Multi-Specialty Approach to PVD

We have had a great success with educating our colleagues of myocardial infarction and stroke, but we tend to forget about peripheral arterial disease.
We know all about heart attacks and brain attacks. Now, it is time to recognize "leg attacks."
Until I became a cardiovascular fellow, I did not realize cardiology's involvement with peripheral vascular disease (PVD). PVD affects more than 18 million people in the U.S., and almost half of them are asymptomatic.
Since only about 20 percent of patients with PVD have typical symptoms, it is commonly under diagnosed. As an internal medicine resident, I rarely had a PVD in my differential. Specialists traditionally get consulted for PVD once it is evident on physical exam.
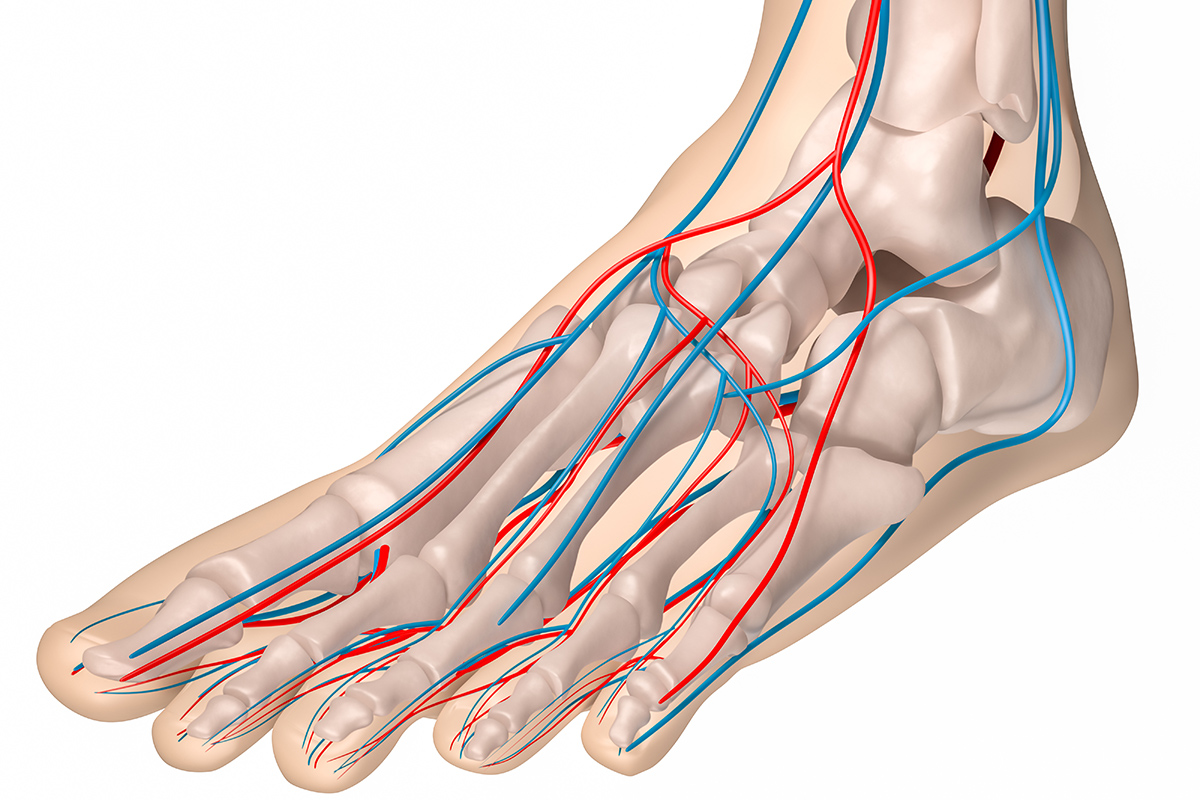
One of the most feared complications of peripheral arterial disease (PAD) is critical limb ischemia. Most of these patients suffer from diabetes and end-stage renal disease, and are being managed by primary care physicians, cardiologists, endocrinologists, surgeons and nephrologists.

The PARTNERS trial was a cross sectional study which looked at 350 primary care practices all over the U.S. The study found that 49 percent of primary care physicians (PCP) failed to recognize patient's previous PAD history.
Small studies have found that median time to referral after a foot ulcer is about 19 days and 25 percent of those foot ulcers are managed by PCP for three months before a specialist referral.
Cardiologist are no different, primarily due to lack of physician awareness of PAD, underestimation of foot infection and lack of recognition of ischemia due to PAD. Hence, there are high rates of amputation or irreversible damage in this patient population.
A multispecialty approach to PAD is the key. There are patients sitting in your waiting rooms with PAD risk factors such as smoking, diabetes, hypertension, obesity and hypercholesterolemia. These are our daily "bread and butter" patients.
Physicians need to expand our differential and look beyond the heart and brain. The utility of recent PAD screening with creation of algorithms remains uncertain.
An optimal approach to the diagnosis and treatment of PAD requires a multidisciplinary team with proper training of the initial staff members. A multidisciplinary team can include a PCP, cardiologist, interventional cardiologist, vascular surgeon, endocrinologist, podiatry, wound care team and other experts.
Screening should be offered to anyone over the age 50 with PAD risk factors for early recognition of disease process. Appropriate referral and early recognition of the condition will encourage effective management with the greatest chance of quality of life, and prevention of unnecessary amputation.
Patients should be thoroughly evaluated by the multi-specialty team before any amputation. Just like you care about vessels to your heart and brain, let us not forget they go to your extremities as well.
