Poll Results: The Danger of Polypharmacy in the Older Adult With Heart Failure
A recent poll described a 74-year old man with New York Heart Association Class IV and Stage D heart failure (HF) secondary to ischemic cardiomyopathy requiring left ventricular assist device (LVAD) implantation as destination therapy, recurrent driveline infections necessitating lifelong antibiotics, paroxysmal atrial fibrillation, transient ischemic attack, hypertension, hyperlipidemia, chronic obstructive pulmonary disease, hypothyroidism, depression, anxiety, and insomnia presents with a 4-day history of recurrent falls at home and is admitted to the hospital after a witnessed syncopal episode without anteceding cardiac symptomatology or seizure semiology. You can find more details about the case here.
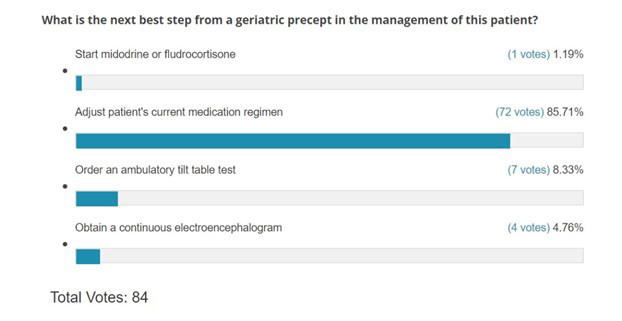
Below find readers' votes on the next best step for management of this patient.
Fludrocortisone and midodrine have been utilized in the past as pharmacological treatment options in the management of orthostatic hypotension. Fludrocortisone works as a volume expander by enhancing sodium reabsorption and total body water, while midodrine is a peripheral alpha-1adrenergic agonist that promotes both arterial and venous constriction. The mechanisms of these agents lead to an effective increase in systemic blood pressure. They should be avoided in patients with preexisting systolic or diastolic cardiac dysfunction, as higher systemic pressures can cause increased left ventricular afterload and myocardial stress which can exacerbate HF symptoms and ultimately lead to circulatory collapse.1 The association of these medications' use and hospitalizations when initiated in patients with HF and orthostatic hypotension has been outlined in previous studies.2 Furthermore, the mean arterial pressure (MAPs) for this LVAD patient were found to be within acceptable limits, further advising against the use of these agents.
The patient is currently on spironolactone and losartan as part of his goal directed therapy and is taking them in conjunction with multiple agents with known anticholinergic and central nervous system depressant properties. Among them include methocarbamol, gabapentin, and hydrocodone. Although there are no absolute contraindications to using these medications in the elderly, they have been listed on the 2019 American Geriatrics Society (AGS) Beers Criteria® as agents to avoid in individuals older than 65 due to their increased risk of causing altered mentation, drowsiness, dizziness, ataxia, and falls with subsequent injury.3 While trazodone has shown efficacy as an antidepressant and sleep aid in the elderly population, it too can contribute to orthostatic hypotension, enhance psychomotor dysfunction, and amplify the effects of other central nervous system depressants.4 The combination of these medications with antihypertensives in the setting of multiple underlying comorbidities and age-related changes involving hemodynamics and autonomic functioning can significantly impair an elderly individual's physiologic compensatory response to hypotensive stress, ultimately predisposing him to orthostasis and syncope.5 Frequently, clinicians quickly assume that patients' medical complexities and comorbidities, including severe heart disease requiring advanced therapies, are the main culprits to the presenting symptoms, and while this may be the case, other potential external inciters should be heavily considered. It is therefore imperative that the initial geriatric assessment of these patients begin with a detailed medication reconciliation, eliminating unnecessary drugs and/or adjusting dosages to mitigate side effects and drug interactions.6 Sometimes patients will find greater relief with removal of attending agents rather than adding on additional drugs that may interact significantly with other medically necessary medications.7 Our experts agree that adjusting the patient's current medication regimen is the best choice in this case.
Tilt table testing should be employed when the diagnosis remains unclear and neurally mediated syncope, specifically a vasovagal reaction, is strongly suspected, as the hemodynamic changes and prodromal symptoms identified with a positive head-up tilt test have been comparable to spontaneous vasovagal syncope.8 While it is important to consider multifactorial etiologies to a syncopal episode, tilt table testing is generally not indicated when an alternative cause has been established or when additional investigation for neurally mediated events would not change the patient's overall management. Additionally, while not impossible, the chance of circulatory collapse with a continuous flow durable LVAD with normal function and no alarms on interrogation is very unlikely.
The American College of Radiology Choosing Wisely® organization along with several clinical guidelines and multidisciplinary task forces recommend against extensive imaging for syncope unless there is strong suspicion based on the clinician's history and physical.9 During the initial assessment, providers should inquire about and evaluate for postictal states, tongue biting and/or residual focal neurologic deficits. Although the patient experienced subtle jerking during the episode, this was most likely representative of convulsive syncope as he did not exhibit other features consistent with a primary neurologic event. The utility of diagnostic tests such as head computed tomography, carotid doppler imaging and electroencephalography in the absence of seizure or stroke symptoms is limited as they have low sensitivity and specificity in identifying lesions contributing to syncope.10 While LVAD patients may develop cerebral hemorrhage if they are supratherapeutic with anticoagulation, a normal international normalized ratio (INR) range for a patient on warfarin and the lack of focal neurological deficits make a primary neurologic event less likely.
References
- Tremblay JA, Laramée P, Lamarche Y, et al. Potential risks in using midodrine for persistent hypotension after cardiac surgery: a comparative cohort study. Ann Intensive Care 2020;10:121.
- Grijalva CG, Biaggioni I, Griffin MR, Shibao CA. Fludrocortisone is associated with a higher risk of all‐cause hospitalizations compared with midodrine in patients with orthostatic hypotension. J Am Heart Assoc 2017;6:e006848.
- American Geriatrics Society. American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2019;67:674-94.
- Cuomo A, Bianchetti A, Cagnin A, et al. Trazodone: a multifunctional antidepressant. Evaluation of its properties and real-world use. J Gerontol Geriatr 2021;69:120-29.
- Magkas N, Tsioufis C, Thomopoulos C, et al. Orthostatic hypotension: from pathophysiology to clinical applications and therapeutic considerations. J Clin Hypertens (Greenwich) 2019;21:546-54.
- Rivasi G, Rafanelli M, Mossello E, Brignole M, Ungar A. Drug-related orthostatic hypotension: beyond anti-hypertensive medications. Drugs Aging 2020;37:725-38.
- Thijs RD, Brignole M, Falup-Pecurariu C, et al. Recommendations for tilt table testing and other provocative cardiovascular autonomic tests in conditions that may cause transient loss of consciousness: consensus statement of the European Federation of Autonomic Societies (EFAS) endorsed by the American Autonomic Society (AAS) and the European Academy of Neurology (EAN). Clin Auton Res 2021;31:369-84.
- Wong CW. Complexity of syncope in elderly people: a comprehensive geriatric approach. Hong Kong Med J 2018;24:182-90.
- American College of Radiology. ACR Appropriateness Criteria Syncope® (acsearch.acr.org). 2020. Available at: https://acsearch.acr.org/docs/3128014/Narrative/. Accessed 07/20/2022.
- Brignole M, Moya A, de Lange FJ, et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J 2018;39:1883-1948.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Dyslipidemia, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Anticoagulation Management and Atrial Fibrillation, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Lipid Metabolism, Novel Agents, Statins, Acute Heart Failure, Heart Transplant, Mechanical Circulatory Support, Interventions and Imaging, Interventions and Vascular Medicine, Echocardiography/Ultrasound, Hypertension
Keywords: Heart-Assist Devices, Arterial Pressure, Calcium, Fludrocortisone, Gabapentin, Hydrocodone, International Normalized Ratio, Losartan, Methocarbamol, Metoprolol, Mexiletine, Midodrine, Pantoprazole, Pravastatin, Spironolactone, Thyroxine, Venlafaxine Hydrochloride, Warfarin, Heart Ventricles, Heart Rate, Atrial Fibrillation, Dizziness, Hyperlipidemias, Hypotension, Orthostatic, Ischemic Attack, Transient, Reference Values, Respiratory Rate, Tilt-Table Test, X-Rays, Heart Failure, Heart Transplantation, Electrocardiography, Amiodarone, Syncope, Pulmonary Disease, Chronic Obstructive, Neurologic Examination, Electroencephalography, Emergency Service, Hospital, Ultrasonography, Doppler, Lower Extremity, Cholecalciferol, Hospitalization, Hypothyroidism, Cardiomyopathies, Craniocerebral Trauma, Hypertension, Anti-Bacterial Agents, Cephalexin, Pacemaker, Artificial, Tomography, Ischemia, Telemetry, Hospitals, Anxiety, Aspirin, Glucose, Geriatrics
< Back to Listings
