Position Statement Expands Definition of High-Risk Plaque
The definition of a high-risk plaque should be expanded beyond the traditional focus on plaque rupture and thin-cap fibroatheroma in the setting of acute coronary syndromes (ACS), according to a new JACC: Cardiovascular Imaging Position Statement published in the journal on Feb. 26.
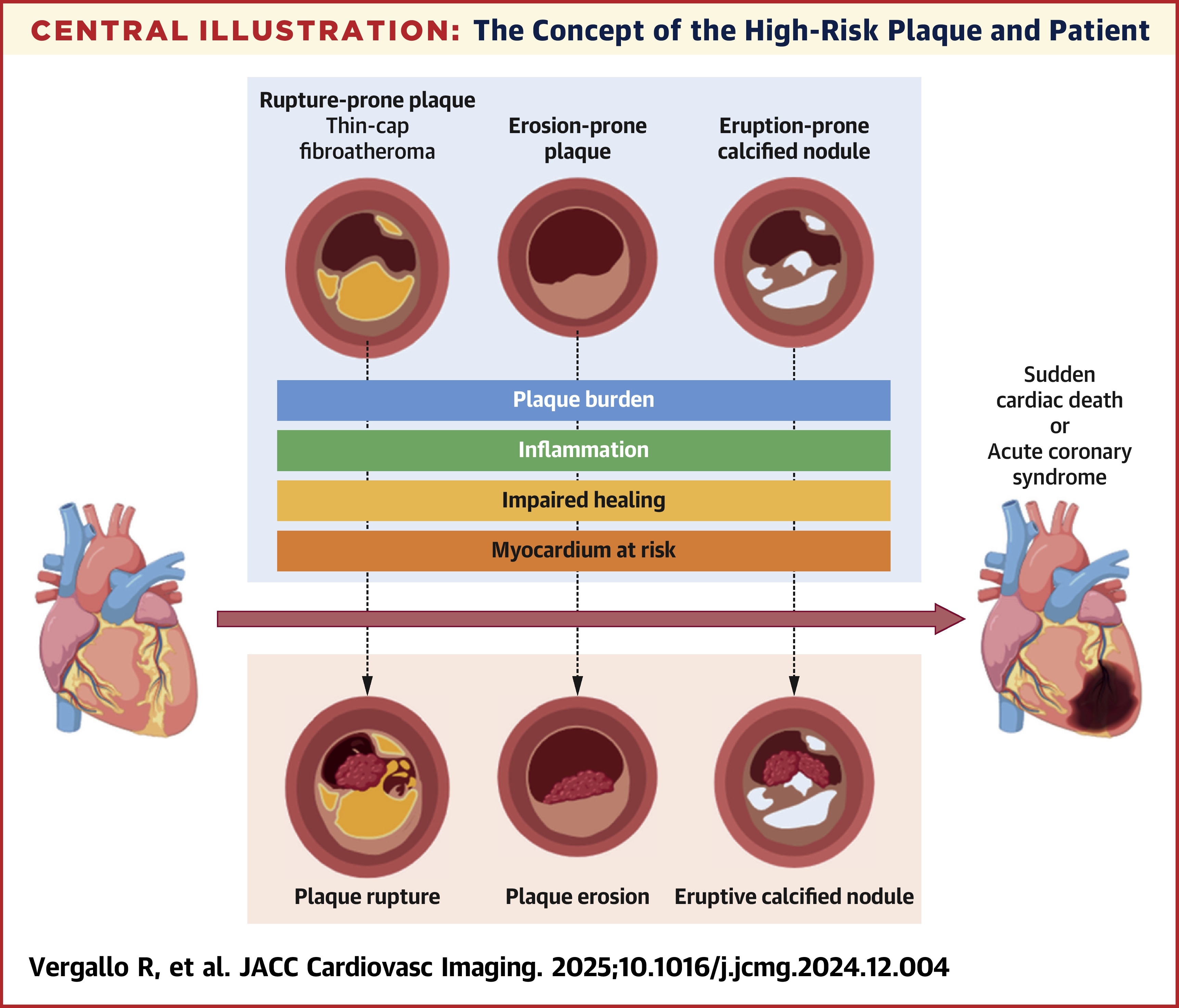
In the Statement, authors Rocco Vergallo, MD, et al., write that the concept of the high-risk plaque is affected by evolving cardiovascular risk and advances in pharmacotherapy. Thus, its definition "must broadly encompass all lesion precursors that are thrombosis prone," such as plaque rupture, plaque erosion and eruptive calcified nodules.
They note that endothelial erosion with thrombosis has become more frequent, accounting for a third of ACS cases, while plaque rupture occurs less frequently. Furthermore, calcified plaques, including eruptive calcified nodules, may be an increasing contributor to ACS.
They define high-risk as: "a plaque with increased propensity to evolve into a clinically relevant thrombosis, and to cause ACS (mostly [STEMI] or type 1 [NSTEMI]) or cardiac death on the basis of its morphology, burden, biological activity, intrinsic thrombogenicity, and location." They provide a proposed list of major and minor criteria for support defining a high-risk plaque.
Additional determining factors should include: "plaque burden, a lipid-rich core, a thin fibrous cap, inflammation, impaired protective mechanisms (prevalence of prothrombotic over antithrombotic factors), an altered local hemodynamic pattern, features of the fluid phase of blood, and the amount of myocardium at risk subtended by the lesion."
In addition to a discussion of expanded criteria and critical risk factors, the authors write that a comprehensive approach requires assessment of both morphology and activity and they discuss noninvasive and invasive imaging modalities. CT angiography is especially promising as a noninvasive approach. More invasive imaging modalities like IVUS and optical coherence tomographic imaging may hold some benefit but remain limited and potentially cumbersome to implement.
In the Statement, the authors also analyze key morphologic features, advances in pharmacologic therapies for plaque regression and stabilization, and the feasibility and efficacy of focal interventional treatments including preemptive plaque sealing.
"However," the authors write, "the safety, efficacy, and cost-effectiveness of such interventions must be demonstrated before widespread adoption."
Clinical Topics: Acute Coronary Syndromes, Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Interventions and ACS, Interventions and Imaging, Computed Tomography, Nuclear Imaging
Keywords: Computed Tomography Angiography, Plaque, Atherosclerotic, Acute Coronary Syndrome
< Back to Listings
