From the Member Sections | The Nursing Shortage and CV Care: A Time For Action

The national nursing shortage has been a concern since long before the COVID-19 pandemic. In fact, it has been on the radar of multiple medical and nursing societies and health care entities for at least a decade.1 The need for more nurses and an expansion of their collective clinical role in patient care is now critical to addressing the demands of an aging patient population.
The American Hospital Association in 2021 projected a shortage of 500,000 nurses by the year 2026.2 With the aging population of the workforce, the shortage may double because 1 million nurses are expected to retire by 2030. While the full impact of the pandemic on this shortage remains unknown, it has served as an accelerant to the underlying crisis. A recent survey by the American Nurses Association found that 22% of registered nurses (RNs) and 20% of nurse leaders indicated wanting to leave the profession due to COVID-19.
Factors in the Nursing Shortage
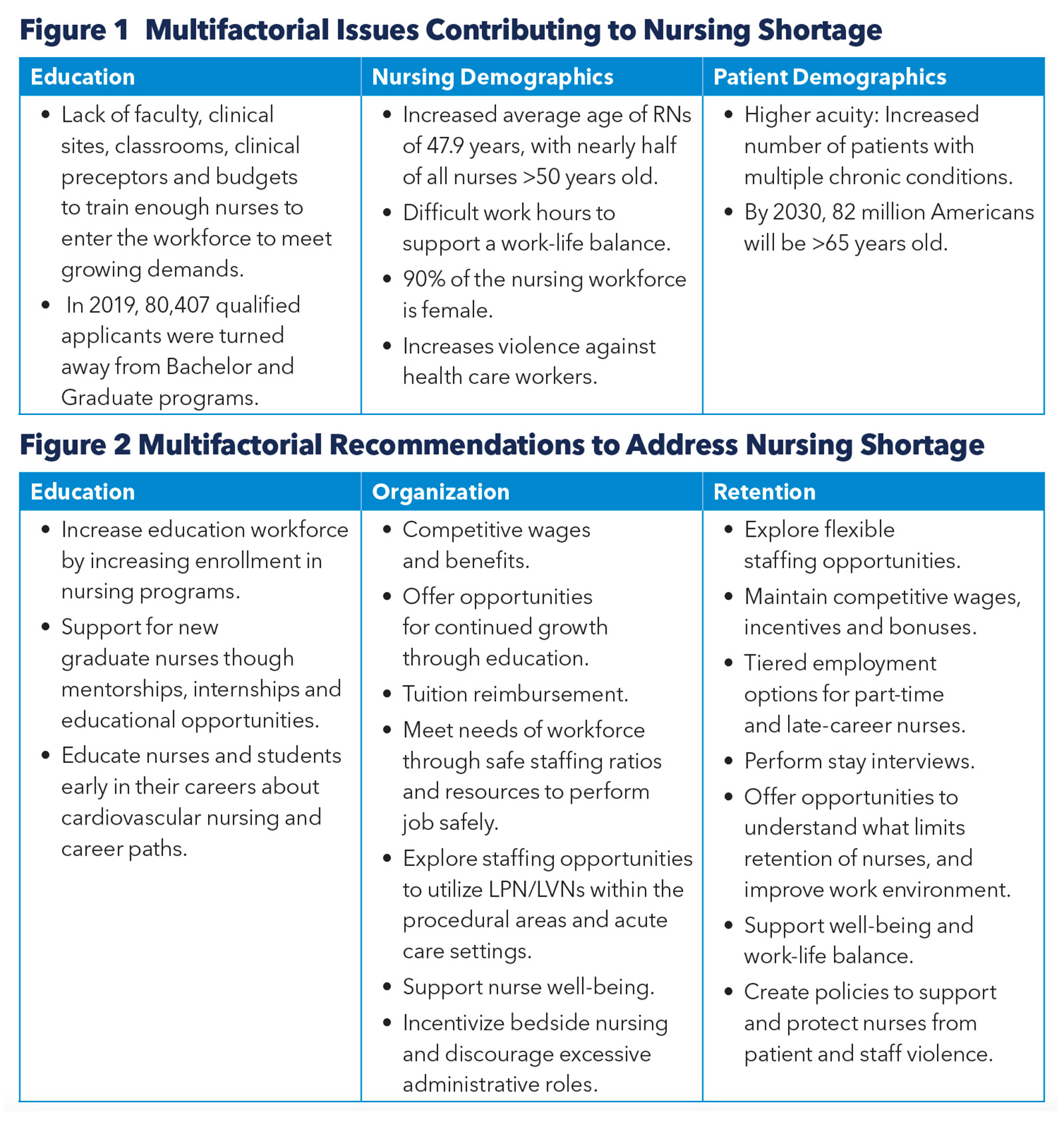
Important factors driving the nursing shortage are tightly linked to issues related to education, nursing demographics and patient demographics (Figure 1). These are multifactorial issues that are difficult to address – which is perhaps why they have been overlooked for years – and institutions are opting for simpler, short-term "solutions" instead. For example, many nurses, including those in cardiac catheterization labs, have been redeployed to different areas of the hospital, regardless of their training or experience.3 Furthermore, it has led to the cycling through of droves of travel nurses. These core issues must be understood and addressed to have a true impact on the problem.
Impact on Cardiovascular Care
Cardiovascular care and procedures have become increasingly complex over the past decade. This has increased the need and reliance on experienced and specialty trained nurses in the pre-op, intra-op, post-op, acute and critical care settings. Nurses caring for these patients require advanced knowledge as they participate in emergency response teams and are responsible for management of complex devices, such as mechanical circulatory support.
Specialized nurses in cardiovascular care are not interchangeable with nurses from other areas of the hospital. Therefore, when a staffing shortage occurs, replacing trained and experienced nurses become more challenging.
The nursing shortage has affected the cardiovascular service line in their ability to accept and care for patients. Institutions are having to divert emergency cases such as STEMIs, procedural volumes are decreasing, and cases are being delayed.
The negative impact of the pandemic continues to be felt in procedural areas, such as the cardiac catheterization lab. A national survey of cardiac catheterization lab nurses and technicians performed during the pandemic demonstrated that 66% experienced a decrease in work hours and 45% were relocated to work in different areas of the hospital.3 Moreover, there was a reported 96% decrease in overall morale with an increase in depression.
Recommendations
Connect With The CV Management Section
Click here to learn about ACC's CV Management Section and engage with your community.
Recognition of the problem is only the first step. Societies, such as the ACC, play an important role in shaping policy to bring change and intervention from a national platform.
In our local institutions, the shortage has not only had a negative impact on patients, but also on physicians and their ability to provide safe and efficient care.
There is an urgent need for aligned support from the cardiovascular team, including our physician colleagues. Physicians can provide a more powerful voice within institutions to help partner with nurses and administration and advocate for long-term solutions. When there is a fracture in the care team, all team members and their patients feel the impact.
Partnership with physician support and advocacy is integral to help administrations, health care payers and policymakers recognize nurses as key stakeholders in cardiovascular care and patient's outcomes.
Staffing Insights From ACC Survey
Significant staff departures in the last half of 2021 were reported by a third of cardiologists in a recent ACC survey. Registered nurses and cardiologists were the most likely clinical staff to leave their organizations, according to 64% and 44% of the respondents, respectively. Departures of nurse practitioners, certified nursing assistants and licensed practical/vocational nurses were reported by about a third of the cardiologists surveyed, and clinical nurse specialists by a tenth. Employees in hospitals/inpatient settings were more likely to leave than those working in clinic/outpatient settings. COVID-19-related issues, better pay or opportunity at another employer, being overworked and burnout were the most common reasons cited for the departures.
While the majority of respondents were very positive about the quality of candidates interviewed and about their training/onboarding process, more than two-thirds of organizations have provided some compensation-related or benefit-related offering to attract qualified candidates. The top three were an increased starting salary, new/increased hiring bonuses and flexible working hours. Yet, two-fifths said it would take more than a year for staffing levels to return to normal levels. One-fifth were offering new incentives or innovative work solutions to retain existing staff.

This article was authored by Bailey Ann Estes, MSN, RN-BC, RNFA, CNOR, RCIS, and Cardiac Care Associate of ACC, a cardiac registered nurse, first assistant and research coordinator at Hendrick Medical Center in Abilene, TX. She is a member of the CV Team Section. Reach out to her @baileyannRN.
References
- Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine. The Future of Nursing. Leading Change, Advancing Health. Washington (DC): National Academies Press (US); 2011.
- Gaffney T. Retaining nurses to mitigate shortages. Am Nurse 2022;Jan. 11.
- Estes BA, Varghese JJ, Jacques J, Naidu SS. Logistical, financial, and psychological impact of the COVID-19 pandemic on cardiac catheterization lab nurses and technologists: A U.S. national survey. J Invasive Cardiol 2021;33:E9-E15.
Clinical Topics: Cardiovascular Care Team, COVID-19 Hub, Geriatric Cardiology, Prevention, Stress
Keywords: ACC Publications, Cardiology Magazine, Aged, Middle Aged, Work-Life Balance, COVID-19, Pandemics, Cardiovascular Nursing, American Nurses' Association, Cardiologists, Depression, Education, Nursing, Graduate, Inpatients, Internship and Residency, Mentors, Motivation, Multiple Chronic Conditions, Nurse Clinicians, Outpatients, Workforce, Employment, Surveys and Questionnaires, Cardiac Catheterization, Nurse Practitioners, Critical Care, Demography, Patient Care, Delivery of Health Care, Hospitals, Policy, Students, Violence, Burnout, Psychological, Faculty, Salaries and Fringe Benefits, Aging
< Back to Listings