Feature | Patient-Centered Recommendations Focus of New HF Guideline

Patient-centric recommendations" to help clinicians prevent, diagnose and treat heart failure (HF) are the focus of a new clinical guideline recently released by the ACC, American Heart Association (AHA), and Heart Failure Society of America (HFSA). The guideline was simultaneously published in JACC.
The joint 2022 Guideline for the Management of HF includes a focus on HF prevention, with revised definitions of Stage A and Stage B HF intended to identify risk factors early (Stage A) and provide treatment before structural changes or signs of decreased HF occur (Stage B).
"One primary goal with the new guideline was to use recently published data to update our recommendations for the evaluation and management of heart failure," said Paul A. Heidenreich, MD, MS, FACC, guideline writing committee chair. "One focus was prevention of heart failure through optimizing blood pressure control and adherence to a healthy lifestyle."
While Stage A recommendations for at-risk patients are also applicable for those individuals who have progressed to Stage B and have "pre-HF" symptoms, additional medications to prevent symptomatic HF are recommended. Specifically, ACE inhibitors (ACEi) are suggested for patients with left ventricular ejection fraction (LVEF) ≤40%, while angiotensin receptor blockers (ARBs) may be prescribed for individuals with an intolerance or contraindication to ACEi. Cholesterol-lowering statins are recommended for people with a history of a myocardial infarction or acute coronary syndrome.
The use of multidisciplinary teams to facilitate guideline-directed medical therapy and self-care support for learning to manage symptoms are recommended in managing individuals who have progressed to Stage C and have HF symptoms. Screenings to identify potential medical or social barriers for effective self-care are also encouraged, as well as education and support to reduce rehospitalization and improve survival. Individuals with Stage C should also be fully vaccinated against respiratory illnesses including COVID-19.
For individuals with Stage C, the new guideline also refines the current four classifications of HF based on LVEF with new terminology.
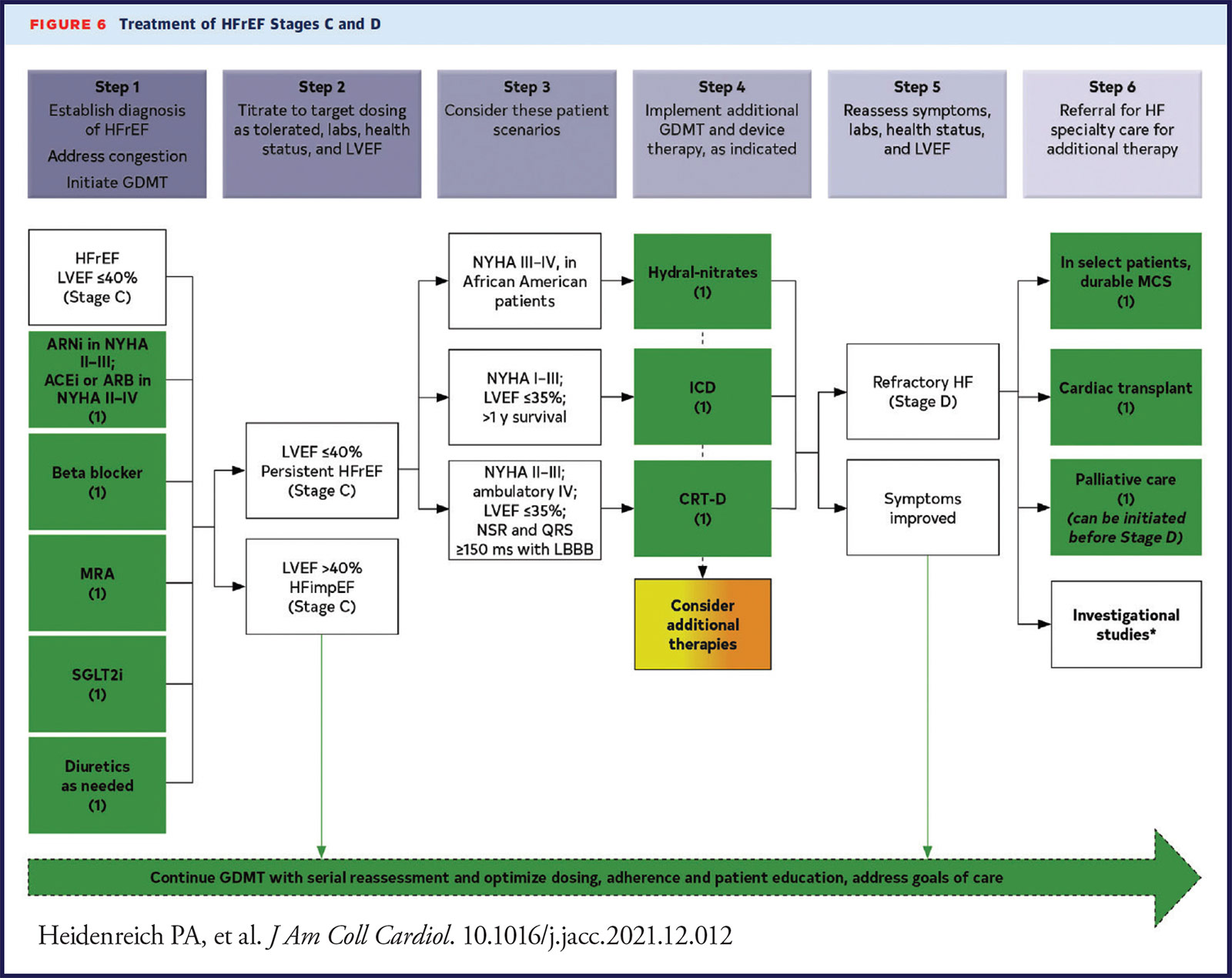
Drug Therapy for HF
Pharmacological treatment for managing patients across the four classifications of HF are addressed. Recommended treatment for those with HFrEF includes four classes of medications, in addition to diuretics. Use of angiotensin receptor-neprilysin inhibitors (ARNis) is recommended, and if not feasible, the use of ACEi is recommended. ARBs are recommended for individuals with an intolerance or potential adverse reaction to ACEi medicines. Mineralocorticoid receptor antagonists (MRA) or beta-blockers are also recommended as in the prior guideline. SGLT2 inhibitors (SGLT2i) are now recommended for people with symptomatic chronic HFrEF regardless of the presence or absence of type 2 diabetes.
"After careful evaluation of new evidence, guideline-directed medical therapy now includes four medication classes that include SGLT2 inhibitors. Irrespective of diabetes status, the DAPA-HF and EMPEROR trials have shown the benefit of treating patients with HFrEF with SGLT2 inhibitors, showing a 30% reduction in heart failure rehospitalization. This is a major step forward in reducing mortality rates in this vulnerable population," said Biykem Bozkurt, MD, PhD, FACC, guideline writing committee vice-chair and incoming editor-in-chief of JACC: Heart Failure.
Individuals with HFmrEF should be treated first with an SGLT2i along with diuretics as needed, according to the guideline authors. ARNi, ACEi, ARB, MRA and beta-blockers are considered weaker recommendations in this population, as the evidence in this population is less robust. As LVEF may change over time, people with HFmrEF should have repeat evaluations of LVEF.
People with HFpEF and hypertension should aim for blood pressure targets in accordance with clinical guidelines. For people with HFpEF, the guideline suggests that SGLT2i may be beneficial in decreasing HF hospitalizations and cardiovascular mortality. Management of atrial fibrillation can also improve symptoms. In select individuals with HFpEF, MRAs, ARBs and ARNi may be considered, particularly among people with LVEF on the lower end of the spectrum of HFpEF.
ICDs, CRT, Amyloidois, More
The guideline also includes recommendations for ICDs, CRT and diagnosis and treatment of cardiac amyloidosis. For those with amyloid heart disease, new recommendations for treatment including screening for serum and urine monoclonal light chains, bone scintigraphy, genetic sequencing, tetramer stabilizer therapy and anticoagulation.
Specialty referrals for individuals with Stage D advanced HF, recommendations for management of atrial fibrillation and valvular heart disease in patients with HF are also included in the guideline. Other topics, including pregnancy and cardio-oncology are also a focus. In keeping with recent guidelines, value statements were created for select recommendations where high-quality, cost-effectiveness studies of the intervention have been published.
This new guideline replaces the 2013 ACCF/AHA Guideline for the Management of Heart Failure and the 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure.
Key Perspectives: 2022 AHA/ACC/HFSA Heart Failure Guideline
- Heart failure (HF) encompasses a broad range of left ventricular (LV) function. New treatment guidelines address the entire spectrum of HF. All patients with current or prior HF, irrespective of EF, should be considered for guideline-directed medical therapy (GDMT). The classification of HF based on ejection fraction (EF) is as follows:
- HF with reduced ejection fraction (HFrEF): LVEF ≤40%.
- HF with improved ejection fraction (HFimpEF): previous LVEF ≤40% and a follow-up measurement of LVEF >40%.
- HF with mildly reduced ejection fraction (HFmrEF): LVEF 41-49% and evidence of increased LV filling pressures.
- HF with preserved ejection fraction (HFpEF): LVEF ≥50% and evidence of increased LV filling pressures.
- GDMT has expanded to include four classes: 1) renin-angiotensin system inhibition (RASi) with an angiotensin receptor-neprilysin inhibitor (ARNi), angiotensin-converting enzyme inhibitor (ACEi) or angiotensin (II) receptor blocker (ARB) alone; 2) beta-blockers; 3) mineralocorticoid receptor antagonist (MRA); and 4) sodium-glucose cotransporter-2 inhibitor (SGLT2i). An ARNi is now recommended as first-line RASi to reduce morbidity and mortality in HFrEF (Class of Recommendation [COR] 1a). An ACEi is recommended when an ARNi is not feasible, and an ARB in those who are ACEi intolerant and when ARNi is not feasible. In symptomatic patients with HFrEF who tolerate ACEi or ARB, replacement with ARNi is recommended for further reduction in morbidity and mortality.
- New recommendations were made for the use of SGLT2is in HF. In symptomatic patients with chronic HFrEF, an SGLT2i is recommended to reduce hospitalization and cardiovascular mortality, regardless of the presence of type 2 diabetes (COR 1a). SGLT2is can also be beneficial in patients with HFmrEF and HFpEF (COR 2a).
- While there is little data to guide management of patients with HFimpEF, a small, randomized trial (TRED-HF) demonstrated a high rate of relapse of dilated cardiomyopathy (44%) within six months of discontinuation of GDMT. Therefore, it is recommended that GDMT be continued in patients with HFimpEF, including those who are asymptomatic, to prevent relapse of HF and LV dysfunction.
- High-value therapies (<$60,000/quality-adjusted life year gained) include ARNis, ACEis, ARBs, beta-blockers, MRAs, and hydralazine and isosorbide dinitrate in African Americans, along with ICDs and CRT, while SGLT2i and cardiac transplantation are of intermediate value. Tafamadis for amyloid was identified as low value (>$180,000/quality-adjusted life year gained), while mechanical circulatory support and pulmonary pressure monitoring are of uncertain value.
- Patients with suspected amyloid should undergo screening for monoclonal light chains, and if negative, bone scintigraphy should be performed to confirm the presence of transthyretin amyloid. Genetic testing is recommended in patients with transthyretin amyloid to differentiate hereditary variant from wild type. Tafamadis is recommended in select patients with wild-type or variant transthyretin amyloid to reduce cardiovascular morbidity and mortality (COR 1a). Anticoagulation is reasonable in patients with cardiac amyloid and atrial fibrillation to reduce the risk of stroke (COR 2a).
- Signs and symptoms of HF can be nonspecific. Therefore, supporting evidence of increased filling pressures, either invasive (hemodynamics) or noninvasive (diastolic function on imaging, natriuretic peptide) are required for confirmation of diagnosis when the EF is >40%.
- Timely referral for HF specialty care is recommended for advanced HF patients (if in accordance with goals of care) to review HF management and to assess suitability for advanced HF therapies.
- HF is a progressive disease, as highlighted by the ACC/AHA Stages of HF A-D. New terminology incorporates the designations "at-risk" and "pre-HF." Primary prevention of HF, through lifestyle modification, screening and management of risk factors and comorbid conditions, is recommended for those at risk (Stage A) or pre-HF (Stage B).
- Management of comorbid conditions in patients with HF may be beneficial. The new guideline provides recommendations for select patients with HF and anemia, iron deficiency, hypertension, sleep disorders, type 2 diabetes, atrial fibrillation, coronary artery disease and malignancy.

Authored by Monica M. Colvin, MD.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, COVID-19 Hub, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Valvular Heart Disease, Atherosclerotic Disease (CAD/PAD), ACS and Cardiac Biomarkers, Anticoagulation Management and ACS, Anticoagulation Management and Atrial Fibrillation, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Heart Transplant, Interventions and ACS, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Structural Heart Disease, Nuclear Imaging, Hypertension
Keywords: ACC Publications, Cardiology Magazine, ACC22, ACC Annual Scientific Session, Acute Coronary Syndrome, African Americans, American Heart Association, Amyloidosis, Anemia, Angiotensin Receptor Antagonists, Angiotensin-Converting Enzyme Inhibitors, Anticoagulants, Atrial Fibrillation, Blood Pressure, Cardiology, Cardiomyopathy, Dilated, Cholesterol, Contraindications, Coronary Artery Disease, Cost-Benefit Analysis, COVID-19, Data Visualization, Data Visualization, Diabetes Mellitus, Type 2, Follow-Up Studies, Genetic Testing, Glucose, Goals, Healthy Lifestyle, Heart Failure, Heart Transplantation, Heart Valve Diseases, Hospitalization, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Hypertension, Isosorbide Dinitrate, Life Style, Mineralocorticoid Receptor Antagonists, Morbidity, Myocardial Infarction, Natriuretic Peptides, Neoplasms, Neprilysin, Patient Care Planning, Patient Care Team, Patient-Centered Care, Prealbumin, Pregnancy, Primary Prevention, Quality-Adjusted Life Years, Radionuclide Imaging, Receptors, Angiotensin, Recurrence, Referral and Consultation, Renin-Angiotensin System, Risk Factors, Self Care, Sleep Wake Disorders, Social Media, Sodium, Sodium-Glucose Transporter 2 Inhibitors, Stroke, Stroke Volume, Ventricular Function, Left, Ventricular Function, Left, Vulnerable Populations, Writing
< Back to Listings