Management of Recurrent Coarctation in Children
Quick Takes
- Management of recoarctation in children is often dictated by age and anatomical complexity.
- Therapeutic interventions include balloon angioplasty, transcatheter stent implantation, and less commonly, surgical revision.
Coarctation of the aorta accounts for 5-8% of all congenital heart disease, with an incidence of approximately four cases per 10,000 live births.1 It can be seen in isolation or associated with other cardiac lesions. Coarctation can present at any age; however, neonates with ductal dependent or "critical coarctation" can present with heart failure and shock following closure of the ductus arteriosus. The primary treatment for infants with coarctation is surgical repair. The incidence of recurrent coarctation is anywhere from 2% to 31%,2 but in the present era in which extended end-to-end anastomosis is more commonly performed, the rate of restenosis has improved.3
The literature regarding risk factors for recoarctation is conflicting. Previous studies have suggested that the type of surgical repair had an impact on rates of recoarctation; however, a recent systematic review found that the chosen surgical technique is not a strong risk factor.4 Rather, having a smaller aortic arch was a strong predictor of recurrent coarctation, and younger age and lower weight at the time of surgical repair were weak determinants of need for reintervention.
Patients must be followed by a cardiologist throughout their lifetime. It is recommended that they be seen every 1-2 years with upper and lower limb blood pressure checks and echocardiography. Cross-sectional imaging is also recommended every 3-5 years after adolescence, or sooner based on anatomy and symptoms, to assess for recurrent stenosis or aortic aneurysm.5-7 The optimal method for addressing recurrent coarctation in children is not well defined. Indications for intervention in recurrent coarctation in the pediatric population include peak-to-peak gradient >20 mm Hg or lesser gradients when there is significant anatomical evidence of narrowing on imaging with extensive collateral flow or significant ventricular dysfunction.8 Repeat surgery can be performed successfully, although transcatheter balloon angioplasty with and without stent placement has been recommended as first-line treatment in isolated recurrent obstruction.2,8,9 However, the level of evidence supporting these recommendations is somewhat limited.
Balloon angioplasty is often considered in young children. This is frequently preferred over stenting due to lack of small stents that are expandable to adult size in the future. Angioplasty is considered safe and effective with low rates of acute aortic wall injury.8 Longer-term risk of aneurysm is thought to be lower than in native coarctation due to scar tissue at the site of recoarctation. Reintervention rates in short- to medium-term follow-up studies range from 15% to 50%.8,9 Studies looking at the effectiveness of balloon angioplasty when separating different morphologies of recurrent stenosis have suggested that balloon angioplasty should be reserved for discrete (or short localized) narrowing. Angioplasty alone is markedly less effective in long-segment hypoplasia or complex morphology, and these patients may benefit from repeat surgical intervention.2
Transcatheter stent implantation is a reasonable therapy for older children who are large enough to receive a stent that can be expanded to adult size. Stenting can provide structural support to the vessel wall and apposition of torn vessel intima to the media. It carries a lower risk of aortic wall injury or aneurysm compared with balloon angioplasty, as there is no need for oversizing. Bare metal stents are typically used, but covered stents are also an option and often used where an aneurysm is present or for those who develop complications, such as aortic wall perforation or tear.10 Stenting has been shown to be effective at relieving residual gradients with a low rate of recurrent stenosis and unplanned repeat interventions. Reported complication rates are typically lower than seen with angioplasty alone or surgery.9-10
Management of recurrent coarctation in children is often dictated by age and anatomical complexity of the lesion. In the younger child with discrete recurrent coarctation, it is reasonable to consider initial balloon angioplasty. Patients with recoarctation in the setting of aortic arch hypoplasia often require surgical intervention to relieve the areas of stenosis. For the older child and adolescent, stent placement that can be dilated to adult size is often employed. Any patient with coarctation of the aorta requires lifelong monitoring for sequelae, including recurrent coarctation, hypertension, or aneurysm formation. Continued long-term data assessment is needed to determine the interventions that will yield the best outcomes (Figure 1).
Figure 1: Interventional Algorithm for Recurrent Coarctation of the Aorta
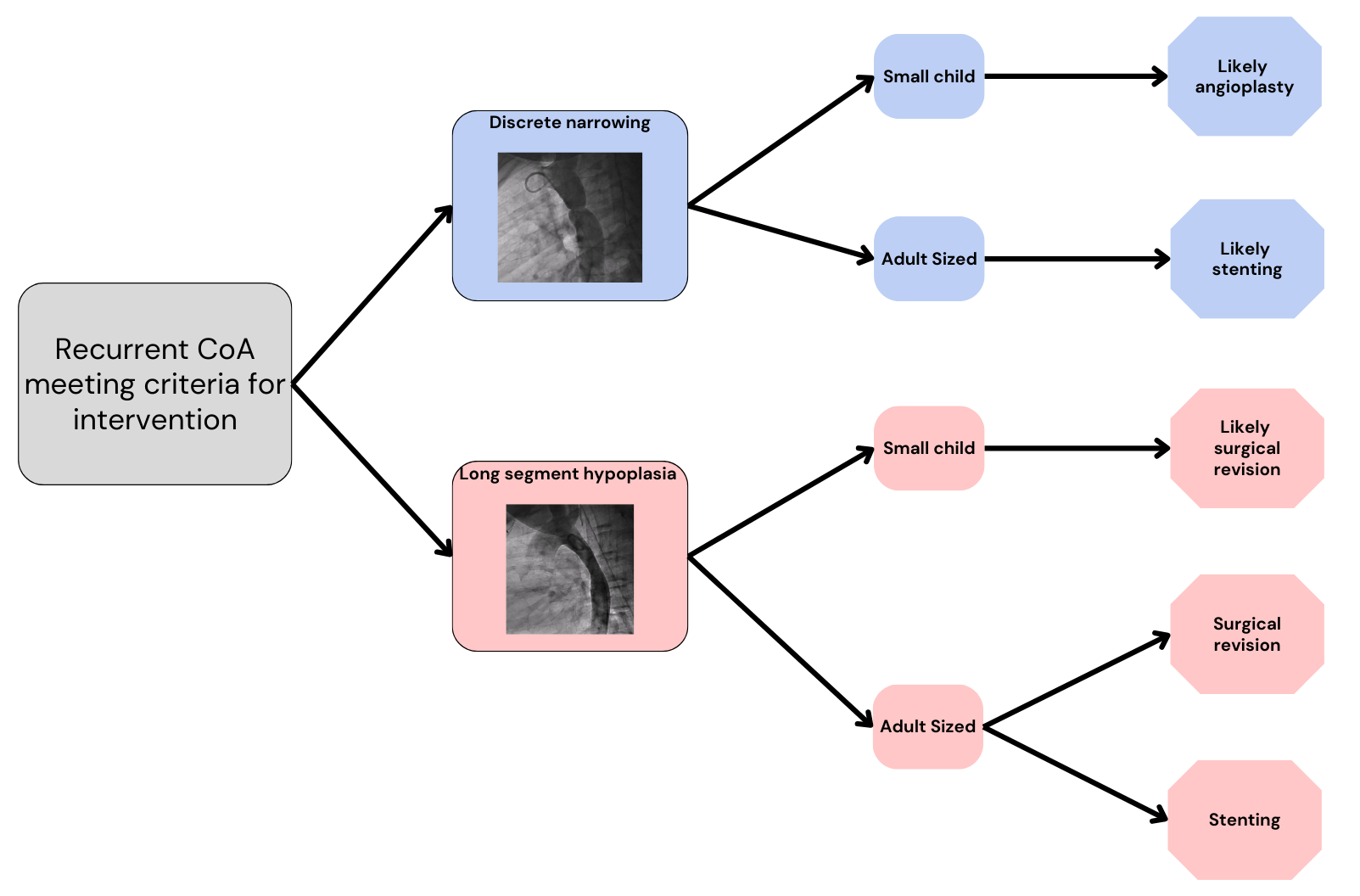
CoA = coarctation of the aorta.
References
- Raza S, Aggarwal S, Jenkins P, et al. Coarctation of the aorta: diagnosis and management. diagnostics (Basel). 2023;13(13):2189. Published 2023 Jun 27. doi:10.3390/diagnostics13132189
- Jiang Q, Hu R, Dong W, et al. Outcomes of arch reintervention for recurrent coarctation in young children. Thorac Cardiovasc Surg. 2022;70(1):26-32. doi:10.1055/s-0041-1731825
- Al-Dairy A. Long-term outcomes of surgical repair of isolated coarctation of the aorta in different age groups. BMC Surg. 2023;23(1):120. Published 2023 May 11. doi:10.1186/s12893-023-02031-5
- Dias MQ, Barros A, Leite-Moreira A, Miranda JO. Risk factors for recoarctation and mortality in infants submitted to aortic coarctation repair: a systematic review. Pediatr Cardiol. 2020;41(3):561-575. doi:10.1007/s00246-020-02319-w
- Salciccioli KB, Zachariah JP. Coarctation of the aorta: modern paradigms across the lifespan. Hypertension. 2023;80(10):1970-1979. doi:10.1161/HYPERTENSIONAHA.123.19454
- Makhoul M, Markush, D, Baker-Smith CM, et al. Clinical practice algorithm for the follow-up of repaired coarctation of the aorta. ACC Expert Analysis. Feb16, 2023. Available at: https://www.acc.org/Latest-in-Cardiology/Articles/2023/02/16/17/09/Clinical-Practice-Algorithm-For-the-Follow-Up-of-Repaired-Coarctation-of-the-Aorta. Accessed 05/23/25.
- Sachdeva R, Valente AM, Armstrong AK, et al. ACC/AHA/ASE/HRS/ISACHD/SCAI/SCCT/SCMR/SOPE 2020 Appropriate use criteria for multimodality imaging during the follow-up care of patients with congenital heart disease: a report of the American College of Cardiology Solution Set Oversight Committee and Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. J Am Coll Cardiol. 2020;75(6):657-703. doi:10.1016/j.jacc.2019.10.002
- Cheng W, Li Z, Ye Z, et al. Stent implantation and balloon angioplasty for native and recurrent coarctation of the aorta. Int Heart J. 2023;64(1):10-21. doi:10.1536/ihj.21-643
- Vasile CM, Laforest G, Bulescu C, Jalal Z, Thambo JB, Iriart X. From Crafoord's end-to-end anastomosis approach to percutaneous interventions: coarctation of the aorta management strategies and reinterventions. J Clin Med. 2023;12(23):7350. Published 2023 Nov 27. doi:10.3390/jcm12237350
- Holzer RJ, Gauvreau K, McEnaney K, Watanabe H, Ringel R. Long-term outcomes of the coarctation of the aorta stent trials. Circ Cardiovasc Interv. 2021;14(6):e010308. doi:10.1161/CIRCINTERVENTIONS.120.010308
Clinical Topics: Congenital Heart Disease and Pediatric Cardiology, Congenital Heart Disease, Cardiac Surgery, Invasive Cardiovascular Angiography and Intervention
Keywords: Aortic Coarctation, Pediatrics, Pediatric Cardiology, Heart Defects, Congenital