Duration of Diabetes and Risk of Incident Heart Failure: Using the Past to Predict the Future
Among patients with type 2 diabetes mellitus (T2DM), heart failure (HF) is the second most common initial presentation of cardiovascular (CV) disease following only peripheral artery disease, while being more frequent than other atherosclerotic complications such as myocardial infarction (MI) and stroke.1 A large observational study of >270,000 patients suggested that optimal control of CV risk factors (e.g., blood pressure, cholesterol, smoking, albuminuria) and glycemic status may neutralize the excess risk of MI and stroke for patients with T2DM.2 However, there was no such relationship with respect to incident HF, and even patients with T2DM and optimal control of all factors carried a 45% higher risk of HF hospitalization compared with patients without T2DM.2 Once diagnosed, HF carries a prognosis comparable to many cancers with 5-year survival of approximately 50%, in addition to substantial healthcare costs.3
HF guidelines have traditionally recommended optimal management of risk factors and comorbidities for the prevention of new-onset HF. In 2017, for the first time, the American College of Cardiology (ACC)/American Heart Association (AHA) HF guidelines set forth a class IIA recommendation for using natriuretic peptide screening for individuals at risk of developing HF, with subsequent team-based care to prevent development of incident HF.4 However, the guidelines did not incorporate recommendations specific to patients with T2DM. Most recently, 2021 European Society of Cardiology (ESC) guidelines have given sodium-glucose co-transporter-2 (SGLT2) inhibitors a class IA recommendation in patients with T2DM at high risk of CV events to prevent HF hospitalizations.5 This recommendation was based on evidence derived from several clinical trials among high-risk patients with T2DM where SGLT2 inhibitors reduced the relative risk of HF events by 27% to 39%.
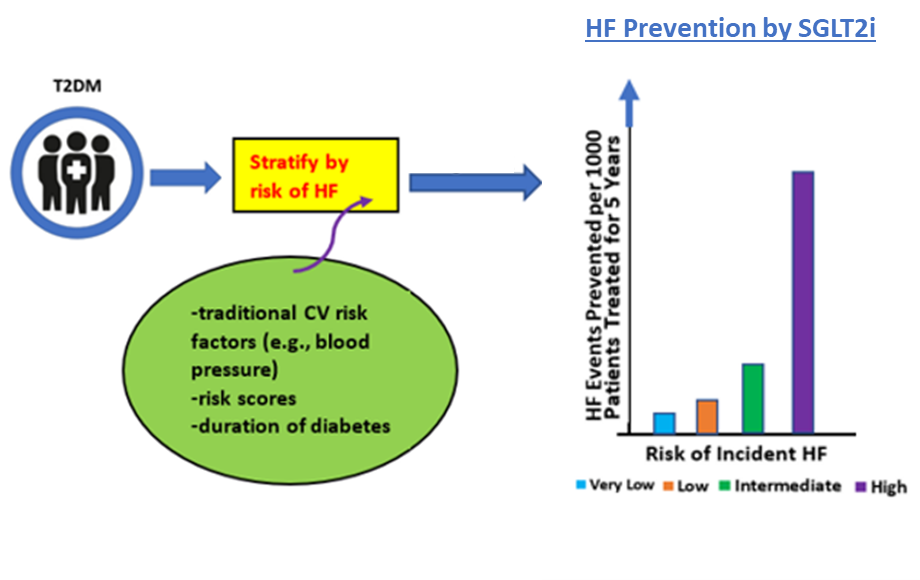
While optimal control of blood pressure and other cardiometabolic risk factors is important for all patients, identifying patients with T2DM at particularly high risk of HF may inform the most cost-efficient approach. For example, despite strong efficacy for HF prevention among patients with T2DM in clinical outcome trials, contemporary use of SGLT2 inhibitors has been low.6,7 Although likely multifactorial, lower utilization rates may partly relate to financial barriers. In this context, a series of studies have investigated risk scores for predicting the risk of incident HF events, which may identify subsets of patients with T2DM most likely to have clinically meaningful benefit with initiation of SGLT2 inhibitor therapy (Table 1). While these prior risk scores identified multiple factors associated with an increased likelihood of HF events, one factor not previously studied was the duration of T2DM.
Table 1: Select risk scores predicting incident HF in T2DM patients.
| Risk score | Variables included in the risk score | C-index (95% CI) |
| WATCH-DM8 | Weight [body mass index], age, hypertension, creatinine, high-density lipoprotein cholesterol, diabetes control [fasting plasma glucose], QRS duration, myocardial infarction, and coronary artery bypass graft. | 0.70 (0.67–0.72) |
| Random Survival Forest-based model8 | Weight [body mass index], age, hypertension, creatinine, high-density lipoprotein cholesterol, diabetes control [fasting plasma glucose], QRS duration, myocardial infarction, and coronary artery bypass graft. | 0.74 (0.72–0.76) |
| Model by Williams et al.9 | Age, coronary artery disease, blood urea nitrogen, atrial fibrillation, hemoglobin A1c, blood albumin, systolic blood pressure, chronic kidney disease, and smoking history. | 0.782* |
| Model by Yang et al.10 | Age, sex, body mass index, hemoglobin A1c, Log10 (urine albumin to creatinine ratio +1) and blood hemoglobin at baseline and coronary heart disease event during follow-up. | 0.853 (0.819–0.886) |
| Model by Pandey et al.11 | Biomarker risk score (high sensitivity troponin T ≥6 ng/L, NT-proBNP ≥125 pg/mL, high-sensitivity C-reactive protein ≥3 mg/L, left ventricular hypertrophy by electrocardiogram). | 0.74 (0.68-0.80) |
WATCH-DM, Weight [BMI], Age, hypertension, Creatinine, HDL-C, Diabetes control [fasting plasma glucose], QRS Duration, MI, and CABG; RSF, random survival forest; TIMI, Thrombolysis in Myocardial Infarction.
In this context, the analysis by Echouffo-Tcheugui and colleagues is a valuable addition to literature.12 The authors studied 9,734 participants with T2DM and without pre-existing HF or coronary artery disease enrolled in the ARIC (Atherosclerosis Risk in Communities) study, and assessed the association between duration of diabetes and subsequent risk of incident HF. A total of 1,968 HF events occurred over a median follow-up period of 22.5 years. The study showed that the risk of HF was higher among patients with longer T2DM duration. Specifically, every 5-year increase in diabetes duration was associated with a 17% increase in the risk of HF, with highest risk among those with a T2DM duration of ≥15 years (HR: 2.82; 95% CI: 2.22-3.63). The association of diabetes duration with risk of HF was most prominent among patients of self-reported Black race, women, those with hemoglobin A1C ≥7%, or a body mass index of ≥30 kg/m2. These findings are in line with previous studies that assessed the association between duration of diabetes and incidence of CV disease. An analysis from the Framingham Heart Study found that after adjustment for co-existing factors, the risk of coronary heart disease was 1.38 times higher for each 10-year increase in duration of diabetes.13 Similarly, analysis of the CRONOS-ADM (CoROnary CT aNgiography evaluation for clinical OutcomeS in Asymptomatic patients with type 2 Diabetes Mellitus) registry found longer diabetes duration associated with a higher prevalence, extent, and severity of coronary heart disease, as well as risk of major adverse CV and cerebrovascular events.14
The authors should be congratulated for an elegant analysis; however, a few limitations should be noted. The current analysis did not adjust for the duration of other risk factor burdens in the model. Patients with longer duration of T2DM will often have risk factors that may accompany or predispose them to diabetes such as long-standing hypertension, obesity, and inactivity. Confounding factors such as access to health care were also not considered. Patients with diabetes for a longer duration of time may have more contact with the healthcare system, which could contribute to a higher chance of incident HF diagnosis. Lastly, a significant graded association between duration of diabetes and incident HF risk was seen in obese individuals, but as such a graded relationship was not among patients who were not obese. This raises the possibility that cardiometabolic risk clustering may have been responsible for the association observed in this study.
In summary, duration of diabetes is a practical and simple variable that may be readily ascertained from the patient history and/or laboratory testing already embedded within routine clinical practice. Likewise, in addition to and/or complementary to available risk scores, duration of diabetes may be one factor to consider in the cost-efficient allocation of SGLT2 inhibitors to identify patients who stand to gain the most from initiation of this cardioprotective therapy.
Figure 1
References
- Shah AD, Langenberg C, Rapsomaniki E, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1·9 million people. Lancet Diabetes Endocrinol 2015;3:105-13.
- Rawshani A, Rawshani A, Franzén S, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2018;379:633-44.
- Taylor CJ, Ordóñez-Mena JM, Roalfe AK, et al. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000-2017: population-based cohort study. BMJ 2019;364:l223.
- Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 2017;70:776-803
- McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599-3726.
- Arnold SV, Inzucchi SE, Tang F, et al. Real-world use and modeled impact of glucose-lowering therapies evaluated in recent cardiovascular outcomes trials: an NCDR® Research to Practice project. Eur J Prev Cardiol 2017;24:1637-45.
- Arnold SV, de Lemos JA, Rosenson RS, et al. Use of guideline-recommended risk reduction strategies among patients with diabetes and atherosclerotic cardiovascular disease. Circulation 2019;140:618-20.
- Segar MW, Vaduganathan M, Patel KV, et al. Machine learning to predict the risk of incident heart failure hospitalization among patients with diabetes: the WATCH-DM risk score. Diabetes Care 2019;42:2298-2306.
- Williams BA, Geba D, Cordova JM, Shetty SS. A risk prediction model for heart failure hospitalization in type 2 diabetes mellitus. Clin Cardiol 2020;43:275-83.
- Yang X, Ma RC, So WY, et al. Development and validation of a risk score for hospitalization for heart failure in patients with type 2 diabetes mellitus. Cardiovasc Diabetol 2008;7:9.
- Pandey A, Vaduganathan M, Patel KV, et al. Biomarker-based risk prediction of incident heart failure in pre-diabetes and diabetes. JACC Heart Fail 2021;9:215-23.
- Echouffo-Tcheugui JB, Zhang S, Florido R, et al. Duration of diabetes and incident heart failure: the ARIC (Atherosclerosis Risk In Communities) study. JACC Heart Fail 2021;9:594-603.
- Fox CS, Sullivan L, D'Agostino RB Sr, Wilson PW. The significant effect of diabetes duration on coronary heart disease mortality: the Framingham Heart Study. Diabetes Care 2004;27:704-08.
- Kim JJ, Hwang BH, Choi IJ, et al. Impact of diabetes duration on the extent and severity of coronary atheroma burden and long-term clinical outcome in asymptomatic type 2 diabetic patients: evaluation by coronary CT angiography. Eur Heart J Cardiovasc Imaging 2015;16:1065-73.
Clinical Topics: Cardiovascular Care Team, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Lipid Metabolism, Nonstatins, Acute Heart Failure, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Computed Tomography, Nuclear Imaging, Hypertension, Diabetes and Cardiometabolic Disease
Keywords: Sodium-Glucose Transporter 2 Inhibitors, Glycated Hemoglobin A, Diabetes Mellitus, Type 2, Body Mass Index, Coronary Artery Disease, Albuminuria, Prevalence, American Heart Association, Peripheral Arterial Disease, Risk, Blood Pressure, Self Report, Computed Tomography Angiography, Laboratories, Cardiometabolic Risk Factors, Follow-Up Studies, Heart Failure, Cardiovascular Diseases, Prognosis, Natriuretic Peptides, Registries, Hypertension, Hospitalization, Myocardial Infarction, Health Care Costs, Stroke, Obesity, Neoplasms, Cholesterol, Cluster Analysis, Health Services Accessibility, Resource Allocation, Glucose, Sodium
< Back to Listings