Coronary Artery Calcium and Polygenic Risk Scores For Cardiovascular Risk Prediction: Results From Two Population-Based Studies
Quick Takes
- In the present analysis of two observational population-based cohorts of middle-aged to older adults, the coronary artery calcium (CAC) score provided better discrimination for coronary heart disease risk prediction than did polygenic risk scores (PRS) in middle-aged and older adults.
- Risk discrimination is significantly improved when the CAC score is added to traditional risk factors, but not when PRS are added.
- An integrative approach involving a combination of the CAC score and PRS may improve risk stratification, particularly at younger ages.
Commentary based on Khan SS, Post WS, Guo X, et al. Coronary artery calcium score and polygenic risk score for the prediction of coronary heart disease events. JAMA 2023;329:1768-77.1
Cardiovascular disease (CVD) risk estimation is a critical component of clinician–patient shared decision making, which is used to guide the initiation and intensification of preventive therapies.2 The Pooled Cohort Equations (PCE) are recommended by the American College of Cardiology (ACC) and American Heart Association (AHA) for risk stratification. Despite challenges with overestimation and underestimation of risk, these traditional risk models guide lipid-lowering pharmacotherapy initiation (e.g., PCE risk >7.5% and selectively in those with a risk of 5-7.4%).2
Coronary artery calcium (CAC) imaging is a guideline-endorsed, cost-effective risk-prediction tool that provides a noninvasive assessment of subclinical atherosclerosis and integrates an individual's lifetime exposure to measured and unmeasured risk factors.2 Polygenic risk scores (PRS) provide a weighted sum of risk across common genetic variants and are associated with subclinical and clinical coronary heart disease (CHD).3 A significant knowledge gap reiterated by the 2022 AHA scientific statement on PRS for CVD was the utility of the CAC score versus PRS in risk discrimination and reclassification.3
In this setting, Khan et al. assessed the change in discrimination when the CAC score or PRS is added to a CHD risk-prediction model incorporating traditional risk factors.1 This analysis included participants 45-79 years of age without known CHD from the MESA (Multi-Ethnic Study of Atherosclerosis) and the RS (Rotterdam Study).1
Methods
The 2013 ACC/AHA PCE were used to calculate each participant's 10-year atherosclerotic cardiovascular disease (ASCVD) risk and fitted to the RS sample to derive the PCE-RS. The CAC score was calculated using the Agatston method in both cohorts. CHD PRS were calculated for each participant using a reweighting process involving several single-nucleotide polymorphisms.1 Incident CHD was defined as fatal or nonfatal myocardial infarction (MI) and CHD death in the RS and as MI, definite or probable angina if followed by revascularization, resuscitated cardiac arrest, and CHD death in the MESA.1 The present analysis included only individuals of European ancestry or self-reported white race specifically in the MESA, resulting in a final sample of 1,991 in the MESA and 1,217 in the RS.1
Main Findings
The median predicted ASCVD risk was approximately 7% in the MESA and 6% in the RS. Incident CHD was approximately 9% in the MESA over a median follow-up of 16 years and 8% in the RS over a median follow-up of 14 years.1
There was a dose–response relationship between CAC scores and CHD rates shown in the data from both studies. However, CHD rates were higher for those with PRS >80%. Regarding model performance, there was a significant change in C-statistic estimates when the CAC score was added to the PCE (0.09; 95% confidence interval [CI], 0.06-0.13), but this result was not observed when PRS were added to the PCE. Similarly, overall categorical net reclassification improvement was significant only with the CAC score being added to the PCE (0.19; 95% CI, 0.06-0.28), not with PRS being added (0.04; 95% CI, -0.05 to 0.1).1 There was no additive predictive utility with both scores added to the PCE compared with the CAC score alone, with overall study findings consistent across age groups as shown by subanalyses among younger and older participants.1
Discussion
In this population-based cohort, the CAC score was better at CHD risk discrimination than were PRS in adults of European ancestry with a median age of 61 years in the MESA and 67 years in the RS.1 These findings are not surprising because the CAC score is a direct measure of subclinical ASCVD whereas PRS assess common genetic variants. This analysis was focused on middle-aged to older adults, which may have accounted for some of the differences noted between the CAC score and PRS. Some studies have reported marginal but significant discrimination when PRS were added to the PCE in relatively younger patients, for whom the traditional ASCVD risk scores may perform poorly.4
In this regard, PRS may be useful in targeting young adults (age <35 years) at high risk to undergo early CAC screening.5 This approach will be particularly useful in the early detection of conversion to CAC score >0.6 From a practical standpoint, the CAC score is an easier test to complete as part of preventive risk assessment, although PRS and the CAC score both provide complementary risk-assessment information. Higher PRS are associated with a greater burden of subclinical atherosclerosis, and individuals with higher PRS may derive greater absolute and relative benefits from lipid-lowering therapy.7 It is not yet apparent whether knowledge of PRS connotes the same motivation to adhere to preventive therapies as knowledge of the CAC score.6
Going forward, an integrative approach involving a combination of the CAC score, PRS, and emerging technologies such as multiomics may improve risk stratification, particularly at an early age.8 The addition of PRS to the CAC score in this study did not result in meaningful improvement in risk prediction even among participants with a CAC score of 0, lending credence to the concept of the "power of zero."9 In a separate study among individuals with no CAC, ASCVD PRS were associated with ASCVD events, largely driven by stroke-related genetic variants but not CHD.10
The analysis by Khan et al. was limited to white participants or those of European ancestry due to PRS being derived in this population. The lack of a diverse sample limits the generalizability of the analysis findings. The authors highlight that efforts to incorporate transethnic or multiancestry CHD PRS may be beneficial in minority groups.1 The CAC score has an advantage in this regard because of its ability to predict risk across multiple racial and ethnic groups.2 Currently, there are no guidelines endorsing PRS use and a consensus on the ideal PRS may be lacking.6
In summary, the results of this analysis incorporating two observational population-based cohorts of middle-aged to older adults based in the United States and The Netherlands showed that the CAC score provides better discrimination than does PRS for CHD risk prediction (Figure 1).1 These findings emphasize the recommendations of the 2019 ACC/AHA Guideline on the Primary Prevention of CVD to selectively use the CAC score to refine risk for individuals with borderline to intermediate ASCVD risk if the clinician–patient decision to start a statin is unclear.2 Nonetheless, it is likely that PRS may be complementary to the CAC score when used for risk prediction. Alternatively, PRS may be a tool used to identify those who would derive the most benefit from CAC testing to help guide statin use, particularly younger patients. Clinicians await ongoing data comparing the CAC score and PRS.1
Figure 1: Coronary Artery Calcium vs. Polygenic Risk Scores
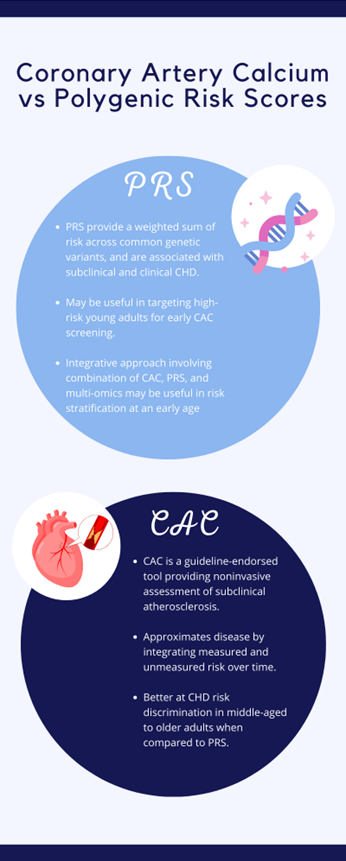
CAC = coronary artery calcium; CHD = coronary heart disease; PRS = polygenic risk scores.
References
- Khan SS, Post WS, Guo X, et al. Coronary artery calcium score and polygenic risk score for the prediction of coronary heart disease events. JAMA 2023;329:1768-77.
- Osei AD, Khan R, Grandhi GR, et al. Coronary artery calcium measurement to assist in primary prevention decisions for aspirin and lipid-lowering therapies. Curr Cardiovasc Imaging Rep 2021;14:1-9.
- O'Sullivan JW, Raghavan S, Marquez-Luna C, et al.; American Heart Association Council on Genomic and Precision Medicine, Council on Clinical Cardiology, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiovascular Radiology and Intervention, Council on Lifestyle and Cardiometabolic Health, Council on Peripheral Vascular Disease. Polygenic risk scores for cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2022;146:e93-e118.
- Emdin CA, Xia R, Agrawal S, et al. Polygenic score assessed in young adulthood and onset of subclinical atherosclerosis and coronary heart disease. J Am Coll Cardiol 2022;80:280-2.
- Severance LM, Carter H, Contijoch FJ, McVeigh ER. Targeted coronary artery calcium screening in high-risk younger individuals using consumer genetic screening results. JACC Cardiovasc Imaging 2021;14:1398-406.
- Blaha MJ. Predicting age of conversion to CAC >0: a role for polygenic risk scores? JACC Cardiovasc Imaging 2021;14:1407-9.
- Natarajan P, Young R, Stitziel NO, et al. Polygenic risk score identifies subgroup with higher burden of atherosclerosis and greater relative benefit from statin therapy in the primary prevention setting. Circulation 2017;135:2091-101.
- Gaine SP, Yoo E, Duvall C, Matasic D, Blumenthal RS, Whelton SP. Emerging Techniques For Cardiovascular Risk Assessment and Prevention (American College of Cardiology website). 2022. Available at: https://www.acc.org/Latest-in-Cardiology/Articles/2022/09/12/11/09/Emerging-Techniques-For-Cardiovascular-Risk-Assessment-and-Prevention. Accessed 04/01/2024.
- Nasir K. Message for 2018 cholesterol management guidelines update: time to accept the power of zero. J Am Coll Cardiol 2018;72:3243-5.
- Al Rifai M, Yao J, Guo X, et al. Association of polygenic risk scores with incident atherosclerotic cardiovascular disease events among individuals with coronary artery calcium score of zero: the multi-ethnic study of atherosclerosis. Prog Cardiovasc Dis 2022;74:19-27.
Clinical Topics: Prevention, Noninvasive Imaging, Dyslipidemia, Vascular Medicine
Keywords: Calcium, Risk, Risk Factors, Coronary Disease, Primary Prevention
