What to Watch for in the Medical Tents: Non-Cardiac Emergencies and Challenges Faced in Race Medicine
The Collapsed Recreational Runner...
Runner 1: A 38-year-old male marathon runner collapses one mile before crossing the finish line. He is alert but responds with slurred speech and complains of dizziness and nausea. It is a humid day, and the temperature is 28°C (82.4°F). He is tachycardic, tachypneic, and sweating profusely. His core body temperature is 40.5°C (104.9°F).
Runner 2: A 60-year-old woman in the finishers' area of a marathon is found shivering intensely still wearing wet race clothing. It has been raining heavily and the temperature is 4°C (39.2°F). She responds to questions slowly and stumbles as she walks. She is tachycardic, hypertensive, and has a core body temperature of 34°C (93.2°F).
Runner 3: Having just finished his first marathon, a 42-year-old man complains of severe headache and dizziness. He was focused on "drinking a cup of water at each aid station," placed every mile along the course. He later begins to vomit and falls to the ground. His core body temperature is 37.2°C (99°F). A point-of-care sodium reveals a concentration of 123 mmol/L.
Each one of the case examples represent classic descriptions of non-cardiac emergencies encountered in the growing field of race medicine. As we excitedly embrace a return to in-person races, highlighted by the running of the 125th Boston Marathon, we are all aware that endurance running is an extremely popular recreational activity in the United States with over 2.5 million half and full marathon finishers annually.1 While the highest profile endurance races often employ core medical staff, mass numbers of volunteers are still relied upon to provide adequate medical coverage on race day. For smaller races, which represent most recreational road races in the United States (US), volunteer medical coverage represents the entirety of the medical operations. Cardiologists and other medical practitioners volunteering may not be as familiar with the unique array of classic pathologies observed in race medicine and endurance athletes. While life-threatening emergencies are relatively rare,2 physicians supervising endurance races must be able to recognize potentially catastrophic medical events when they present to the medical tents. This expert analysis aims to familiarize readers with race medicine and several key non-cardiac emergencies that occur during recreational endurance races: hyperthermia, hypothermia, and hyponatremia.
Factors Impacting Race Medicine and Epidemiology of Race Emergencies
Unfavorable weather conditions predictably increase the incidence of medical events during recreational endurance events. Wet bulb globe temperature (WBGT) is the gold standard of apparent temperature, which integrates the effects of temperature, humidity, wind, and sunlight in the calculated WBGT. For endurance races, the ideal WBGT is between 4.4°C to 15°C (40°F to 59°F), with rates of adverse medical events increasing outside this range and rising considerably once WBGT reaches >15.6°C (60°F).3
Medical race planners and responding volunteer race physicians can also anticipate levels of medical need and allocate medical assets based on specific locations along the racecourse. In multiyear studies of the Hawaii Ironman™ Triathlon4 and the Twin Cities Marathon™,5 most medical encounters occurred at the finish line as expected, with collapse being the most common presentation. The most common etiology of race collapse that occurs upon completion of an endurance race is generally benign and a consequence of exercise-associated postural hypotension caused by lower extremity blood pooling that occurs with cessation of activity (loss of the musculovenous pump). Collapse elsewhere on the course and any unheralded collapse during physical exertion signals heightened concern for much more serious pathology.6 Cardiac arrest is the most feared medical emergency but is very rare with an incidence of 0.54 per 100,000 half- and full-marathon participants.2 However, rates of other serious and potential life-threatening medical emergencies during distance races are higher, with an estimated 16 to 155 emergencies per 100,000 race entrants.7
Exertional Heat Stroke
Muscles generate heat during exercise that is normally dissipated through perspiration and increased blood flow to the skin. Exertional hyperthermia, which is defined as a core body temperature >40°C (104°F), occurs when heat production outpaces normal physiologic thermoregulatory mechanisms.8 Although physical exertion can be sustained for a period of time at hyperthermic body temperatures, exertional hyperthermia will eventually lead to organ failure, which is the core tenet of exertional heat stroke (EHS). EHS is a life-threatening diagnosis, accompanied by central nervous system disturbance and multiple organ system failure and requires immediate clinical recognition and intervention.8
Unsurprisingly, the incidence of EHS increases with warmer race conditions with the greatest risk when WBGT exceeds 28°C (82°F).9 In seminal work from Roberts, describing medical events over a 12-year period at the typically cool weather Twin Cities Marathon™, EHS cases averaged only 1-2 per 10,000 finishers.5 In contrast, in a much hotter and more humid event, the Falmouth Road Race, a short but intense 11.5 kilometer event, averaged an alarmingly high 21.3 EHS cases per 10,000 runners.10 As expected, heat index was found to be a strong predictor of EHS.10 Runner-specific characteristics that increase the risk of EHS include obesity, low physical fitness, lack of heat acclimatization, sleep deprivation, sweat gland dysfunction, sunburn, and recent illness.8,9 We also believe, based on our own experience overseeing the Peachtree Road Race, the largest 10-kilometer race held annually on July 4th in Atlanta, that race intensity increases the risk of exertional hyperthermia and EHS in combination with hot and humid race conditions. Finally, inadequate hydration increases the risk of EHS as heat dissipation is impaired by reduced sweating and skin blood flow.8,11
It is imperative to recognize EHS as a life-threatening race medicine emergency that demands immediate recognition and initiation of proper treatments. Symptoms of EHS are unfortunately nonspecific and may include confusion, dizziness, headache, hyperventilation, vomiting, diarrhea, seizures, and collapse. In the example Runner 1, the presence of altered mentation in the context of warm and humid weather conditions should lead to the diagnosis of EHS until proven otherwise. Diagnosis is confirmed with a rectally obtained core body temperature, but this should not delay initiation of care. Alternate forms of body temperature measurement may be unreliable as they are affected by ambient external conditions and superficial cooling measures.8 As such, clinical suspicion should guide treatment decisions in the absence of an immediate core body temperature.
EHS requires immediate whole-body cooling.9 Cold-water immersion in 1.7°C (35°F) to 15°C (59°F) water is the gold standard cooling modality.12 Once cooling is initiated, rectal temperature and vital signs should be monitored every 5 to 10 minutes and the athlete should be removed once the core body temperature reaches 38.9°C (102°F).9 If a cold water tub is not available, and in all cases of exertional hyperthermia, cycling ice-water soaked towels to the head, trunk, and extremities along with ice packs to the neck, axillae, and groin are recommended.8,9 For cases of EHS, this is a less-effective therapy.12 The athlete should be transported to a nearby hospital once the body temperature has been lowered. If the athlete exhibits any signs of hemodynamic instability or body temperature is not responsive to cooling measures within 15 to 20 minutes, urgent escalation of care is needed with expedited transfer to the hospital with cooling measures in place.13 In addition, it is important to keep in mind that the ambient temperature in the ambulance generally mandates continued use of cooling towels for any athlete with hyperthermia who necessitates transfer to the hospital for further care.
Hypothermia
While normal exercise physiology potentiates hyperthermia, this same physiology offers some protection against hypothermia. Hypothermia is defined as a core temperature below 35°C (95°F) and occurs when body heat is lost faster than can be generated through metabolic heat production. While the incidence of race-associated hypothermia is not well established, it is logical that the addition of rain and wind to cold race conditions leads to increased loss of body heat, which in turn increases the risk for hypothermia.14,15 In addition, body composition influences the risk for hypothermia as those with increased body fat, subcutaneous fat, and muscle mass are able to better maintain core temperatures compared to those with less fat and muscle. Women and individuals >60 years old are also at increased risk for hypothermia.15
Symptoms of hypothermia generally progress with decreases in body temperature. With mild hypothermia (32°C [89.6°F] to 35°C [95°F]), athletes may demonstrate confusion, slurred speech, and mild ataxia. Shivering is usually present, and athletes may exhibit tachycardia, hypertension, and tachypnea. With moderate hypothermia (28°C [82.4°F] to 32°C [89.6°F]), shivering may cease, but altered mentation may now be present. Heart rate, blood pressure, and respiratory rate may also decrease at this level. With severe hypothermia (<28°C [82.4°F]), individuals are generally nonresponsive and at substantial risk of cardiac arrest.15 Runner 2 displayed symptoms typically observed with mild hypothermia. It is important to note that symptoms can vary widely between individuals and that shivering is affected by many physiologic factors and may not be a reliable marker of the severity of hypothermia.15 Rectal temperature is the most accurate assessment of core temperature in suspected hypothermia.13
Athletes with suspected hypothermia should be gently and quickly transferred to a warm and dry environment and wet clothing should be promptly removed. Treatment should be initiated with passive rewarming using warm clothing, blankets, and drinks. Those with moderate hypothermia or any signs of altered mentation require active rewarming through application of heating pads, warm blankets, or warm air, and should be transported to a nearby hospital. If severe hypothermia or signs of cardiac instability are present, active rewarming measures should be applied and left in place as the athlete is immediately transferred to a hospital with advanced cardiac support capabilities.16 Those with moderate and severe hypothermia should be moved with caution as excess movement may incite arrhythmias at core temperatures <32°C (89.6°F).14,16
Exercise-Associated Hyponatremia
In Runner 3, with his normal core temperature, hyponatremia represented the most likely diagnosis. Exercise-associated hyponatremia (EAH) occurs when serum, plasma, or blood sodium concentration falls to <135 mmol/L during or up to 24 hours after physical activity.17 With symptoms attributed to cerebral edema, the diagnosis is exercise-associated hyponatremic encephalopathy (EAHE).18 The likelihood of developing EAHE generally increases with the severity of hyponatremia and is more common with sodium concentration <130 mmol/L. However, this relationship is unpredictable as EAHE can occur with serum sodium ≥130 mmol/L and asymptomatic EAH can still be present with serum sodium ≤125 mmol/L.19
The primary determinant of serum sodium concentration is total body sodium and potassium relative to total body water content. Excessive water intake disrupts this electrolyte to water balance and leads to the development of EAH.17,19 Increased race duration and distance, availability of drinking fluids, and weight gain are all associated with EAH. In addition, high or low body mass index, female sex, and extreme temperature are also associated with increased rates of EAH.18 Asymptomatic EAH is common with a reported incidence of 12-13% in marathon runners,20,21 and up to 51% in Ironman™ triathlon and ultramarathon races.18 Symptomatic EAH, however, is rare. Most endurance events report no cases, though isolated case reports are increasing in endurance sports and other physical activities.18
Like EHS, the clinical presentation of EAH is nonspecific. Mild symptoms include light headedness, nausea, and dizziness. More severe symptoms including headache, altered mental status, seizures, and respiratory distress are suggestive of EAHE and represent a medical emergency.18 Serum sodium monitoring is indicated in any athlete if symptomatic EAH or EAHE are suspected, particularly in the presence of normothermia.13 Point-of-care sodium analysis is now available and generally present at most large-scale endurance events. If sodium measuring capabilities are not available, athletes should be treated based on clinical assessment.18
With incidental asymptomatic hyponatremia, treatment is aimed at preventing further decreases in serum sodium. These athletes may be given oral hypertonic solution if serum sodium is <130 mmol/L (100 mL 3% saline with a sweetener or concentrated bouillon [4 bouillon cubes in 125 mL of water]). Athletes presenting with mild symptoms may be treated in similar fashion, although a bolus of 100 mL of intravenous hypertonic 3% saline may be alternatively administered to nauseated athletes. With signs of improvement, mildly symptomatic EAH athletes may be discharged but should be counseled to seek medical attention if any neurologic symptoms develop. Athletes presenting with severe symptoms of EAHE require immediate intravenous (IV) hypertonic saline with a 100 mL bolus of 3% saline solution, repeated up to twice if necessary. Emergent IV hypertonic saline should not be delayed for laboratory measurements. In the acute phase, osmotic demyelination that can occur with overcorrection of hyponatremia is of minimal concern.18 Athletes with EAHE should then be promptly transported to a hospital.
Our Clinical Approach and Additional Contemporary Concerns
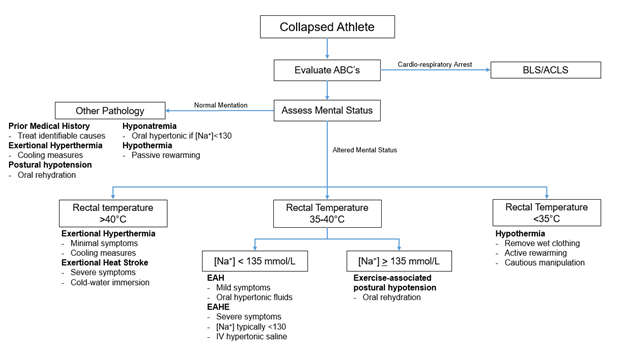
When evaluating a collapsed endurance athlete, medical personnel must consider many factors. Beginning with the race climate, certain pathologies that are non-cardiac in nature may or may not be more likely. The assessment of the athlete begins with the standard ABC's of initial emergency assessment. With intact vitals, hemodynamics, and mental status, postural hypotension or mild exertional hyperthermia may be present. The evaluation should continue with a core body temperature measurement and close clinical observation in the medical tent. All race medicine volunteers need to be cognizant of the possibility of EHS, hypothermia, and EAHE as these pathologies require timely intervention without delay. It is paramount to recognize that, 1) symptoms are not particularly sensitive or specific for classic race medicine pathologies, and 2) altered mental status is a hallmark of severe disease. An algorithm highlighting a simplified approach to the collapsed athlete is shown in Figure 1.
Figure 1. Algorithm for the Evaluation of the Collapsed Endurance Athlete. Courtesy of Tso J, Kim JH.
As US and international recreational athletes continue to increase in number and diversity, race medicine has also evolved in complexity with modern day challenges. Race directors and race medical directors are now charged with additional responsibilities beyond just ensuring the appropriate training and orientation of medical volunteers. Particularly for large-scale events, emergency medical planning is critical and involves the race staff, emergency officials in the city, and coordination with city emergency medical services (EMS) services to ensure the safety of race participants, volunteer staff, and residents of the city who are not involved with the event. The tragic events at the 2013 Boston Marathon have led to sobering new medical priorities in the consideration and planning for possible mass casualty events. Finally, the evolving COVID-19 pandemic necessitates careful logistic considerations for mass gatherings of individuals. Fortunately, endurance races occur outdoors, dramatically reducing the risk of disease transmission, though appropriate infection mitigation measures are still indicated and should follow the latest evidence-based recommendations. As such, the coordination of multiple organizations and medical assets in any city preparing for a large-scale recreational endurance race is critical and represents another important and new aspect of race medicine.
Conclusion
In the practice of race medicine, practitioners and medical volunteers must be familiar with both cardiac and non-cardiac pathologies observed in collapsed runners. In particular for non-cardiac diagnoses, EHS, hypothermia, and EAHE all represent emergencies that require immediate recognition and prompt treatment. Recognition is dependent on understanding specific risks that may be present among endurance athletes and risks associated with particular race climates. As interest peaks in recreational endurance exercise, the practice of race medicine embraces new complexities and challenges that require a team-based approach focused on organization, expertise in the care of race-specific medical pathology, and careful preparation for safe mass gatherings as well as possible catastrophic events.
References
- Running USA Releases 2019 U.S. Running Trends Report (RunningUSA website). 2019. Available at: https://www.runningusa.org/product/running-usa-releases-2019-u-s-running-trends-report/. Accessed 01/08/2019.
- Kim JH, Malhotra R, Chiampas G, et al. Cardiac arrest during long-distance running races. N Eng J Med 2012;366:130-40.
- Roberts WO. Heat and cold: what does the environment do to marathon injury? Sports Med 2007;37:400-03.
- Laird RH. Medical care at ultraendurance triathlons. Med Sci Sports Exerc 1989;21:S222-5.
- Roberts WO. A 12-yr profile of medical injury and illness for the Twin Cities Marathon. Med Sci Sports Exerc 2000;32:1549-55.
- Hoffman MD, Rogers IR, Joslin J, Asplund CA, Roberts WO, Levine BD. Managing collapsed or seriously ill participants of ultra-endurance events in remote environments. Sports Med 2015;45:201-12.
- Schwellnus MC, Kipps C, Roberts WO, et al. Medical encounters (including injury and illness) at mass community-based endurance sports events: an international consensus statement on definitions and methods of data recording and reporting. Br J Sports Med 2019;53:1048-55.
- Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc 2007;39: 556-72.
- Casa DJ, Demartini JK, Bergeron MF, et al. National Athletic Trainers' Association Position Statement: exertional heat illnesses. J Athl Train 2015;50:986-1000.
- Demartini JK, Casa DJ, Belval LN, et al. Environmental conditions and the occurrence of exertional heat illnesses and exertional heat stroke at the Falmouth Road Race. J Athl Train 2014;49:478-85.
- Montain SJ, Coyle EF. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol (1985) 1992;73:1340-50.
- Casa DJ, McDermott BP, Lee EC, Yeargin SW, Armstrong LE, Maresh CM. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev 2007;36:141-49.
- Childress MA, O'Connor FG, Levine BD. Exertional collapse in the runner: evaluation and management in fieldside and office-based settings. Clin Sports Med 2010;29:459-76.
- Fudge JR, Bennett BL, Simanis JP, Roberts WO. Medical evaluation for exposure extremes: cold. Wilderness Environ Med 2015;26:63-68.
- Castellani JW, Young AJ, Ducharme MB, Giesbrecht GG, Glickman G, Sallis RE. American College of Sports Medicine position stand: prevention of cold injuries during exercise. Med Sci Sports Exerc 2006;38:2012-29.
- Brown DJA, Brugger H, Boyd J, Paal P. Accidental Hypothermia. N Eng J Med 2012;367:1930-38.
- Rosner MH, Kirven J. Exercise-associated hyponatremia. Clin J Am Soc Nephrol 2006;2:151-61.
- Hew-Butler T, Rosner MH, Fowkes-Godek S, et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin J Sport Med 2015;25:303-20.
- Noakes TD, Sharwood K, Speedy D, et al. Three independent biological mechanisms cause exercise-associated hyponatremia: evidence from 2,135 weighed competitive athletic performances. Proc Natl Acad Sci USA 2005;102:18550-55.
- Almond CSD, Shin AY, Fortescue EB, et al. Hyponatremia among runners in the Boston Marathon. N Eng J Med 2005;352:1550-56.
- Kipps C, Sharma S, Pedoe DT. The incidence of exercise-associated hyponatraemia in the London marathon. Br J Sports Med 2011;45:14-19.
Clinical Topics: Arrhythmias and Clinical EP, Diabetes and Cardiometabolic Disease, Prevention, Sports and Exercise Cardiology, Vascular Medicine, Implantable Devices, SCD/Ventricular Arrhythmias, Exercise
Keywords: Sports, Athletes, Heat Exhaustion, Shock, Temperature, Body Temperature, Sodium, Humidity, Hypothermia, Physical Exertion, Hot Temperature, Hyponatremia, Sweating, Dizziness, Accidental Falls, Shivering, Hypotension, Orthostatic, Emergencies, Point-of-Care Systems, Marathon Running, Heat Stroke, Nausea, Body Composition, Central Nervous System, Adipose Tissue, Heart Arrest, Muscles, Subcutaneous Fat, Lower Extremity, Medical Staff, Algorithms, Hyperthermia, Induced, Reference Standards, Headache
< Back to Listings