Contraceptive Planning For Women With and Without Cardiovascular Disease
Quick Takes
- Women of reproductive age with cardiovascular disease (CVD) require preconception planning with a multidisciplinary team to assess pregnancy risks and contraceptive options.
- Long-acting reversible contraception (LARC), such as intrauterine devices and subdermal implants, are the most efficacious and have the largest safety profile for women with CVD.
- For women with severe CVD or modified World Health Organization risk class IV, pregnancy is not recommended and LARC should be encouraged.
- Social determinants of health negatively affect outcomes in women with CVD.
This article highlights the critical role of preconception counseling and effective contraceptive planning for women of reproductive age with cardiovascular disease (CVD). These women face unique challenges, including the potential for teratogenic medication use and heightened risks of morbidity and mortality during pregnancy.
Preconception Counseling and Risk Assessment
For women with CVD, pregnancy planning is crucial. Preconception counseling allows for risk stratification, medication adjustment, and comprehensive patient education. Women with CVD often take medications that pose teratogenic risks, making early and individualized counseling essential to mitigate potential harm. Despite the importance of these discussions, studies show that only about half of women with congenital heart disease recall receiving contraception counseling.1-3 This alarming gap underscores the need for proactive engagement by cardiology teams, beginning in adolescence and continuing into adulthood. Pediatric and adult cardiologists must collaborate to ensure continuity of care and reproductive health discussions.4,5
Preconception counseling should involve a multidisciplinary team to address both cardiovascular and obstetric concerns. Detailed risk assessments, identifying modifiable risks, optimizing medical therapy, and establishing a pregnancy management plan tailored to the patient's specific condition are essential components of this approach. In addition, integrating patient education about potential complications and risks to both the mother and fetus ensures informed decision-making and better outcomes for both mother and child.6
Contraceptive Methods
Contraceptive options should prioritize safety and effectiveness, particularly in high-risk groups. Tier I contraception is comprised of long-acting reversible contraceptives (LARCs), such as intrauterine devices (IUDs) and subdermal implants, and have a typical-use 1-year failure rate of <1%, which makes them highly efficacious. They also have greater safety profiles than Tier II and Tier III methods.6 Hormonal IUDs, in particular, offer added benefits for women on anticoagulants by reducing heavy menstrual bleeding, a common concern in this population. These methods provide reliable contraception without significantly increasing cardiovascular risks, making them the preferred choice for many women with CVD.7
For women at elevated thromboembolic risk, combined hormonal contraceptives (CHCs) are associated with an increased clotting risk. However, CHCs may still be appropriate for select patients under close monitoring. Progestin-only methods, such as progestin-only pills or injectables (9% vs. 6% effective),8 offer alternative options for patients who cannot use estrogen-containing methods. Effective contraceptive counseling should involve shared decision-making, in which the patient's preferences and lifestyle are carefully considered alongside clinical recommendations.8,9
Emergency Contraception
Emergency contraceptives are underutilized in women with CVD, often due to barriers like cost and access. Copper IUDs offer a dual advantage as both emergency contraception and long-term prevention. With a failure rate of <0.1%, copper IUDs are the most effective form of emergency contraception. However, their use is limited by the need for an in-office procedure, which may not be immediately available to all patients. Logistical and financial challenges disproportionately impact low-income and rural women, further highlighting the need for equitable health care access.10
Oral emergency contraceptives, such as levonorgestrel and ulipristal acetate, are valuable alternatives but must be taken within 5 days of unprotected intercourse. Their failure rates can vary from 1% to 3%.11 Although widely available, their effectiveness diminishes with time, body mass index, and potential drug-drug interactions, necessitating timely access and proper counseling. Pretreatment with antiemetics may be recommended to mitigate adverse effects such as nausea and vomiting, enhancing patient comfort and compliance. Advanced provision of emergency contraception is safe in women with CVD and can improve usage rates and reduce the incidence of unplanned pregnancies, particularly in high-risk populations.
Pregnancy Termination
For women with severe CVD or modified World Health Organization (WHO) risk class IV conditions, pregnancy termination should be discussed to reduce the risk of morbidity and mortality. The risks of continuing pregnancy in these cases often outweigh the potential benefits, necessitating open and compassionate conversations between patients and their care teams. Surgical methods of termination are generally preferred for women with significant cardiovascular risks, such as pulmonary hypertension or cardiomyopathy, as they allow for a controlled environment and reduce the physiological stress associated with medical termination and are also better tolerated than pregnancy and delivery.3
Timely decision-making is critical to minimize complications, as the risks associated with abortion increase with gestational age. Multidisciplinary collaboration is essential to address anticoagulation management, balancing the risks of bleeding with thromboembolic events. Clinicians must provide empathetic support and evidence-based guidance to help patients navigate these complex decisions.12
Addressing Disparities
Disparities in access to contraception and reproductive care disproportionately affect women with high CVD burdens, particularly those in low-income, rural, or minority populations. Women from underserved communities often face barriers such as cost, lack of insurance, limited access to health care providers, and geographic challenges. These factors exacerbate the risks of unplanned pregnancies in women who are already at high risk for pregnancy-related complications.4
Addressing these disparities requires systemic efforts, including policy changes to improve coverage for contraceptive services, expansion of community health programs, and enhanced provider education. Additionally, ensuring the availability of youth-friendly and culturally sensitive health care services can help bridge gaps in care. Health care systems must prioritize equitable access to reproductive care to improve outcomes for women with CVD and to reduce health care disparities.13
Multidisciplinary Care and Shared Decision-Making
A cardio-obstetrics team-based approach is essential for optimal outcomes. This model integrates expertise from cardiologists, obstetricians, primary care providers, and other specialists to deliver comprehensive, patient-centered care. Regular assessments of reproductive goals and contraceptive needs should be a routine part of cardiovascular care for women of reproductive age. Shared decision-making is a cornerstone of this approach, ensuring that patients are actively involved in their care plans.
Clinicians should provide clear and evidence-based information about the risks and benefits of various contraceptive options, empowering patients to make informed choices that align with their values and health goals. By fostering open communication and collaboration, multidisciplinary teams can address the complex needs of women with CVD and improve overall care quality (Figure 1).13
Figure 1: Multidisciplinary model for shared decision-making in contraception and pregnancy counseling for women with cardiovascular conditions
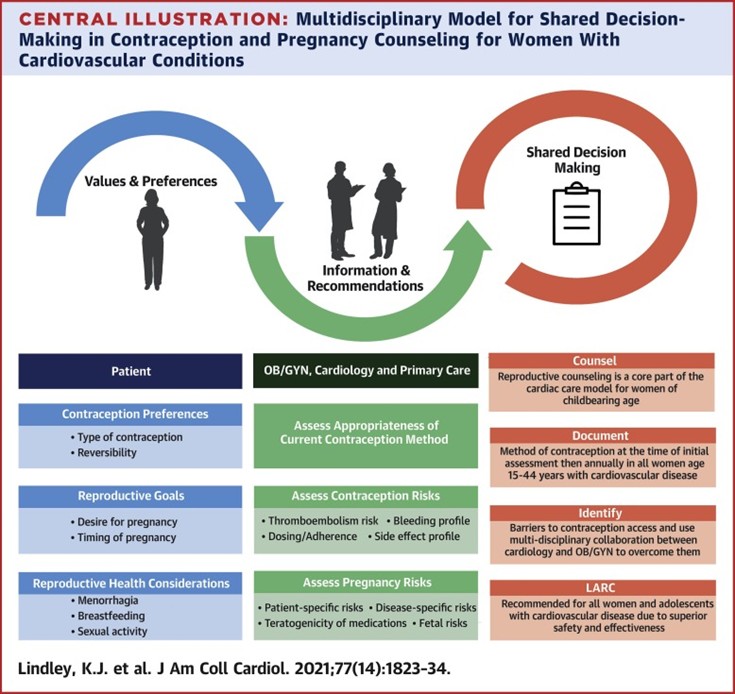
Reproduced with permission from Lindley KJ, Teal SB. Contraception in women with cardiovascular disease. JAMA. 2022;328(6):577-578. doi:10.1001/jama.2022.11541.
LARC = long-acting reversible contraception; OB/GYN = obstetrician/gynecologist.
Expert Recommendations
- Expand education: Both pediatric and adult cardiologists must be equipped to discuss contraceptive safety and pregnancy risks with women of reproductive age. Ongoing training and resources are critical to ensure providers can address these topics effectively.
- Start with 8s: Increase education and access to 8s, particularly for high-risk patients. These methods should be emphasized as first-line options for most women with CVD.
- Advance research: Further studies are needed to guide evidence-based recommendations, especially in complex cases of CVD during pregnancy. Research should focus on optimizing care for medically complex patients.
- Address barriers: Improve access to reproductive health care for underserved populations through policy changes and community outreach. Innovative solutions, such as telehealth services, can help bridge gaps in care.
Conclusion
Effective contraception and pregnancy planning are critical components of cardiovascular care for women. A multidisciplinary, patient-centered approach ensures safer reproductive outcomes and improved quality of life for this high-risk population.
References
- Lu CW, Wu MH, Wang JK, et al. Preconception counseling for women with congenital heart disease. Acta Cardiol Sin. 2015;31(6):500-506. doi:10.6515/acs20150319b
- Farr SL, Downing KF, Tepper NK, Oster ME, Glidewell MJ, Reefhuis J. Reproductive health of women with congenital heart defects. J Womens Health (Larchmt). 2023;32(2):132-137. doi:10.1089/jwh.2022.0513
- European Society of Gynecology (ESG); Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), et al. ESC guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2011;32(24):3147-3197. doi:10.1093/eurheartj/ehr218
- Lindley KJ, Teal SB. Contraception in women with cardiovascular disease. JAMA. 2022;328(6):577-578. doi:10.1001/jama.2022.11541
- Wang T, Chen L, Yang T, et al. Congenital heart disease and risk of cardiovascular disease: a meta-analysis of cohort studies. J Am Heart Assoc. 2019;8(10):e012030. doi:10.1161/JAHA.119.012030
- Lindley KJ, Bairey Merz CN, Davis MB, et al. Contraception and reproductive planning for women with cardiovascular disease: JACC focus seminar 5/5. J Am Coll Cardiol. 2021;77(14):1823-1834. doi:10.1016/j.jacc.2021.02.025
- Roos-Hesselink J, Baris L, Johnson M, et al. Pregnancy outcomes in women with cardiovascular disease: evolving trends over 10 years in the ESC Registry Of Pregnancy And Cardiac disease (ROPAC). Eur Heart J. 2019;40(47):3848-3855. doi:10.1093/eurheartj/ehz136
- Fast facts: effectiveness of birth control methods (ACOG website). 2025. Available at: https://www.acog.org/womens-health/infographics/effectiveness-of-birth-control-methods. Accessed March 27th 2025.
- Mcilvaine S, Feinberg L, Spiel M. Cardiovascular disease in pregnancy. Neoreviews. 2021;22(11):e747-e759. doi:10.1542/neo.22-11-e747
- Salcedo J, Cleland K, Bartz D, Thompson I. Society of family planning clinical recommendation: emergency contraception. Contraception. 2023;121:109958. doi:10.1016/j.contraception.2023.109958
- Cleland K, Raymond EG, Westley E, Trussell J. Emergency contraception review: evidence-based recommendations for clinicians. Clin Obstet Gynecol. 2014;57(4):741-750. doi:10.1097/GRF.0000000000000056
- Samuelson Bannow B, Federspiel JJ, Abel DE, Mauney L, Rosovsky RP, Bates SM. Multidisciplinary care of the pregnant patient with or at risk for venous thromboembolism: a recommended toolkit from the Foundation for Women and Girls with Blood Disorders Thrombosis Subcommittee. J Thromb Haemost. 2023;21(6):1432-1440. doi:10.1016/j.jtha.2023.03.015
- Goldfarb MJ, Saylor MA, Bozkurt B, et al. Patient-centered adult cardiovascular care: a scientific statement from the American Heart Association. Circulation. 2024;149(20):e1176-e1188. doi:10.1161/CIR.0000000000001233
Clinical Topics: Cardiovascular Care Team, Prevention
Keywords: Cardio-Obstetrics, Contraception, Preconception Care, Pregnancy, High-Risk