STEMI Management Update 2021: What Have We Learned?
Quick Takes
- The COVID pandemic has had a profound impact on STEMI care.
- This has reaffirmed the ACC/AHA adage that "the appropriate and timely use of some form of reperfusion therapy is likely more important than the choice of therapy" given the undeniable harm of delay in treatment.
- Future advances in addressing myocardial salvage, microvascular obstruction, coronary remodeling, and secondary prevention will enhance STEMI care.
Amidst these remarkable, disruptive times, it seems appropriate that one may reasonably take some latitude in defining the length of a year. The extraordinary evolution in our care of ST-elevation myocardial infarction (STEMI) patients has been dominated by an unprecedented pandemic that has transformed the landscape of STEMI management.1 The emergence of COVID-19 as a global threat overwhelmed emergency medical services (EMS), health care systems and health care providers worldwide: remarkably, this continues to the present day. The subsequent demand for urgent medical attention, coupled with requirements for mechanical ventilation and intensive care unit beds has transformed percutaneous coronary intervention (PCI) capable hospitals into coronavirus centers, thereby attenuating PCI services with redeployment of essential providers to COVID-19 care areas. Suspensions of pre-hospital PCI lab activations to facilitate COVID testing and appropriate triage have delayed EMS response times. Impediments to inter-hospital transfers have resulted in longer total ischemic times. Paradoxically, there has been a dramatic decrease in the number of STEMI presentations related, in part, to patient concerns about exposure to COVID-19. The sometimes-confusing clinical milieu in this environment highlights the need to recognize STEMI mimics to guide appropriate therapy and avoid unnecessary angiography.
The important dual goals of timely reperfusion therapy and the safety of health care providers necessitated modifications in protocols in many PCI hospitals and reasserted the appropriateness of pharmaco-invasive therapy as a legitimate alternative, especially in early presenting patients.1 So too was there recognition of the need for more rapid but safe patient discharge to facilitate use of hospital services while recognizing the necessity to monitor ongoing performance and track metrics and outcomes. Despite the long-standing pre-occupation with door-to-balloon time (DBT), it has been re-emphasized that total ischemic time is paramount as reported in a new pooled analysis of over 3,000 STEMI patients from ten randomized trials undergoing primary PCI (pPCI). When stratified by both ischemic times and DBT, cardiac magnetic resonance imaging (MRI) revealed that infarct size and microvascular obstruction were strongly correlated to ischemic time but not DBT.2 The global occurrence of STEMI and optimizing care in low and middle income countries reaffirms the American College of Cardiology (ACC)/American Heart Association (AHA) guideline adage that "the appropriate and timely use of some form of reperfusion therapy is likely more important than the choice of therapy" given the undeniable harm of delay.3,4 Recent registry data from Canada, France and Mexico support the utility of the pharmaco-invasive approach as compared to pPCI.5-7
The heterogeneity of acute coronary syndrome patients continuously challenges clinicians as to how best to balance the benefit and risks when employing anti-thrombotic therapy. Artificial intelligence and machine learning capabilities from large data sets have utilized high-dimensional, non-linear relationships to make data-driven predictions that integrate the concurrent risk of myocardial infarction and major bleeding thereby informing more strategic decisions to enhancing an optimal margin of benefit.8
Appropriate treatment of the non-culprit disease in STEMI is complex. Coronary flow limitation as well as characterization of the putative plaque are likely to provide more insight into how best to manage these patients. Whereas intervention of major obstructive non-culprit vessels appears beneficial, understanding which non-obstructive coronary vessels in the peri-myocardial infarction period pose an increased risk for future adverse cardiac events remains challenging. Recent Scandinavian data using infrared spectroscopy and intravascular ultrasound indicates that lesions exhibiting both a high lipid content and large plaque burden portend susceptibility to subsequent morbidity and mortality.9
The occurrence of residual microvascular obstruction (MVO), despite restoration of macrovascular flow, constitutes a previously unrealized Achilles' heel of STEMI management that occurs in at least one-third of such patients undergoing coronary reperfusion. Because inflammation is a legitimate casual culprit for failed reperfusion, targeting inhibition of the interleukin-6 receptor with tocilizumab was the focus of a study in three high volume Norwegian PCI centers. Within six hours, 199 STEMI patients underwent pPCI. Patients were randomized to placebo or 280 mg of tocilizumab and the primary endpoint was myocardial salvage index as quantified by MRI. Although no significant difference in infarct size was observed at 6 months, in those patients treated beyond 3 hours (where MVO would be expected to be greatest), salvage index was improved thereby keeping the door open for future investigation of this approach.10
Notwithstanding the lessons emerging from randomized clinical trials and registries, such findings are not necessarily transferable to local jurisdictions. When considering the multiplicity of factors including differing health care systems, provider and institutional expertise, socio-economic conditions, geography, and climate, it is obvious that one mode of reperfusion cannot always fit all patients in all locales. Of most STEMI patients presenting to non-PCI hospitals, half are "walk-ins" and despite great efforts over two decades, at least 50% of these do not receive pPCI within desirable time windows. Monitoring the quality of patient outcomes and adapting to this feedback while preserving a humanistic and holistic approach is a responsibility we all share.
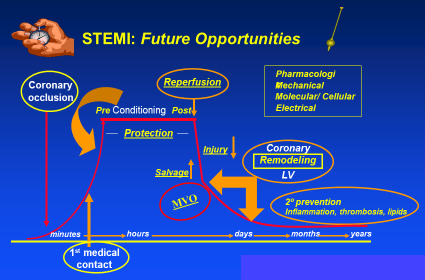
As we look to the future, there are a host of investigative efforts designed to inform optimal care of STEMI patients. These include enhanced diagnosis and treatment in the peri COVID-19 era, deciding on the most appropriate fibrinolytic dosing of pharmaco-invasive therapy, and exploring which innovative pharmacotherapy limits secondary events and favorably modifies coronary and ventricular remodeling. There has been tremendous progress in STEMI care to date. However future opportunities remain relating to timelier reperfusion, lessons learned from periconditioning, myocardial salvage, microvascular obstruction, coronary remodeling, and secondary prevention. These and other opportunities to enhance the future of STEMI care (Figure 1) give us optimism that advances in STEMI for our patients will continue.
Figure 1: Summary of Opportunities to Enhance STEMI Care According to Elapsed Time
References
- Bainey KR, Bates ER, Armstrong PW. ST-segment-elevation myocardial infarction care and COVID-19: the value proposition of fibrinolytic therapy and the pharmacoinvasive strategy. Circ Cardiovasc Qual Outcomes 2020;13:e006834.
- Redfors B, Mohebi R, Giustino G, et al. Time delay, infarct size, and microvascular obstruction after primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv 2021;14:e009879.
- Chandrashekhar Y, Alexander T, Mullasari A, et al. Resource and infrastructure-appropriate management of ST-segment elevation myocardial infarction in low- and middle-income countries. Circulation 2020;141:2004-25.
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78-e140.
- Bainey KR, Armstrong PW, Zheng Y, et al. Pharmacoinvasive strategy versus primary percutaneous coronary intervention in ST-elevation myocardial infarction in clinical practice: insights from the Vital Heart Response Registry. Circ Cardiovasc Interv 2019;12:e008059.
- Danchin N, Popovic B, Puymirat E, et al. Five-year outcomes following timely primary percutaneous intervention, late primary percutaneous intervention, or a pharmaco-invasive strategy in ST-segment elevation myocardial infarction: the FAST-MI programme. Eur Heart J 2020;41:858-66.
- Araiza-Garaygordobil D, Gopar-Nieto R, Cabello-López A, et al. Pharmacoinvasive strategy vs primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction: results from a study in Mexico City. CJC Open 2020;3:409-18.
- D'Ascenzo F, De Filippo O, Gallone G, et al. Machine learning-based prediction of adverse events following an acute coronary syndrome (PRAISE): a modelling study of pooled datasets. Lancet 2021;397:199-207.
- Erlinge D, Maehara A, Ben-Yehuda O, et al. Identification of vulnerable plaques and patients by intracoronary near-infrared spectroscopy and ultrasound (PROSPECT II): a prospective natural history study. Lancet 2021;397:985-95.
- Broch K, Anstensrud AK, Woxholt S, et al. Randomized trial of interleukin-6 receptor inhibition in patients with acute ST-segment elevation myocardial infarction. J Am Coll Cardiol 2021;77:1845-55.
Clinical Topics: Acute Coronary Syndromes, Cardiovascular Care Team, COVID-19 Hub, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Stable Ischemic Heart Disease, Vascular Medicine, Lipid Metabolism, Interventions and ACS, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Nuclear Imaging, Chronic Angina
Keywords: ST Elevation Myocardial Infarction, Myocardial Reperfusion, Percutaneous Coronary Intervention, Coronary Vessels, Ventricular Remodeling, Triage, Acute Coronary Syndrome, Secondary Prevention, Coronavirus, American Heart Association, Patient Discharge, Benchmarking, Respiration, Artificial, Artificial Intelligence, Pandemics, COVID-19, COVID-19 Testing, Receptors, Interleukin-6, Magnetic Resonance Imaging, Hospitals, Registries, Delivery of Health Care, Morbidity, Health Personnel, Inflammation, Intensive Care Units, Angiography, Ultrasonography, Interventional, Spectrum Analysis, Lipids, SARS-CoV-2
< Back to Listings