Harold on History | The Evolution of Personalized Medicine
Personalized medicine, also called precision or individualized medicine, is the tailoring of interventions for prevention and treatment of disease to the individual characteristics of each patient. The complete sequencing of the human genome, completed in 2003, facilitated further evolution of personalized medicine, moving beyond the genome into the entire spectrum of molecular medicine.
The Human Genome Project has facilitated whole genome interrogation, obtaining panomics data from individual patients that can identify genomic and metabolomic phenotypes to develop more efficient treatment strategies. This has led to a greater understanding of how a person's unique molecular and genetic profile makes them susceptible to certain diseases through the interactions (interactome) of the DNA sequence, transcriptome, proteome, metabolome, microbiome and epigenome.
By moving from a "one size fits all approach" to one of personalized medicine, we've also moved from being reactive to being proactive, whereby we can focus on prevention and the optimal selection of drug therapy that best addresses a patient's unique medical attributes. The upside? Better treatment and less trial and error in prescribing medicine.
Deep phenotyping with data analysis performed using network analysis can further optimize medication and behavioral changes to improve health – for each patient. Rather than mass population screening, genomic and proteomic biomarkers can reveal the underlying cause of a disease for direct targeting.
Steve Jobs crystalized this convergence, saying, "I think the biggest innovations of the 21st century will be at the intersection of biology and technology. A new era is beginning."
In a sense, personalized medicine is not entirely new. The identification of the ABO blood group system, in 1901 by Karl Landsteiner at the University of Vienna, may be one of the first instances of recognizing differences in each patient's biology. Landsteiner's discovery of why some blood transfusions were successful and others were not led to him winning the Nobel Prize in physiology and medicine in 1930.
The first published account of a case of recessive inheritance in humans was in 1902. Sir Archibald Garrod, an Oxford trained physician, made the first connection between genetic inheritance and Mendel's laws of inheritance and susceptibility to a disease called alkaptonuria. He proposed the idea that diseases occur through a metabolic route, leading to the molecular basis of inheritance.
The discovery of DNA, in 1869 by the Swiss chemist Friedrich Miescher, based on analysis of pus-coated surgical bandages, set the stage for future studies in molecular medicine.
From there, the way RNA and DNA molecules are put together was discovered by Russian biochemist Phoebus Levene in 1919; DNA structure was further defined in 1950 by Austro-Hungarian biochemist Erwin Chargaff, facilitating the discovery of DNA's double helix structure in 1953 by James D. Watson and Francis H. C. Crick; all leading to the first DNA sequencing method in 1977, developed by Frederick Sanger.
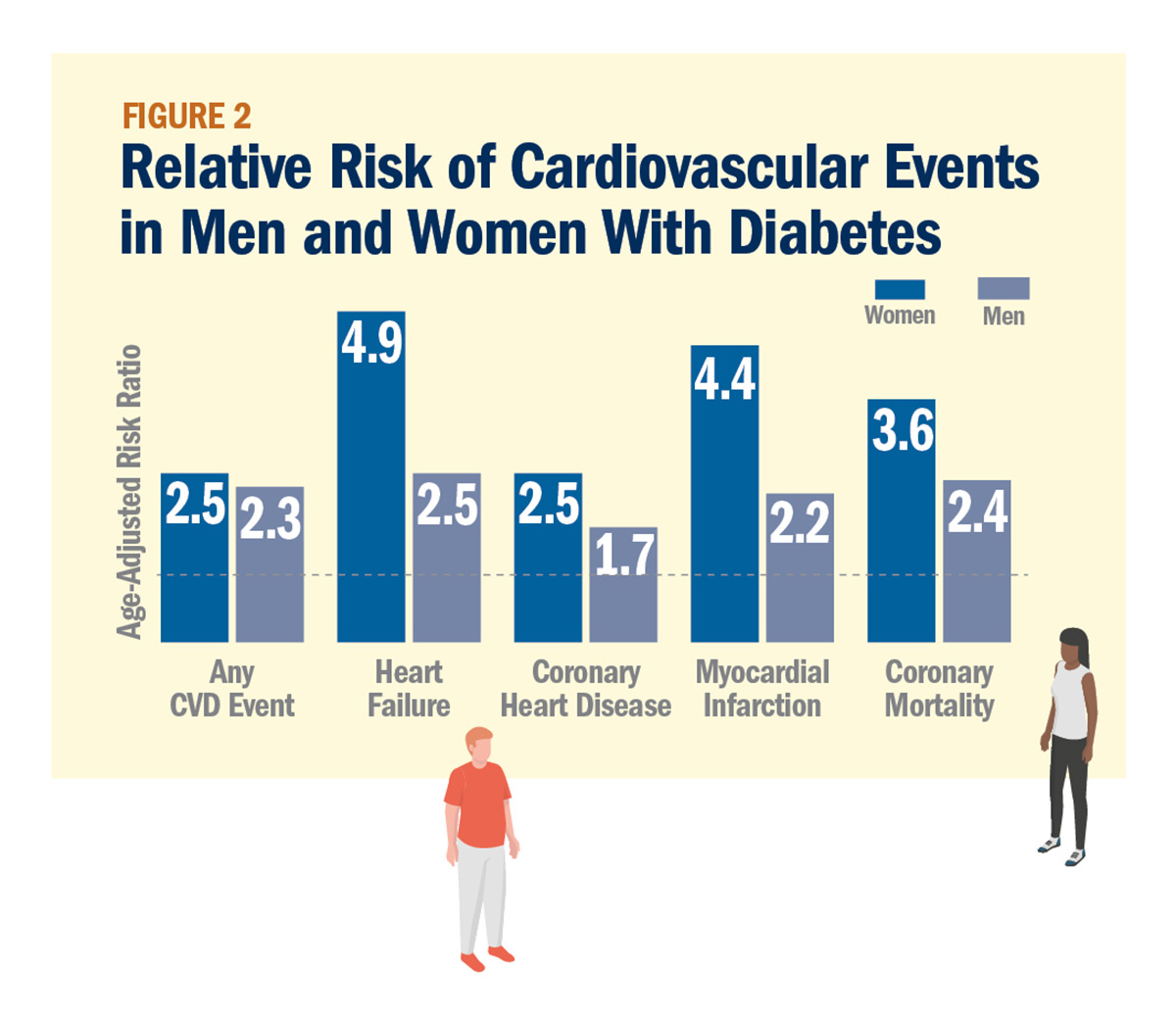
Today, health and disease can be defined by genetic fingerprints, enabled by the availability of the entire complement of the human genome. We've come to realize that diseases such as diabetes, cancer and heart disease are caused by a complex interplay of genetic and environmental factors.
Understanding family history and inherited components of diseases may allow more focused predictions of an individual's health risks, facilitating greater patient involvement in generating their own personal data and using it to guide their own medical management.
The association of genetic risk with disease outcomes can be as strong as lifestyle risk. Cardiovascular precision medicine can integrate basic science techniques with genomic information and may allow for correcting disease-associated genetic mutations using new cutting-edge technologies, like CRISPR systems, in disease-driven cardiomyopathy.
Pharmacogenomics is leading to the development of effective drug therapies in cardiovascular therapeutics for smaller subgroups of patients stratified by their genetic profile. Chemical and biological probes used in molecular imaging can identify molecular pathway mechanisms and help guide clinical decision-making. Clopidogrel therapy can have a different impact on reducing stent thrombosis depending on patients' genetic variance within CYP2C19, which encodes an enzyme that covers the drug from an inactive to active state. PCSK9 inhibitors for the management of hyperlipidemia are an example of targeted cardiovascular therapeutics driven by genomics.
Sensor technology such as wearables will allow us to understand the physiome, which describes the physiological dynamics of the normal intact organism, and is built upon information and structure. Neural networks and artificial intelligence will play an increasingly important role in understanding the physiome using big data and gaming theory. The impact of consumer genomics and genetic risk scoring continues to evolve.
On Dec. 18, 2015, President Barack Obama signed the bipartisan Precision Medicine Initiative. He defined the effort as "delivering the right treatments, at the right time, every time to the right person." The National Institutes of Health (NIH) is driving participant-engaged, data-driven research efforts at the intersection of human biology, behavior, genetics, environment, data science and computation aimed at developing more effective ways to improve health and treat disease.
Using knowledge gained from genome-wide association studies, we can develop a greater understanding of disease at the molecular level to predict the risk of developing a disease and present patients with potential treatment and/or preventive strategies. Personalized medicine will increasingly utilize emerging technologies for prevention and treatment, looking at individual variability in genes, environment and lifestyle – marking a new relationship between genomics and drug discovery.

Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, EP Basic Science, Genetic Arrhythmic Conditions, Heart Failure and Cardiac Biomarkers, Interventions and Imaging
Keywords: ACC Publications, Cardiology Magazine, Human Genome Project, Genome, Human, Pharmacogenetics, Proteome, Molecular Medicine, ABO Blood-Group System, Genome-Wide Association Study, Proteomics, Clustered Regularly Interspaced Short Palindromic Repeats, Base Sequence, Metabolome, Transcriptome, RNA, Patient Participation, Nobel Prize, Alkaptonuria, Genomics, Ticlopidine, Sequence Analysis, DNA, Drug Discovery, Mutation, National Institutes of Health (U.S.), Phenotype, DNA, Artificial Intelligence, Neoplasms, Microbiota, Life Style, Molecular Imaging, Blood Transfusion, Hyperlipidemias, Cardiomyopathies, Thrombosis, Diabetes Mellitus, Heart Diseases, Biomarkers, Stents, Suppuration
< Back to Listings