How to Best Screen For and Manage Carcinoid Heart Disease
Quick Takes
- Screening for carcinoid heart disease (CHD) using N-terminal pro–B-type natriuretic peptide levels and echocardiography is recommended in all patients with metastatic carcinoid tumor.
- Echocardiography is the key investigation for the identification and follow-up of CHD, which usually affects the right-sided cardiac valves.
- Bioprosthetic valve replacement is undertaken for severely diseased valves, with close monitoring required for potential bioprosthetic valve thrombosis.
Carcinoid heart disease (CHD) is a complex, hormonal sequelae of secretory neuroendocrine tumors (NETs). NETs and their metastases secrete multiple hormonal amines and peptides. Carcinoid syndrome (CS) is due to systemic elevation of serotonin levels or its metabolite 5-hydroxyindoleacetic acid. Other hormones including histamine, tachykinins, kallikrein, and prostaglandins are secreted by NETs and contribute to symptoms.1,2 The primary symptoms of CS can include diarrhea, skin flushing, and bronchospasm. Most NET primaries are intestinal, with gastroenteropancreatic sites accounting for an incidence of 3.6 per 100,000, followed by lung NETs and then those located in the gonads or thymus, or of unknown origin.3
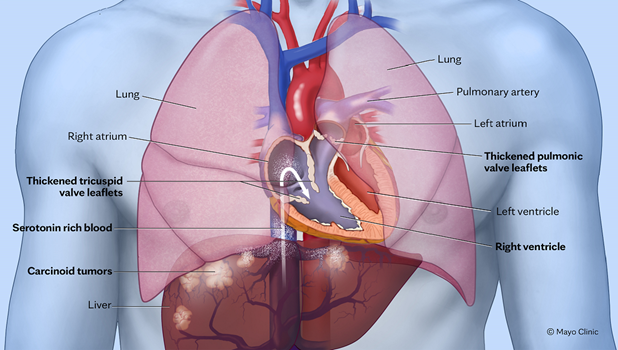
CHD arises because of plaque-like, fibrous deposits on right-sided heart valves (the tricuspid and pulmonic valves) and right-sided chamber endocardium, caused by serotonin-related stimulation of fibroblast growth and fibrogenesis. Carcinoid plaques result in thickening, retraction, and immobility of the tricuspid valve leaflets and subtricuspid apparatus, as well as of the pulmonic valve cusps (Figure 1).1 Generally, CHD develops when hepatic metastases of NETs are present. Left-sided valve involvement (the aortic and mitral valves) is rare because serotonin is enzymatically inactivated in lung vessels by monoamine oxidase. Left-sided valve disease may arise when a patent foramen ovale or atrial septal defect allows a right-to-left shunt or very high circulating levels of vasoactive substances that may overwhelm hepatic and pulmonary degradative capacity.1
Figure 1: Neuroendocrine Tumor Metastases in the Liver Releasing Serotonin
Illustration demonstrating NET metastases in the liver releasing serotonin, which in turn has caused thickening and retraction of the pulmonic and tricuspid valves as well as endocardial thickening in the RV.
NET = neuroendocrine tumor; RV = right ventricle.
Tricuspid and pulmonary valves in CHD are more frequently affected by regurgitation than stenosis. This phenomenon eventually leads to right ventricular (RV) volume overload and right-sided heart failure (HF). Those with CHD and severe symptoms have reduced survival rates, with 3-year rates reported as low as 30%.2 In addition, New York Heart Association (NYHA) class, age, and abnormal creatinine levels have been associated with increased mortality rates.4
All patients with CS are recommended to have a detailed cardiac history and examination. If signs or symptoms of cardiac involvement are present, N-terminal pro–B-type natriuretic peptide (NT-proBNP) levels and transthoracic echocardiography (TTE) are recommended for further evaluation. If there are no cardiac signs or symptoms, periodic screening with NT-proBNP levels can be considered, with levels >260 ng/mL warranting further evaluation with TTE.1,2 Identification of CHD or other pathology by TTE warrants referral to a cardiologist with expertise in CHD. The 2017 expert consensus document recommends ongoing follow-up with NT-proBNP levels if TTE findings are unremarkable, and with surveillance TTE every 6 months for mild CHD and every 3 months for moderate or greater CHD.2 This recommendation differs from the European Neuroendocrine Tumor Society (ENETS) recommendation of yearly TTE surveillance in cases of nonsevere CHD.1
TTE remains the mainstay both for the diagnosis and grading of severity of valvular disease. However, multimodality imaging evaluation may be required in CHD. Cardiac magnetic resonance imaging may further assess RV size and function and define cardiac metastases. Cardiac metastases have been reported in 1.75% of patients undergoing DOTATATE positron emission tomography (PET) for staging in all-comers with NETs.5 DOTATATE PET remains the most common method for the detection of cardiac metastases; gallium-68–DOTATATE labeled somatostatin analogue is used as a PET tracer that targets somatostatin receptor subtype 2 expressed on the NET cell membranes, and tumor foci are detected as hot spots.5 Cardiac computed tomography may play a role in excluding coronary artery disease in preoperative patients and further evaluate cardiac anatomy, particularly the RV outflow tract, before intervention.
Once RV failure develops, diuretic therapy becomes the mainstay of medical care. However, the preferred treatment to avoid significant HF and improve long-term prognosis involves valve replacement. Indications for valve replacement in CHD are the same as the standard indications outlined by American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Management of Patients With Valvular Heart Disease for those without NET, and include the presence of severe, symptomatic valvular heart disease, or associated ventricular enlargement or dysfunction.6 An additional indication for intervention in severe tricuspid regurgitation (TR) is prior to planned liver tumor resection surgery to minimize bleeding risk associated with significant right atrial pressure elevation.1
Surgical valve replacement is recommended because repair is not possible in the setting of thickened and damaged valve leaflets and cusps. Bioprosthetic valves are generally preferred because right-sided mechanical valves have increased thrombosis and bleeding risks with warfarin anticoagulation and have overall worse prognosis.7 Postoperative anticoagulation for bioprostheses is generally undertaken for ≥6 months. CHD may be associated with increased risk of bioprosthetic valve thrombosis, which may respond to long-term anticoagulation. Experienced anesthesiology support is essential during surgical valve replacement due to the risk of carcinoid crisis, which can result in life-threatening hypotension. Anesthesiology protocols to prevent carcinoid crisis often include preoperative treatment with somatostatin analogues (e.g., octreotide) for ≥2-4 weeks to prevent release of serotonin, and intravenous (IV) octreotide infusion commencing before induction with anesthesia and continued both intraoperatively and postoperatively. Intraprocedural hypotension should be managed as a carcinoid crisis using additional IV boluses of octreotide.
There is emerging potential for percutaneous valve replacement interventions in this population, although there are no specific data for CHD. Transcatheter valve-in-valve implantation may be useful in patients with bioprosthetic degeneration. Percutaneous pulmonic valve replacement has been widely applied in the congenital population and in select patients with CHD deemed high risk for surgery. If percutaneous pulmonic valve bioprostheses are not suitable due to pulmonary annulus dilation or narrowing, a prestent can be deployed as a scaffold before transcatheter valve bioprosthesis placement. Percutaneous tricuspid valve replacement technologies are currently under investigation and may play a role for severe TR in patients who are not operative candidates, although patients with CHD have generally been excluded from clinical trials. Tricuspid edge-to-edge repair (TEER) is being increasingly used for TR; however, TEER is generally not considered for significant TR in this population because carcinoid plaques leave the tricuspid leaflets retracted and fixed, which limits the ability to percutaneously deploy clips.
In summary, CS is characterized by flushing and diarrhea predominantly in patients with liver metastases. Serotonin-induced endocardial proliferation results in carcinoid plaques, predominantly affecting the tricuspid and pulmonic valves, with regurgitation being a more prominent manifestation than stenosis. Severe valvular CHD may result in right-sided HF, which is associated with poor prognosis. Screening for cardiac disease is recommended for all patients with metastatic NET or CS by way of history, physical examination findings, NT-proBNP levels, and TTE findings. Bioprosthetic valve replacement is generally undertaken for symptomatic right-sided valve disease. Close surveillance for bioprosthetic valve thrombosis is recommended. Patients with advanced CHD should be managed at centers with experience managing patients with CHD, using a multidisciplinary care team approach with close coordination between the cardiologist, cardiac surgeon, oncologist, cardiac anesthesiologist, and other specialists.
References
- Grozinsky-Glasberg S, Davar J, Hofland J, et al. European Neuroendocrine Tumor Society (ENETS) 2022 guidance paper for carcinoid syndrome and carcinoid heart disease. J Neuroendocrinol 2022;May 25:[ePub ahead of print].
- Davar J, Connolly HM, Caplin ME, et al. Diagnosing and managing carcinoid heart disease in patients with neuroendocrine tumors: an expert statement. J Am Coll Cardiol 2017;69:1288-304.
- Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol 2017;3:1335-42.
- Nguyen A, Schaff HV, Abel MD, et al. Improving outcome of valve replacement for carcinoid heart disease. J Thorac Cardiovasc Surg 2019;158:99-107.e2.
- Wang Y, Ayoub C, Yang AF, et al. Gastroenteropancreatic neuroendocrine tumor metastasis to the heart: evaluation of imaging manifestations. Curr Probl Diagn Radiol 2023;52:340-5.
- Otto CM, Nishimura RA, Bonow RO, et al.; Writing Committee Members. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021;77:e25-e197.
- Connolly HM, Schaff HV, Abel MD, et al. Early and late outcomes of surgical treatment in carcinoid heart disease. J Am Coll Cardiol 2015;66:2189-96.
Clinical Topics: Valvular Heart Disease, Cardio-Oncology, Noninvasive Imaging
Keywords: Carcinoid Heart Disease, Tricuspid Valve, Pulmonary Valve Insufficiency
< Back to Listings