Increasing VA-ECMO Flow Rarely Raises PCWP in Patients With Cardiogenic Shock
Increasing venoarterial (VA) extracorporeal membrane oxygenation (ECMO) flow often has a neutral or infrequently a beneficial effect on pulmonary capillary wedge pressure (PCWP), despite raising left ventricular (LV) afterload, challenging the common assumption that high VA-ECMO flow increases PCWP and the risk of pulmonary edema in patients with cardiogenic shock, according to the PAPO-Flow single-center prospective study published Sept. 8 in JACC.
The PAPO-Flow study, conducted by Ouriel Saura, MD, et al., in Paris, France over a 10-month period in 2024, involved 80 patients with refractory cardiogenic shock (mean age, 49 years; 20% women) on femoral VA-ECMO. Patients underwent stepwise flow variations from 2 to 4 L/min in 0.5-L/min increments within the first 48 hours to determine the impact of flow variations on PCWP. Assessments included measurements from a pulmonary artery catheter, transthoracic echocardiography, and blood gas analyses to monitor hemodynamic and echocardiographic parameters.
At baseline, 34% of patients had PCWP ≥18 mm Hg. Notably, baseline PCWP was higher in individuals with LV dilation, mitral regurgitation, elevated central venous pressure (CVP) and preserved right ventricular (RV) function.
Results showed that as VA-ECMO flow was incrementally increased, PCWP decreased in 36% of patients, remained stable in 58%, and increased in only 6% of patients despite a concurrent rise in LV afterload. The authors explain that “the expected rise in PCWP caused by afterload elevation appears to be counterbalanced by a reduction in RV preload.”
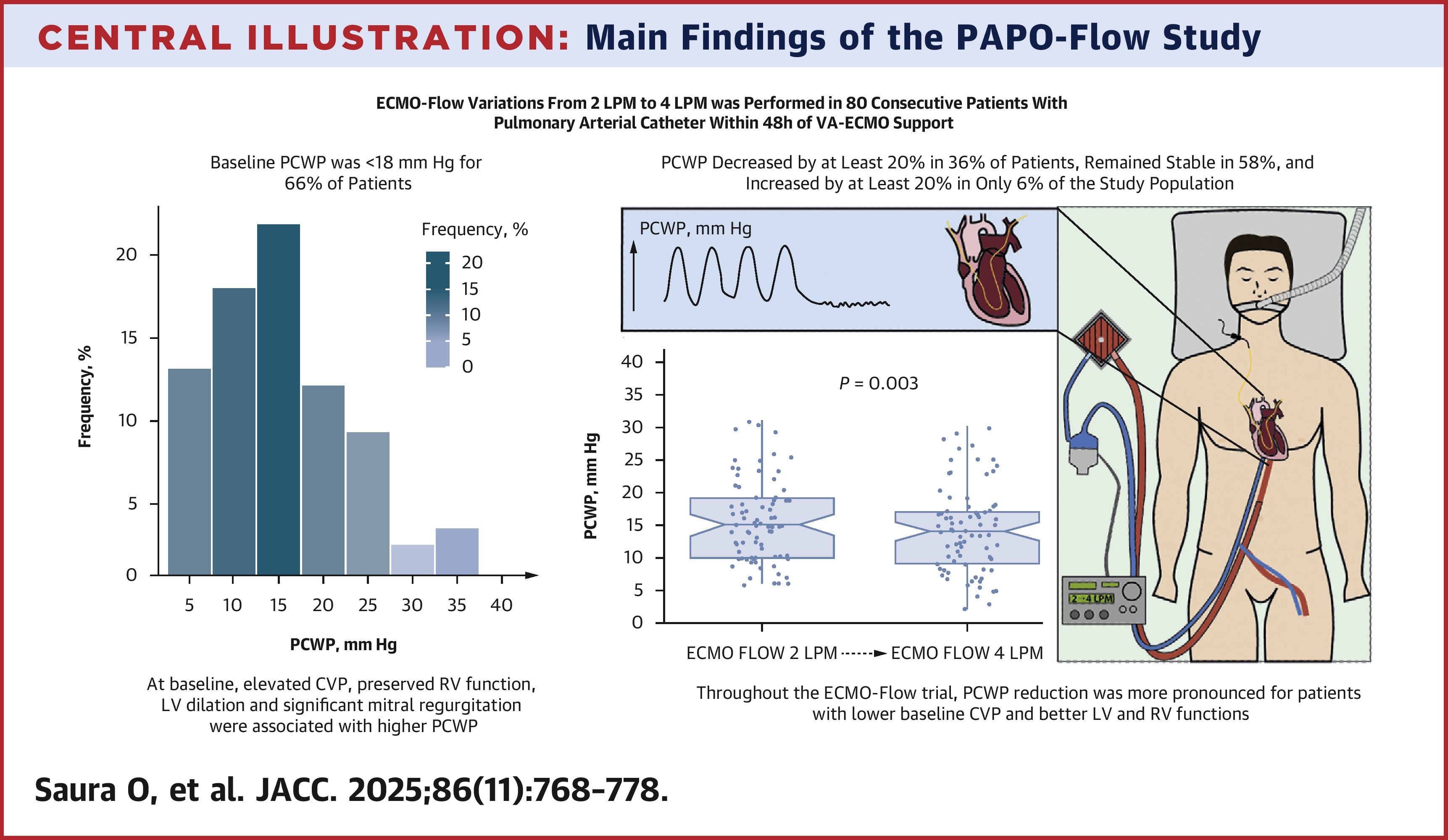
Further hemodynamic analysis revealed that CVP significantly decreased with increased flow, whereas RV afterload remained unchanged. Indexed stroke volume also decreased and myocardial work remained stable despite a rise in LV afterload. Importantly, throughout the study, a significant PCWP reduction was more commonly observed in patients who had lower baseline CVP and better LV and RV function.
In an accompanying editorial, Vanessa Blumer, MD, FACC, et al., write, “These findings suggest that the presumed linear relationship between VA-ECMO flow and LV overload may be more physiologically nuanced, and perhaps modulated by concurrent reductions in RV preload, improved RV–pulmonary arterial coupling, or decreased venous return.” They also suggest that “in selected patients, higher VA-ECMO flow may improve rather than worsen pulmonary congestion” and note that “not all patients on VA-ECMO follow the same path or will benefit from the same interventions.”
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: Shock, Cardiogenic, Pulmonary Wedge Pressure, Extracorporeal Membrane Oxygenation, Hemodynamics
< Back to Listings
