Focus on EP | A Paradigm Shift in the Management of Outside Hospital Cardiac Arrest

Every year more than a half million cardiac arrests occur in the U.S., and more than half of these events occur outside the hospital setting.
Management of outside hospital cardiac arrests (OHCA) is critically dependent on initiating CPR and providing external defibrillation in a timely manner. Despite numerous attempts to improve emergency response systems, including the strategic deployment of AEDs in public places, OHCA outcomes have remained dismal with survival to hospital discharge rates of 10-12%.1
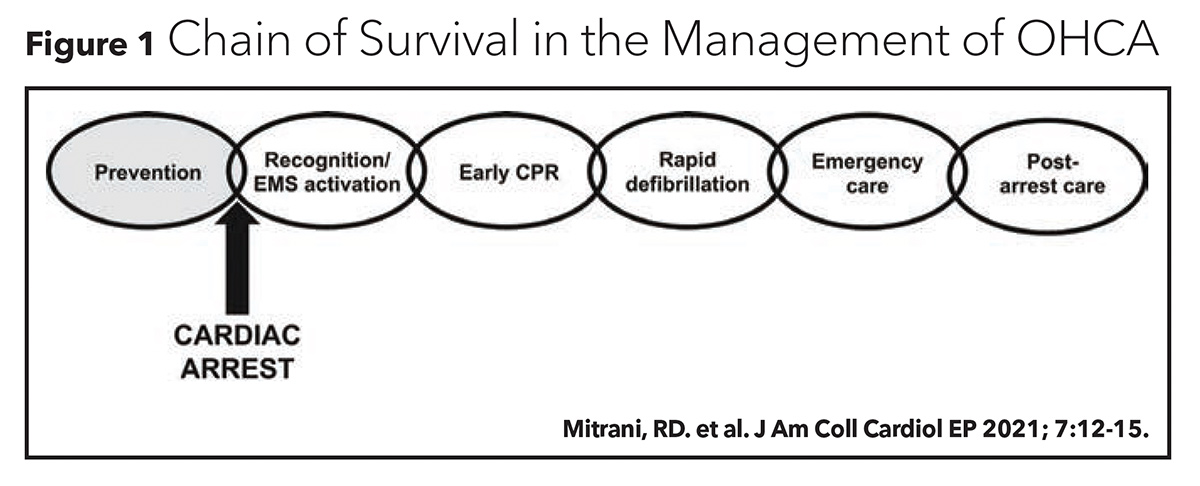
More recent efforts to optimize the chain of survival in OHCA have focused on engaging community activists who are able to provide basic life support in a more timely manner until emergency medical services (EMS) are available (Figure 1). During the COVID-19 pandemic, however, the stay-at-home mandates, calls for social distancing and public fear of disease transmission may have dissuaded community responders from assisting in OHCA.
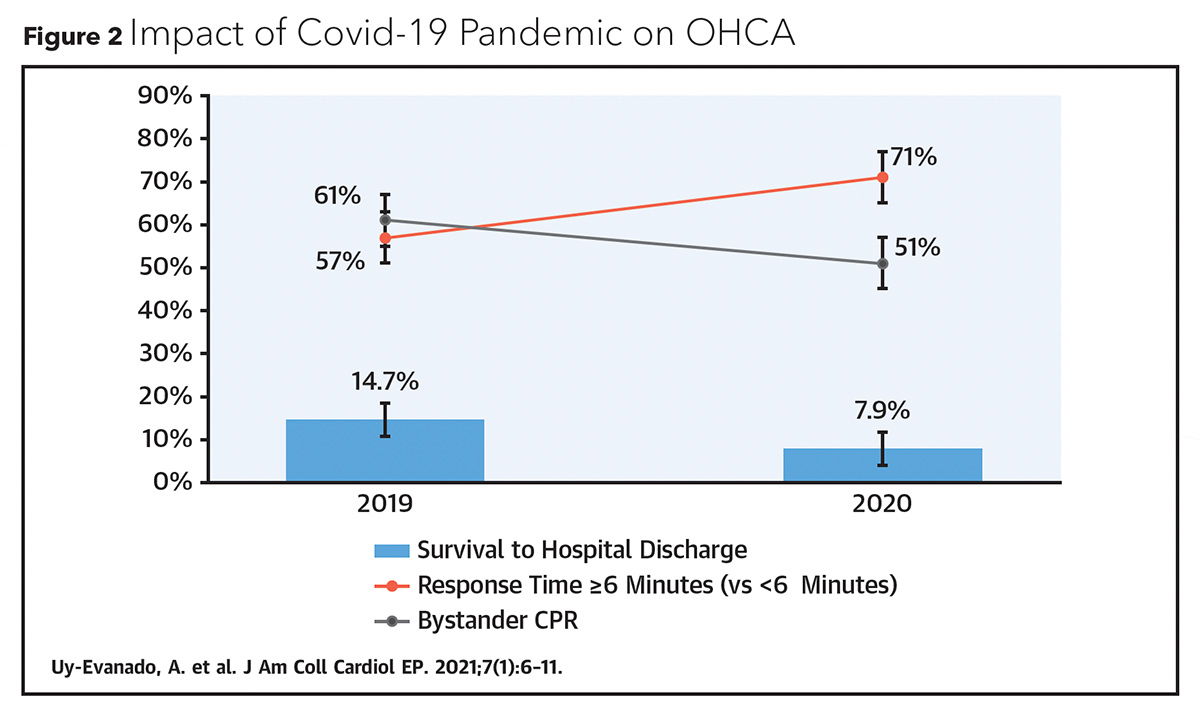
An investigation of OHCA outcomes during the COVID-19 pandemic confirmed this suspicion and revealed its detrimental impact on OHCA survival rates. Uy-Evanado, et al., compared consecutive cases of prepandemic OHCA cases (March to May 2019) with consecutive canvases of pandemic OHCA cases (March to May 2020) in two communities from Oregon and California.2 From the prepandemic to the pandemic period, the number of OHCA cases increased by nearly 25% (Figure 2). Compared to the prepandemic period, during the pandemic period there was a significant increase in the proportion of OHCA cases occurring in the home (76% vs. 73%; p=0.009), a significant increase in EMS response time (7.6 mins vs. 6.6 min; p<0.001) and a significant decrease in the proportion of OHCA cases involving bystander CPR (51% vs. 61%; p=0.002) and bystander use of AEDs (1% vs. 5%; p=0.002). Overall, OHCA survival to hospital discharge during the pandemic period was nearly 50% lower than during the prepandemic period (7.9% vs. 14.7%; p=0.02).
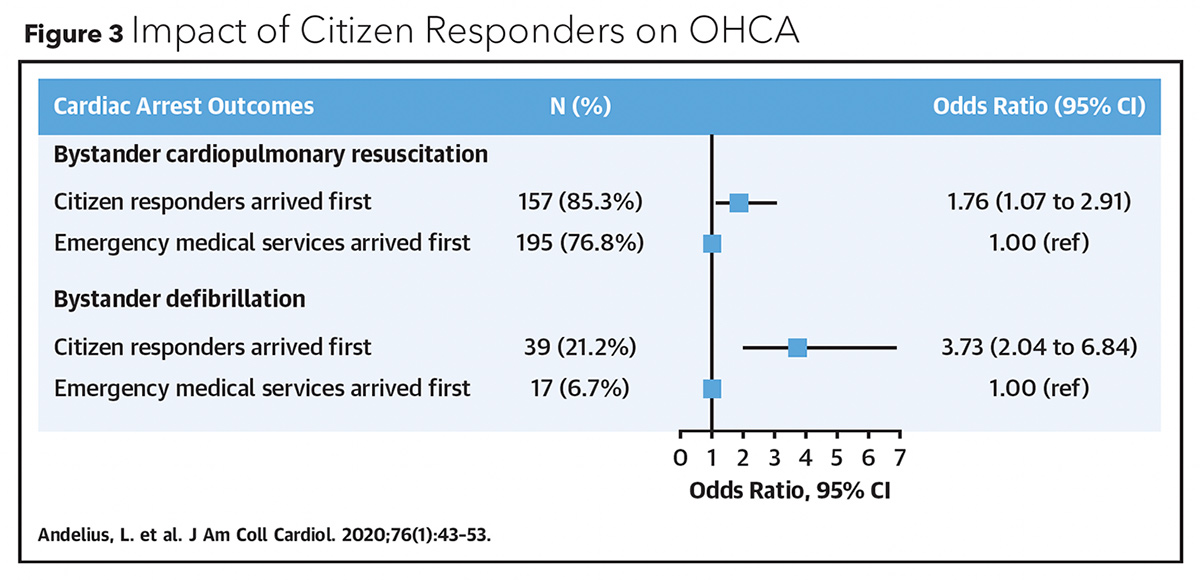
More recent efforts to improve survival rates in OHCA have focused on utilizing technology to facilitate response times. Andelius, et al., evaluated the use of a smartphone-based activation of community responders in OHCA cases and its impact on bystander CPR and AED use in the capital region of Denmark from 2017-2018.3 Community responders were adult volunteers who were not required to have CPR and/or AED training. However, nearly 99% of volunteers had received CPR training and 26% were health care professionals. At the time of a suspected OHCA, a centralized emergency dispatch system would reach out to nearby community responders and coordinate efforts to localize the OHCA location, start CPR, and/or retrieve a nearby AED. After the event had resolved, responders were surveyed on whether physical injury or psychological distress was experienced.
Of the 6,836 responders who were alerted in 438 OHCA cases, 51% (n=3,480) responded to the alarm, and 47% (n=1,623) accepted the alarm. In 8% of OHCA cases no responders accepted the alarm. In 42% of OHCA cases, community responders arrived before EMS and this was associated with a significantly higher percentage of bystander CPR (85.3% vs. 76.8%; p=0.027) and AED use (21.2% vs. 6.7%; p<0.001). The longer it took for EMS to arrive at an OHCA, the more likely it was for a community responder to be the first to arrive: community responders arrived before EMS in 23.3% of cases when EMS response time was <5 minutes and in 71.2% of cases when EMS response was >10 minutes (Figure 3). There was a trend towards improved 30-day survival in OHCA cases when citizen responders arrived before EMS (16.1% vs. 13.1%; p=0.38).
What a fantastic repurposing of an old red phone box 🤩 pic.twitter.com/y81r8YwjVA
— Sarah-Jane Marsh 💙 (@BWCHBoss) September 4, 2021
A separate study by Schiebeck, et al., assessed the feasibility of using drones (unmanned aerial vehicles) to deliver AEDs to locations of suspected OHCA to assist standard EMS response in a semi-urban region of Sweden in 2020.4 Drones were available for dispatch between 8 a.m. and 10 p.m. (during regulated air space time) but their use was limited by inclement weather (darkness, rain and wind ≥8 m/s) and geographic constraints (no-fly zones, buildings ≥5 stories, and outside of administrative range).
Of the 53 alerts of suspected OHCA during the study period, 74% were prohibitive for drone use. In the 14 cases eligible for drone use, a drone was dispatched in 12 cases (86%) and successfully delivered an AED in 11 cases (92%). The median distance traveled by the drone (hanger to suspected OHCA location) was 1.9 miles and there was 100% accuracy in delivering the AED within 10 feet of the expected drop off point. In seven of these cases (64%), the drone arrived prior to EMS with a median time benefit of 1:52 minutes. Of note, the delivered AED was not attached to the patient until EMS arrived.
While the results from these two studies are promising, it is unclear whether similar positive outcomes could be expected from the use of these technologies in less urban areas, where smartphone and drone utilization may be less prevalent. It is also unknown whether communities will embrace having untrained bystanders or unmanned vehicles involved in emergency care. Furthermore, additional concerns related to patient privacy and data security will need to be addressed before these consumer technologies can be adopted in the health care setting. Nonetheless, these proof-of-concept studies highlight exciting innovations that may improve survival in OHCA.
As the COVID-19 pandemic continues to strain the availability of medical resources and health care providers, community responders will be increasingly relied upon to expedite resuscitation efforts in OHCA. Effective incorporation of bystanders into the chain of survival for OHCA, however, will require significant updates to the current emergency response system. At the very least, community responders should be provided appropriate personal protective equipment and testing for COVID-19 to reduce infection transmission concerns. Perhaps community responders for medical emergencies should also be offered incentives for their availability, similar with airplane passengers who are assigned larger exit row seats to assist with potential flight emergencies. Whatever the solution to this dilemma may be, it will undoubtedly utilize novel technologies to educate, engage and empower community responders to play a greater role in the management of OHCA.

This article was authored by Edward Chu, MD, (@Ed_Chu_MD), an electrophysiology attending physician in Miami. He just completed his fellowship training at Mount Sinai Medical Center in New York.
References
- Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: A review. JAMA 2019;321:1200-10.
- Uy-Evanado A, Chugh HS, Sargsyan A, et al. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC Clin Electrophysiol 2021;7:6-11.
- Andelius L, Malta Hansen C, Lippert FK, et al. Smartphone activation of citizen responders to facilitate defibrillation in out-of-hospital cardiac arrest. J Am Coll Cardiol 2020;76:43-53.
- Schierbeck S, Hollenberg J, Nord A, et al. Automated external defibrillators delivered by drones to patients with suspected out-of-hospital cardiac arrest. Eur Heart J 2021;Aug 26:[Epub ahead of print].
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, COVID-19 Hub, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias
Keywords: ACC Publications, Cardiology Magazine, Smartphone, Reaction Time, COVID-19, Motivation, Emergencies, Patient Discharge, Survival Rate, Personal Protective Equipment, Wind, Oregon, Fellowships and Scholarships, Population Density, Pandemics, Darkness, Sweden, New York, COVID-19 Testing, Feasibility Studies, Physical Distancing, Privacy, Social Media, Emergency Medical Services, Heart Arrest, Hospitals, Cardiopulmonary Resuscitation, Communication, Computer Security, Health Personnel, Volunteers, Delivery of Health Care, Technology, Fear, Rain, Psychological Distress, Electrophysiology, Physicians, Reference Standards, Denmark
< Back to Listings