to achieve at least 85% of the maximal age-predicted heart rate. Although validation is still needed, diastolic FFR/iFR/RFR ≤0.76 is currently considered hemodynamically significant.8,25
The Road Ahead to Address ANOCA
ANOCA is not a benign syndrome. Misdiagnosis and lack of appropriate patient counseling and treatment can be problematic. Patients presenting with angina may eventually undergo anatomic coronary imaging (invasive or noninvasive) documenting nonobstructive CAD. This may lead to noncardiac testing and therapies without an accurate diagnosis. Considerable evidence documents an increased risk of significant adverse outcomes in this population.1
Advances in clinical management have been guided by the efforts of expert writing groups, including the EAPCI and the Microvascular Network.3,8 Clinicians are now rethinking the diagnosis of ischemic heart disease, recognizing the importance of ANOCA for the correct diagnosis and management of patients. Further registry data and randomized trials are needed to pave the road toward more comprehensive management of these patients, however. In the interim, avoidance of labeling the angina patient with nonobstructive coronaries as "noncardiac" until clearly proven is crucial.


This article was authored by Ricardo O. Escárcega, MD, FACC, medical director, Cardiac Catheterization Laboratories; Richard A. Chazal, MD, MACC, medical director, Center for Quality/Transformation/Innovation; and Malissa J. Wood, MD, FACC, vice president and chief physician executive, all at Lee Health Heart Institute, Fort Myers, FL.
References
- Pepine CJ. ANOCA/INOCA/MINOCA: Open artery ischemia. Am Heart J Plus 2023;26.
- Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459-1544.
- Kunadian V, Chieffo A, Camici PG, et al. An EAPCI expert consensus document on ischaemia with nonobstructive coronary arteries in collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology and Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. EuroIntervention 2021;16:1049-69.
- Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med 2007;356:830-40.
- Ford TJ, Corcoran D, Berry C. Stable coronary syndromes: pathophysiology, diagnostic advances and therapeutic need. Heart 2018;104:284-92.
- Fearon WF, Nishi T, De Bruyne B, et al. Clinical outcomes and cost-effectiveness of fractional flow reserve-guided percutaneous coronary intervention in patients with stable coronary artery disease: Three-year follow-up of the FAME 2 Trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation). Circulation 2018;137:480-87.
- Ciccarelli G, Barbato E, Toth GG, et al. Angiography Versus hemodynamics to predict the natural history of coronary stenoses: Fractional flow reserve versus angiography in multivessel evaluation 2 substudy. Circulation 2018;137:1475-85.
- Samuels BA, Shah SM, Widmer RJ, et al. Comprehensive management of ANOCA, Part 1-Definition, Patient Population, and Diagnosis: JACC State-of-the-Art Review. J Am Coll Cardiol 2023;82:1245-63.
- Sinha A, Dutta U, Demir OM, et al. Rethinking false positive exercise electrocardiographic stress tests by assessing coronary microvascular function. J Am Coll Cardiol 2024;83:291-99.
- Lopez DM, Divakaran S, Gupta A, et al. Role of exercise treadmill testing in the assessment of coronary microvascular disease. JACC Cardiovasc Imaging 2022;15:312-21.
- Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol 2018;72:2625-41.
- Sara JD, Widmer RJ, Matsuzawa Y, et al. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC Cardiovasc Interv 2015;8:1445-53.
- Lee JM, Jung JH, Hwang D, et al. Coronary flow reserve and microcirculatory resistance in patients with intermediate coronary stenosis. J Am Coll Cardiol 2016;67:1158-69.
- Fearon WF, Balsam LB, Farouque HM, et al. Novel index for invasively assessing the coronary microcirculation. Circulation 2003;107:3129-32.
- Sheikh AR, Zeitz CJ, Rajendran S, et al. Clinical and coronary haemodynamic determinants of recurrent chest pain in patients without obstructive coronary artery disease - A pilot study. Int J Cardiol 2018;267:16-21.
- Williams RP, de Waard GA, De Silva K, et al. Doppler versus thermodilution-derived coronary microvascular resistance to predict coronary microvascular dysfunction in patients with acute myocardial infarction or stable angina pectoris. Am J Cardiol 2018;121:1-8.
- da Silva RL, de Andrade PB, Dangas G, et al. Randomized clinical trial on prevention of radial occlusion after transradial access using nitroglycerin: PATENS trial. JACC Cardiovasc Interv 2022;15:1009-18.
- Ford TJ, Stanley B, Good R, et al. Stratified medical therapy using invasive coronary function testing in angina: The CorMicA trial. J Am Coll Cardiol 2018;72:2841-55.
- Beltrame JF, Crea F, Kaski JC, et al. International standardization of diagnostic criteria for vasospastic angina. Eur Heart J 2017;38:2565-8.
- Davignon J, Ganz P. Role of endothelial dysfunction in atherosclerosis. Circulation 2004;109:III27-32.
- Tsujita K, Maehara A, Mintz GS, et al. Comparison of angiographic and intravascular ultrasonic detection of myocardial bridging of the left anterior descending coronary artery. Am J Cardiol 2008;102:1608-13.
- Tarantini G, Barioli A, Nai Fovino L ,et al. Unmasking myocardial bridge-related ischemia by intracoronary functional evaluation. Circ Cardiovasc Interv 2018;11:e006247.
- Nakanishi R, Rajani R, Ishikawa Y, et al. Myocardial bridging on coronary CTA: An innocent bystander or a culprit in myocardial infarction? J Cardiovasc Comput Tomogr 2012;6:3-13.
- Sternheim D, Power DA, Samtani R, et al. Myocardial bridging: diagnosis, functional assessment, and management: JACC state-of-the-art review. J Am Coll Cardiol 2021;78:2196-2212.
- Escaned J, Cortes J, Flores A, et al. Importance of diastolic fractional flow reserve and dobutamine challenge in physiologic assessment of myocardial bridging. J Am Coll Cardiol 2003;42:226-33.
Clinical Topics: Atherosclerotic Disease (CAD/PAD)
Keywords: Cardiology Magazine, ACC Publications, Ischemia, Coronary Artery Disease, Angina Pectoris, Plaque, Atherosclerotic, Cardiology Magazine Spotlight Series
< Back to Listings