The Road to Technology Development, Interview with the Director of Stanford Biodesign, Dr. Josh Makower
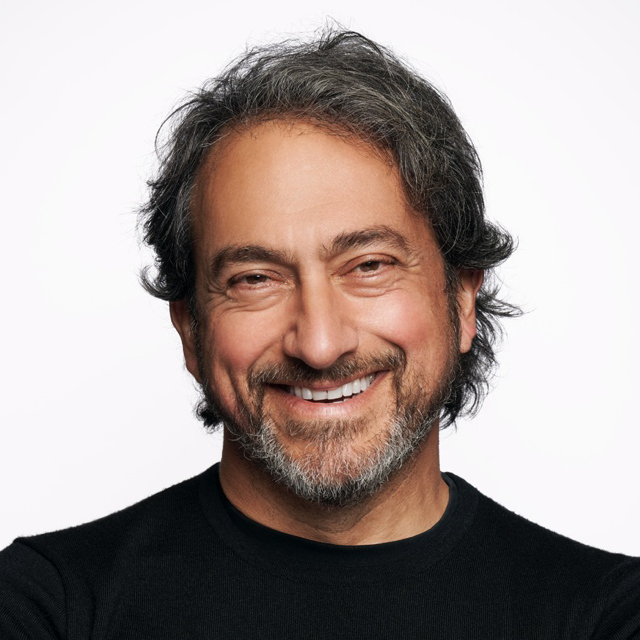
Josh Makower, MD, is a professor of medicine and bioengineering at the Stanford University Schools of Medicine and Engineering. He also serves as director of Stanford Byers Center for Biodesign. Makower received a bachelor's degree in Mechanical Engineering from Massachusetts Institute of Technology, a medical degree from New York University School of Medicine, and an MBA from Columbia University. As an entrepreneur, Josh holds over 300 patents and patent applications, has founded nine startups, and was awarded the Coulter Award for Healthcare Innovation by the Biomedical Engineering Society in 2018.
How did Stanford Biodesign come to be, and how has the program evolved over the last two decades?
Almost 30 years ago while working at Pfizer, Inc. in New York City, I had the unique opportunity to study the process of how successful medical device startups solved problems and was able to contrast that with similar teams inside of large companies. I observed that successful startups prioritized clinical needs, whereas teams inside big companies started with a technology and looked for places to apply it. The results were starkly different. I believed that if we could break down the steps successful teams used into reproducible steps, innovation could happen anywhere – even within big companies. The process we proposed was simple: Focus on the needs first, convert those statements into a detailed specification, and then use that to brainstorm new solutions. I began developing this method myself first within Pfizer and then through multiple startups at my incubator, called ExploraMed. Almost 10 years later, I had the great fortune to meet Paul Yock, MD, FACC. Yock was looking to build a focused effort inside of Stanford to help students prepare for medical device careers, and so the idea to translate this method into a teaching platform was hatched.
Over the last 20 years, Yock has led the program with great success, expanding the size of the fellowship and internal team, building out the graduate curriculum across an array of topics including digital health and value-based innovation, and building an international presence. It's amazing to look back and see what has been accomplished under his leadership; almost 4.5 million patients have benefitted from the inventions of our students and fellows, and thousands of students inoculated with Biodesign-thinking are now spread across the world.
Why do you think we need clinicians who are trained in technology development?
It is important for innovative clinicians to learn the process behind technology development as it will help them understand the role they can play, as well as the roles ideally played by others, and ultimately enable them to have a higher probability of success. One of the most important key learnings from the process is the discipline of need finding and need statement/specification creation. It sounds easy, but it really isn't! Often, clinicians embed solutions as they try to frame needs, and that distorts the next steps and limits the breadth of the solutions proposed. Also, it is common for an inventor to "fall in love" with their initial ideas, and this limits their ability to impartially judge how well they match the need criteria. By mastering these, and the many other elements of the process, one can more accurately address the real need, and thereby be more likely to succeed with their innovation.
What are the major obstacles faced by clinicians with technology ideas and how can they overcome them?
It takes amazing perseverance to accomplish anything of value. Interestingly, it's usually reimbursement that stands as the biggest barrier to innovation. Even after approval by the FDA, it's very hard to establish a new therapy with a new code, coverage and payment. One must be prepared for these challenges and think ahead to design studies and deliver enough evidence to convince payers that the therapy is worthy.
The next most challenging process is usually achieving regulatory approvals. While the FDA has made great strides over the past several years in attempts to improve transparency and predictability, there remains a wide variation of approaches from reviewer to reviewer. This can lead to unexpected delays and challenges, which can be very expensive for innovators to navigate.
What is your advice to academic institutions that aim at leveraging innovation and technology transfer?
I would recommend applying the same filter of what is truly needed to the technologies before trying to transfer things out. Not every idea or technology will address the needs best. If the faculty have a keen sense of the Biodesign process and practice it as they innovate, they should be able to meet the mark more often than not. All these steps also will help colleagues in the technology licensing department of the University understand where the innovation fits, how significant its potential is, and who might be the right partners to approach.
