PROSPECT II: High hsCRP Level Indicates High-Risk Vulnerable Plaque Post NSTEMI
A high baseline level of high-sensitivity C-reactive protein (hsCRP) may indicate pan-coronary atherosclerosis and focal high-risk plaques in patients with a recent NSTEMI, according to a substudy of PROSPECT II published April 23 in JACC: Cardiovascular Interventions.
In the PROSPECT II trial, researchers used three-vessel imaging with near-infrared spectroscopy (NIRS) and IVUS to characterize untreated nonculprit lesions (NCLs) following the treatment of all flow-limiting lesions in 501 NSTEMI patients (median age 63 years; 17% women; 15% with diabetes).
In this analysis, Ole Fröbert, MD, et al., examined the association between plaque morphology and baseline hsCRP levels; about 51% were in the high hsCRP group (>3 mg/L), 36% in the intermediate CRP group (1-3 mg/L) and 14% in the low CRP group (<1mg/L).
The median baseline hsCRP level was 3.1 mg/L. Those with a higher hsCRP level were more likely to have a higher white blood cell count, greater BMI, history of current or recent smoking, and previous stroke or transient ischemic attack. Those with lower hsCRP levels were more likely to have higher high-density lipoprotein levels and history of previous MI or PCI.
Results from the primary imaging endpoints showed that the percentage of patients with at least one highly lipidic plaque with a maximum lipid core burden index for any 4-mm pullback length [MaxLCBI4mm] ≥324.7 increased from 39.4% to 57.2% to 59.3% in the low, intermediate and high groups (p=0.01). Similarly, the proportion of patients with at least one highly lipidic plaque with MaxLCBI4mm ≥324.7 and ≥70% burden increased from 22.7% to 27.2% to 36.7% (p=0.01). Each one-unit increase in log-transformed hsCRP was associated with a 33% increase in the odds of one or more highly lipidic NCL.
While older age was also independently associated with highly lipidic NCLs, LDL-C, history of smoking, diabetes and sex were not. Similar trends were seen for correlates of NCLs and high-risk plaque features.
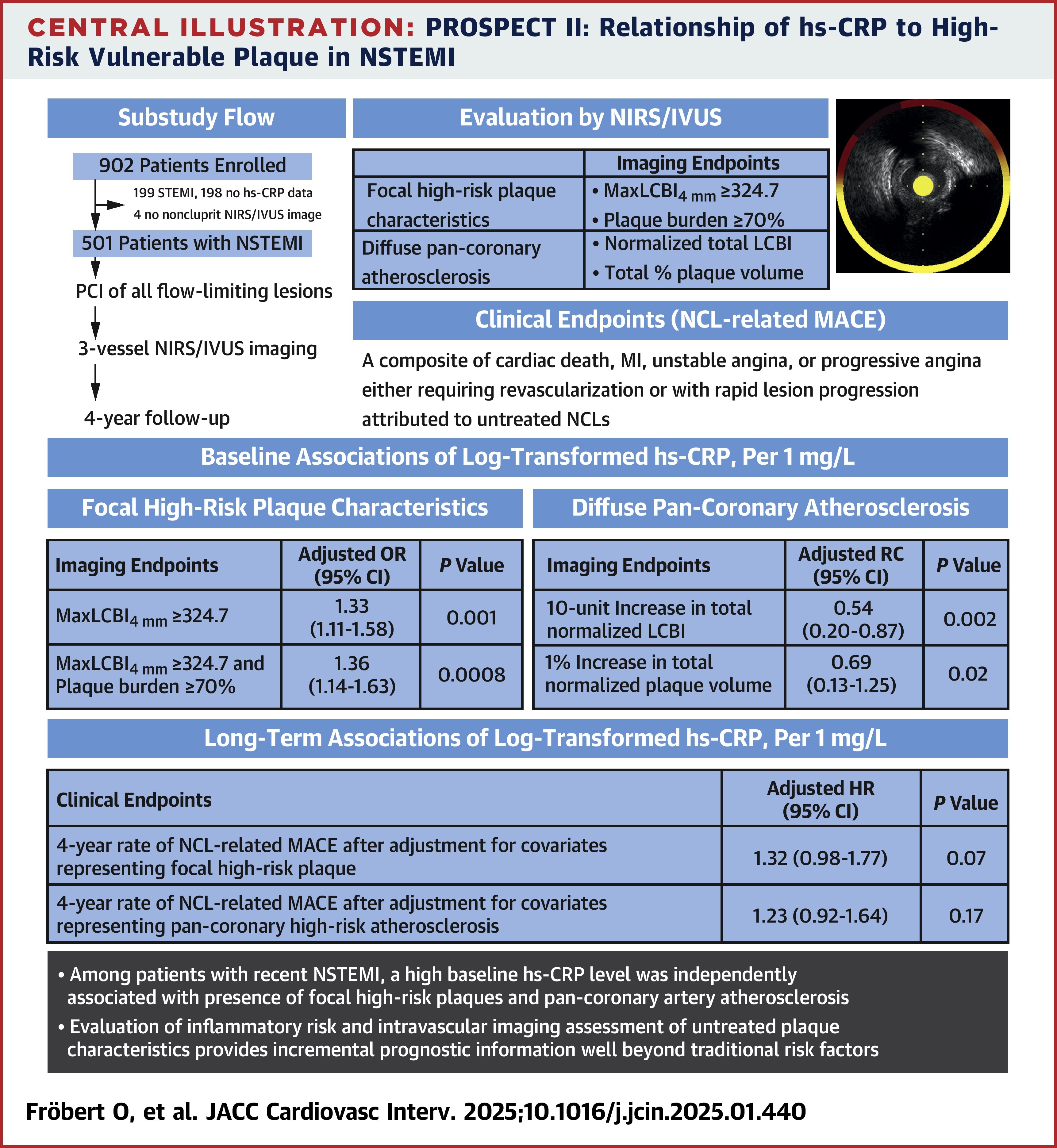
An analysis of imaging endpoints for diffuse pan-coronary atherosclerosis found that in a multivariable linear regression model, hsCRP was an independent predictor of a 10-unit increase in total normalized liquid core burden index (LCBI; p=0.002) and an increase in total normalized plaque volume (p=0.02).
While rates of major adverse cardiac events increased from 3.3% to 6.7% to 8.2% in the low, intermediate and high hsCRP groups at four years, the analysis did not reach statistical significance.
"The novelty of this study lies in integrating hsCRP with advanced imaging techniques such as NIRS and IVUS, linking biochemical markers to detailed structural plaque characteristics," write the authors. They add that, "Routine evaluation of inflammatory risk and intravascular imaging of untreated plaques provide prognostic information beyond traditional risk factors and may be used to tailor revascularization in the future."
In an accompanying editorial comment, Paul M. Ridker, MD, MPH, FACC, writes that, "the current data confirming prognostic information from hsCRP that augments and differs from information gleaned from [LDL-C] support concepts related to universal hsCRP screening in multiple cardiovascular settings," and that, "the presence of highly lipidic nonculprit lesions and pan-coronary plaque could, at least in theory, be used as a method to identify high-risk individuals who might be the most likely to benefit from anti-inflammatory interventions introduced at the time of infarction."
Clinical Topics: Noninvasive Imaging, Echocardiography/Ultrasound
Keywords: Ultrasonography, Interventional, Plaque, Atherosclerotic, Spectroscopy, Near-Infrared, C-Reactive Protein, Diagnostic Imaging, Inflammation, Atherosclerosis
< Back to Listings
