Poll Results: Institutional Minimal Multidisciplinary Heart Team Requirements
The poll question revolves around the clinical scenario of man with a chronological age of 92 years with severe low gradient aortic stenosis. Please see complete details of the clinical vignette here.
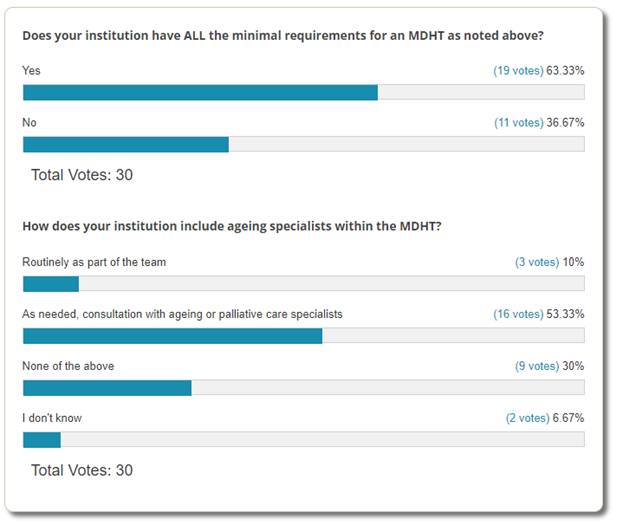
Among those who responded to the Poll: Institutional Minimal Multidisciplinary Heart Team Requirements, most feel that their institution currently does have ALL (interventional cardiologist, cardiac surgeon, echocardiographic and radiographic image specialist, clinical cardiology valve expertise, heart failure specialist, cardiovascular anesthesiologist, nurse practitioners/physician assistant, valve coordinator/program navigator, institutionally supported data manager, and hospital administrator representative) the minimal requirements for the multidisciplinary heart team (MDHT). However, only 10% reported having geriatric and palliative care specialists included as routine MDHT members with most having as needed consultation. Approximately a third of poll respondents reported no utilization of geriatric and palliative care specialists as part of the MDHT for structural heart disease care.
Further Details of the Patient Work-Up
Related to the 92-year-old patient described in the poll (see Medical History and Hospital Data here):
Cardiac Catheterization: Severe distal ostial left circumflex stenosis (felt not to increase peri-procedural risk and was not intervened upon), patent left anterior descending artery stent.
CT Chest (transcatheter aortic valve replacement (TAVR) protocol): Aortic valve annulus area 620 mm2 (Edwards Sapien S3 29 mm valve, +4.7% oversized), aortic valve annulus perimeter 91 mm2 (Medtronic Evolut™ 34 mm valve), valve angle 52°, left main coronary artery height 18 mm, right coronary artery height 22 mm, no left ventricular outflow tract (LVOT) calcium, moderate aortic valve calcium, minimal luminal area of 9 mm via right femoral access.
The MDHT met to discuss the case. The MDHT findings are listed below:
- Increased mortality risk due to age, NYHA class IV heart failure (at hospital presentation), and in-patient status (5.5% risk of in-hospital post-procedure mortality)1
- Increased risk of complete heart block requiring pacemaker due to baseline conduction disease
- Ostial circumflex disease unlikely to increase peri-procedural TAVR risk
- Increased infection risk due to open plantar ulcer
- Increased risk of acute kidney disease due to baseline chronic kidney disease
- Average risk valve anatomy and vascular access
Patient underwent successful deployment of a 29 mm Edwards Sapien S3 Ultra valve in the aortic position via femoral access with improvement in his valve hemodynamics (peak gradient 6 mmHg, mean gradient 3 mmHg, aortic valve area 2.8 cm2).
The procedure was complicated by complete heart block requiring permanent pacemaker and urinary retention requiring indwelling foley on discharge.
6-Month Follow-Up
Patient is alive and using a walker to ambulate. He still has an indwelling foley after multiple failed voiding trials and was seen in the emergency room once after a mechanical fall resulting in concussion. His ejection fraction has not improved.
See Expert Opinion from various members of the MDHT.
References
- Figulla HR, Lauten A, Hamm C, Lange R, Sack S, Mohr FW. TCT-715 Developing a TAVR risk score for the prediction of mortality after transcatheter aortic valve replacement. J Am Coll Cardiol 2014;64:B210.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Valvular Heart Disease, Implantable Devices, Aortic Surgery, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Acute Heart Failure, Interventions and Imaging, Interventions and Structural Heart Disease, Computed Tomography, Echocardiography/Ultrasound, Nuclear Imaging
Keywords: Aged, Aged, 80 and over, Transcatheter Aortic Valve Replacement, Aortic Valve, Anesthesiologists, Constriction, Pathologic, Coronary Vessels, Follow-Up Studies, Palliative Care, Patient Discharge, Stroke Volume, Urinary Retention, Aortic Valve Stenosis, Cardiac Catheterization, Stents, Heart Failure, Tomography, X-Ray Computed, Hospital Administrators, Renal Insufficiency, Chronic, Physician Assistants, Nurse Practitioners, Echocardiography, Emergency Service, Hospital, Referral and Consultation, Heart Block, Surveys and Questionnaires, Pacemaker, Artificial, Surgeons, Hospitals
< Back to Listings

