Highlights From the TCT 2020 Virtual Conference

Like many conferences during the COVID-19 pandemic, the recent Transcatheter Cardiovascular Therapeutics (TCT) Virtual Conference was like no other. The virtual format has resulted in a larger audience and provided more flexibility, especially for the busy Fellows in Training. In this piece, I wanted to share some of the highlights from the TCT Virtual Conference.
Percutaneous Coronary Interventions (PCI)
The conference had several important studies presented on PCI covering a range of topics, including stent optimization strategies and complex lesion management. Starting with the use of fractional flow reserve (FFR), the TARGET FFR trial, presented by Damien Collison, MD, evaluated an important question: does a physiology-guided incremental optimization strategy (PIOS) – using FFR to guide post-PCI stent optimization – improve outcomes? In a randomized trial of 260 patients undergoing PCI, PIOS failed to show a significant improvement in the primary outcome; post-PCI FFR > 0.9. However, questions still remain about its impact on other outcomes.
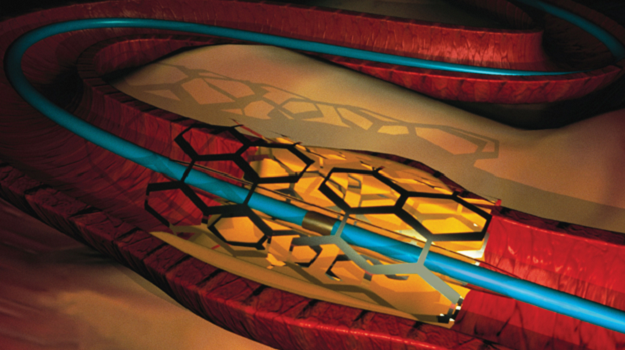
Other methods of PCI optimization were also presented. In the ULTIMATE trial, presented by Xiao-Fei Gao, MD, intravascular ultrasound (IVUS) guidance was evaluated in 1,448 patients undergoing PCI with drug-eluting stent. After three years of follow up, IVUS guidance was associated with lower rates of the primary outcome; target vessel failure (6.6% in IVUS guidance versus 10.7% angiography guidance; p value = 0.01) and lower rates of the safety outcome; stent thrombosis (0.1% in IVUS guidance group versus 1.1% angiography guidance group; P value = 0.02).
Finally, the Disrupt CAD III study, presented by Jonathan M. Hill, MD, evaluated the use of coronary intravascular lithotripsy (IVL) in an international multicenter study of 431 patients undergoing PCI with severely calcified lesions. The study showed that 92.4% of patients achieved the primary efficacy endpoint of procedural success and there were no major safety concerns. However, longer follow up is needed to truly understand the impact of this new application of IVL on such lesions. This is unlikely to replace currently used atheroablative devices but may serve as an additional option in certain cases.
Peripheral Interventions
The conference also had several studies on peripheral interventions with several addressing the controversies surrounding paclitaxel drug-coated balloon (DCB). The IN.PACT BTK trial, presented by Antonio Micari, MD, evaluated the effectiveness and safety of the IN.PACT 014 paclitaxel DCB; a different DCB from the one recently removed from the market by the FDA (IN.PACT Admiral). In a randomized trial of 50 patients with critical limb ischemia and chronic total occlusions in the infra-popliteal arteries. There was no significant difference in the primary safety outcome at 30 days. In addition, at nine months follow up, there was a nonsignificant difference in the primary effectiveness outcome; late lumen loss (0.89 +/- 77 mm in DCB versus 1.31 +/- 0.72 mm in PTA; P value = 0.017). Similar findings were presented from the VOYAGER PAD trial. It is difficult to make any conclusions from these findings and larger studies are certainly needed to address this important issue.
Structural Heart Disease Interventions
In the field of structural heart disease intervention, there were several important TAVR studies presented. Two studies were presented on the outcomes of valve-in-valve TAVR in different populations.
The TRANSIT study evaluated the outcomes of having a second TAVR in 172 low-risk patients with degenerated bioprosthetic valve. The authors noted an all-cause mortality of 7% at 30 days and 10% at one year follow up; about 58% of which were cardiovascular related.
On a similar topic, the PARTNER 2 trial valve-in-valve (VIV) sub-study, presented by Rebecca T. Hahn, MD, FACC, showed no significant difference in all-cause mortality between ViV patients (high risk) and intermediate risk patients undergoing first TAVR at five years (50.6% in ViV group vs. 45.9% in native TAVR group; P value = 0.06). In addition, these patients had significant improvement in functional status and quality of life with similar rates of valve degeneration to native SAPIEN XT valves at five years of follow-up. These findings highlight the growing evidence on the use of VIV TAVR in different populations.
Several studies were also presented on cerebral embolic protection (CEP) during TAVR. The REFLECT II trial evaluated the role of CEP using the TriGUARD 3 device in a randomized trial that was suspended prematurely by the sponsor. The study did not show a significant difference in the primary outcome of all-cause mortality or stroke. Interestingly, findings from the STS-ACC TVT registry, were also presented showing that EPD was used in 10% of patients but with marked variations in use between hospitals and no significant difference in the primary safety and efficacy outcomes. Overall, these findings are an important step in better understanding the use and outcomes of CEP.
The TCT 2020 virtual conference provided attendees with great new insights on so many topics. It was both educational and inspiring to learn from the experts in the field. I learned a lot from the presentations, and it has certainly had an influence on my clinical and research focus.


