Partial Perforations in LBBAP May Not Carry Higher Risk of Adverse Outcomes
Partial perforations (PP) of the lead helix, a potential complication of left bundle branch area pacing (LBBAP), is not associated with a higher risk of adverse clinical outcomes, according to a new study published in JACC: Clinical Electrophysiology.
In a single-site, retrospective clinical evaluation at a Japanese hospital, study authors Hiroyuki Kato, MD, PhD, et al., identified 95 patients (mean age 77.5 years; 50.5% women) from 2019-2023 who underwent LBBAP, either left bundle branch pacing (LBBP) (60 patients) or left ventricular septal pacing (35 patients).
All patients had either bradyarrhythmias or heart failure (HF). Among them, the indication for pacing was atrioventricular block in 52, sinus node dysfunction in 26, sinus node dysfunction in 14 and atrioventricular node ablation due to atrial fibrillation with HF in three patients. The mean CHADS2 score was 2.2; mean LVEF was 54.5%.
Postoperative echocardiography performed one week post procedure revealed that a PP occurred in 25 patients, all of whom were treated with an LBBP; the incidence rate was 41.7%. Patients with a PP, vs. those without, had a lower interventricular septal thickness (8.6 mm vs. 9.6 mm) at baseline, and a significantly longer paced QRS duration (127.3 ms vs. 120.0 ms).
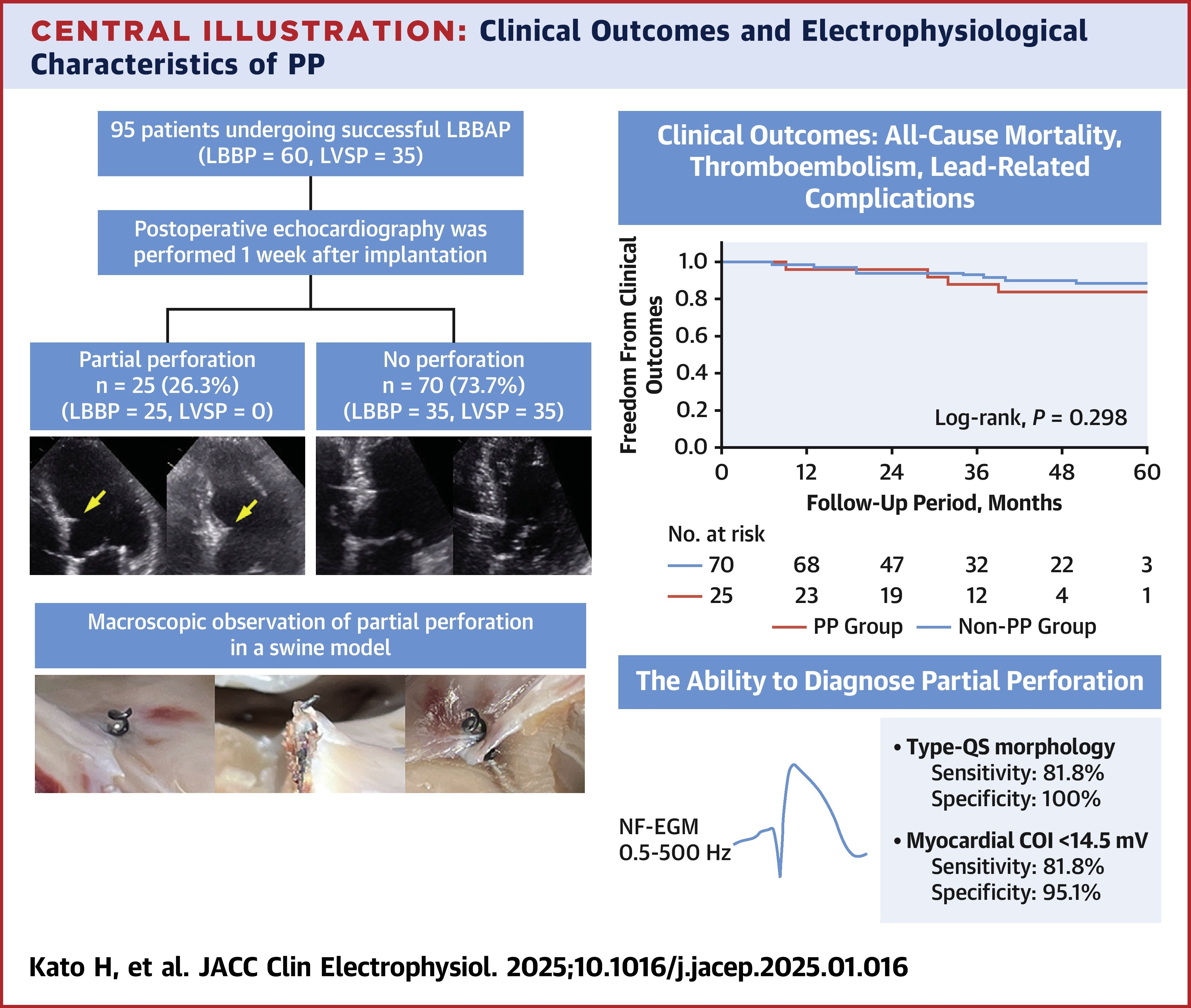
Results showed that at a median follow-up of 24 months the event-free survival rates were similar between the PP and non-PP groups for the combined clinical outcome of all-cause mortality, thromboembolism and lead-related complications. Of note, no thromboembolism or lead-related complications occurred in the PP group. The similar event-free survival persisted at five years (84.0% vs. 88.6%).
Additionally, the nonfilter unipolar electrogram (NF-EGM) showed that in the PP group the morphology was type-RS in two patients and type-QS in nine patients, and in the non-PP group it was type-R in 36 and type-RS in five patients.
An experimental study also conducted by the researchers in four swine hearts to evaluate LBBAP lead implantation had similar outcomes in terms of morphology: one heart with no PP was classified as type-R, while two with a PP and one with a complete perforation were classified type-QS. The authors write that "the type-QS and type-R morphologies of NF-EGM reliably identified and excluded PP, respectively, as validated in the swine studies."
"Although our study found that PP did not correlate with poor clinical outcomes or pacing complications, the long-term safety and impact of PP on lead extraction remain unclear," they write. Moreover, until evidence establishes PP is clinically harmless, it should be avoided. They propose determining the endpoint of deep septal lead advancement using NF-EGM morphology."
"Conduction area pacing focusing on capturing the left bundle has been rapidly adopted and we continue to learn best practices for lead placement," says ACC Clinical Content Editor-in-Chief Fred M. Kusumoto, MD, FACC. "Although there was no impact on outcomes, the authors report that partial perforation of the septum is not uncommon, and that the presence of a unipolar QS or RS morphology should alert the implanter that partial perforation may be present."
Clinical Topics: Arrhythmias and Clinical EP, Noninvasive Imaging, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Echocardiography/Ultrasound
Keywords: Echocardiography, Electrophysiology
< Back to Listings
