Poll Results: To Ablate Atrial Fibrillation or Not in the Older Adult? A Geriatric Cardiology/Electrophysiology Dilemma
Brief Clinical Vignette. Mr. PT is an 82-year-old man who presents with persistent, mildly symptomatic atrial fibrillation (AF) of approximately 4-5 months' duration. He also has New York Heart Association (NYHA) class II heart failure with reduced ejection fraction and left ventricular ejection fraction (LVEF) 40%.
The aim of the first poll question was to ascertain which choice would be made for a man recognized to have AF of a duration of 4-5 months. A limited amount of information (chronological age, symptoms, LVEF, and NYHA class) was provided.
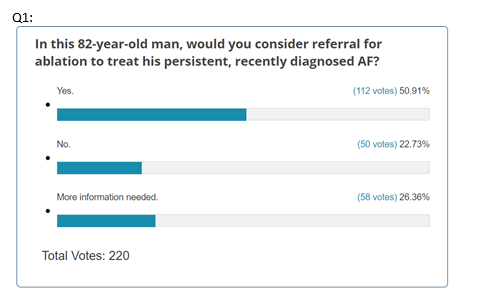
There was a robust response (n = 220). On the basis of the available data, approximately 50% of respondents stated they would consider referral for AF ablation. The other 50% was divided between no (meaning they would not consider referral) and more information needed.
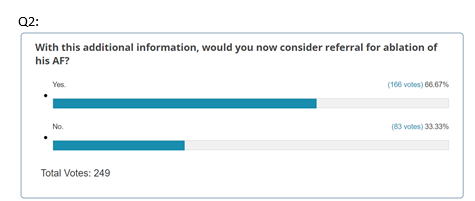
Following a more comprehensive vignette on the same patient, the question was again asked later in the poll. In addition to more detailed cardiac information, a comprehensive geriatric assessment (CGA) was presented. This CGA encompassed:
- Medical and cognitive domains. The medical domain (vision, hearing, gastrointestinal tract and genitourinary tract conditions, substance use, elder abuse, and whether there were recent falls,1 an extremely important condition that has been under-recognized, until recently, in the cardiovascular [CV] community)2 and cognitive domain (age-related memory changes, minor neurocognitive impairment, major neurocognitive impairment [also known as dementia]; other impairments, such as depression and delirium, also need to be considered).
- The presence of multimorbidity,3 a science of its own, was presented in the first paragraph of the expanded clinical vignette.
- Physical domain. An assessment of what a person can do in their daily life (activities of daily living [ADL], instrumental ADL, Nagi Rosow-Breslau activities, and frailty [a small component of the CGA]).
- Polypharmacy.4 The abundance of (prescription and over-the-counter) medications.
- This patient's abundance can be classified as hyperpolypharmacy (≥10 medications). Although hyperpolypharmacy was not the focus of this clinical vignette, it is important to recognize the role that polypharmacy (≥5 medications) and hyperpolypharmacy can play in altering expected CV and non-CV outcomes.
- Goals. Lastly, the patient's goals of care were discussed, albeit somewhat superficially.
- A more effective approach would involve setting SMART (specific, measurable, achievable, relevant, and time-bound) goals. For instance, committing to exercising with his spouse 4 days per week, covering 1 mi (1.6 km) each day, over the subsequent year would fulfill all SMART criteria. As advancements in the science of aligning treatment with physical and cognitive objectives progress, clinicians can aim to optimize this matching process.
- Missing items.
- Other variables that could potentially alter the appreciation of the potential success or failure of ablation (e.g., size or volume of the left atrium).
- Mechanistic details of the ablation (e.g., pulmonary vein isolation).
Interestingly and surprisingly, the results of the second poll question showed an increase from 50% to 67% with the new information, with a slight increase in the sample size (n = 249).
Does the evidence from randomized controlled trials consider the additional information obtained from the CGA?
Please see the excellent PRO/CON debate by Drs. Brian Olshansky and John Mandrola pertaining to this dilemma.
References
- Denfeld QE, Turrise S, MacLaughlin EJ, et al.; American Heart Association Cardiovascular Disease in Older Populations Committee of the Council on Clinical Cardiology and Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, Stroke Council. Preventing and managing falls in adults with cardiovascular disease: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes 2022;15:[ePub ahead of print].
- Gorodeski EZ, Goyal P, Hummel SL, et al.; Geriatric Cardiology Section Leadership Council, American College of Cardiology. Domain management approach to heart failure in the geriatric patient: present and future. J Am Coll Cardiol 2018;71:1921-36.
- Forman DE, Maurer MS, Boyd C, et al. Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol 2018;71:2149-61.
- Krishnaswami A, Steinman MA, Goyal P, et al.; Geriatric Cardiology Section Leadership Council, American College of Cardiology. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol 2019;73:2584-95.
Clinical Topics: Arrhythmias and Clinical EP, Geriatric Cardiology, Atrial Fibrillation/Supraventricular Arrhythmias, Heart Failure and Cardiomyopathies, Anticoagulation Management
Keywords: Ablation, Geriatrics, Atrial Fibrillation, Aged