Spotlight Series | Microvascular Dysfunction Treatment Options For Coronary Microvascular Dysfunction
Coronary microvascular dysfunction (CMD) has been associated with a wide spectrum of conditions and diseases.1 Importantly, it has proven to be a strong prognostic marker of morbidity and mortality. Despite these findings and increased attention, guideline-based treatment recommendations directed at CMD are lacking.
CMD may cause transient myocardial ischemia, in the absence of macrovascular coronary artery disease (CAD) or with obstructive macrovascular disease. Because current diagnostic approaches make evaluation challenging when upstream epicardial obstructive disease is present, most useful evaluations have focused on selected patient cohorts without epicardial obstructive disease.
Coronary Microvascular Dysfunction
The coronary microvasculature constitutes most of the myocardial vascular bed and therefore conditions affecting the microvasculature are also likely to influence cardiac mechanical function.
CMD is believed to mostly affect the coronary arterioles, although more distal involvement (capillaries, venules, pericytes, membrane, etc.) is possible. It was first suggested in 1967 as a cause for angina and ischemia without obstructive CAD2 and securely linked to the coronary microvasculature in the 1980s3 when functional testing was performed.
Yet more than four decades later, very few labs (<5%) perform any functional testing during invasive coronary angiography. The barriers to this important testing are numerous and include lack of proven therapies to alter outcomes. However, these barriers will have to be addressed if the field of CMD is to move forward. It is remarkable, given its very high prevalence, that pathologic and treatment information on CMD is so scarce.

CMD is prevalent in hypertension, cardiomyopathies (hypertrophic, ischemic and nonischemic), diabetes, metabolic syndrome, chronic kidney disease, cancer chemotherapy and several other conditions. It is increasingly recognized as an important contributor to myocardial ischemia, in the presence and absence of epicardial coronary atherosclerosis, that is either obstructive or nonobstructive.
The latter, termed ischemia and no obstructive coronary arteries (INOCA), has a high prevalence that occurs mostly in middle-aged women; however, effective treatment remains elusive.4
Multiple studies have confirmed findings from the WISE study that INOCA and CMD are associated with impaired prognosis.5-8 Thus, an effective treatment strategy would be anticipated to beneficially impact this impaired prognosis.
Although to date there are no experimental models for INOCA, animal models of CMD, a hallmark of INOCA, provide a pathway to enhance our understanding of CMD pathophysiology and provide direction for novel therapies.9
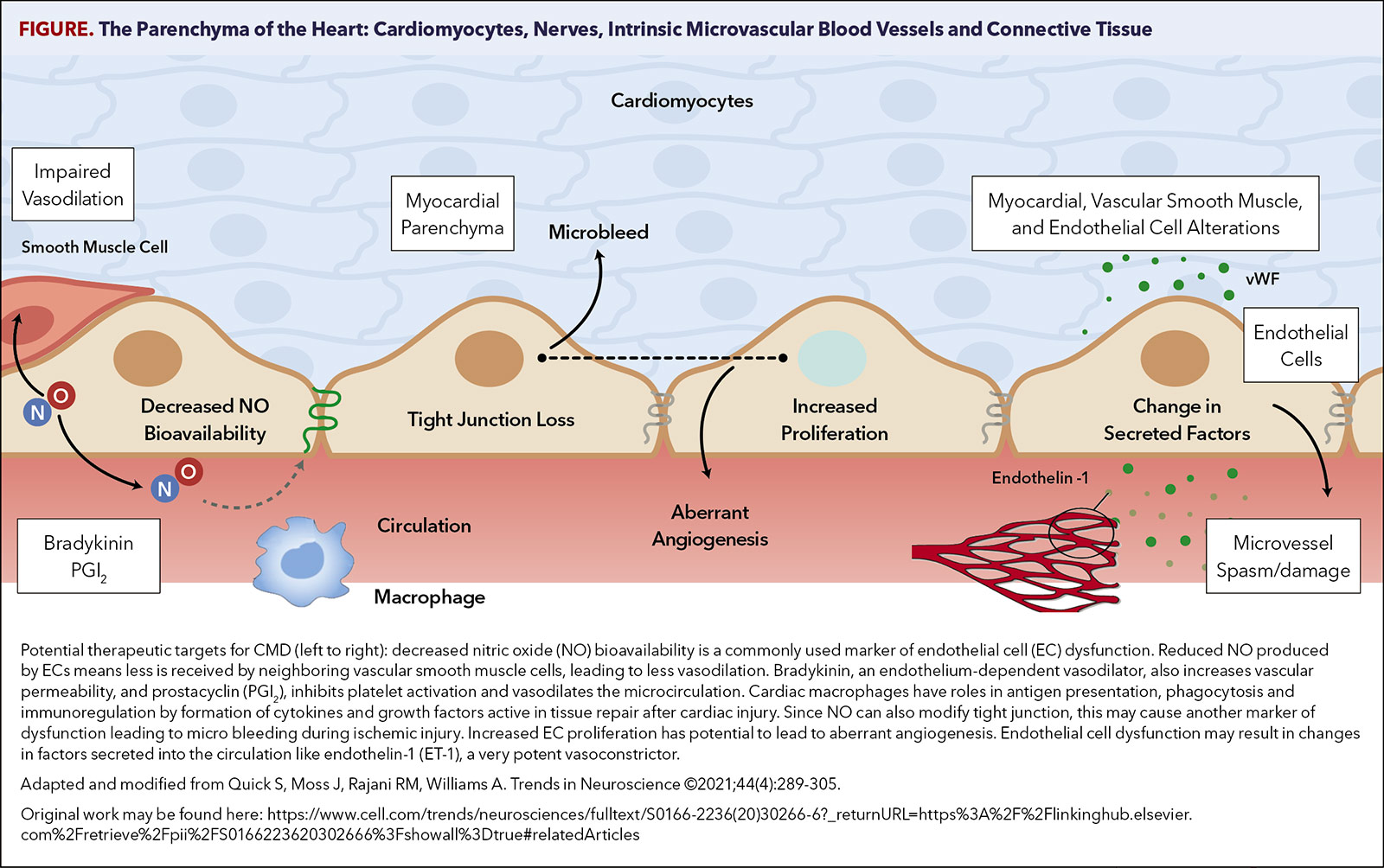
These experimental studies also provide insights into the genetic and environmental basis of human CMD. Suggestions are included for functional, structural, endothelium-dependent, neurohumoral, vascular smooth muscle cell, arteriolar capillary density, nitric oxide, reactive oxygen species, endothelin (ET-1), prostaglandin, renin angiotensin aldosterone system (RAAS), sympathetic nervous system, and media alterations in CMD (Figure).
Because of limitations in the techniques to study CMD in intact patients, most treatment studies have focused on patients without upstream obstructive CAD. As INOCA is much more prevalent among women (by approximately threefold), sex-related differences are critically important.
The detailed findings of an extensive review conducted by Bairey Merz, Pepine, et al., has been published elsewhere.10 This comprehensive review of treatment studies confirmed that all studies have been small in sample size, with heterogeneous methodology, and few were double-blinded and/or placebo-controlled.
The studies used many different treatments, outcomes and definitions for CMD. The small sample sizes severely limit the power of these studies for impact on major adverse cardiovascular events, with the majority enrolling fewer than 20 patients.
Studies evaluating sildenafil, quinapril, estrogen and transcutaneous electrical nerve stimulation application demonstrated benefits in their respective endpoints. Very limited to no benefit was observed with L-arginine, doxazosin, pravastatin and diltiazem.
Our systematic review highlights that there are few data to support consensus documents or clinical practice guideline-recommended therapies for CMD. Some pertinent highlights are summarized here that we believe may be useful for future large, randomized, controlled trials.
Table. Potential Therapies For CMD
(an incomplete list):
Potential Clues to Mechanisms
Pharmacologic
Nonpharmacologic
Some of these treatments are listed in the Table. Briefly, statins, ACE inhibitors and ARBs have shown considerable promise.11-13 These smaller trials are supported by several recent very large registries reporting that patients with nonobstructive CAD receiving statins have significantly better outcomes compared with those who were not receiving statins.14,15
Drugs influencing the RAAS (ACE inhibitors or ARBs) have a strong rationale and have shown promise.16 But adding aldosterone blockade to an ACE inhibitor or ARB did not result in additional improvement.17 Late sodium channel blockade and estrogens also have some compelling data.18-20
Additionally, many nonpharmacologic studies have suggested promise. Most attractive are those using exercise.21 Two separate, very recent phase-1 "proof-of-concept" studies using autologous, granulocyte colony stimulating factor-mobilized CD34+ cells injected directly into the left coronary artery have published encouraging findings.22,23
Several larger, well-controlled trials are underway that will provide important new data on management for patients with INOCA. The British Heart Foundation-sponsored CorCTCA trial (NCT03477890) is ongoing.24 It will help to clarify the prevalence and clinical significance of INOCA when care is based on coronary CTA.
To date, there are no disease-modifying therapies specific to INOCA, but two ongoing trials will provide important new data in this regard. The PRecIsion Medicine With ZibotEntan in Microvascular Angina (PRIZE) trial holds promise (NCT04097314).25,26
Small Vessel Impact on Angina, Ischemia
The diagnosis of CAD has focused on presence of obstructive epicardial CAD. It is estimated that at least two of five male and female patients with angina referred for elective coronary angiography have nonobstructive epicardial coronary arteries, with rates relatively higher in women. Missed the first three articles in this four-part series, developed by invited Guest Editor, C. Noel Bairey Merz, MD, FACC? Click here to read them now.
The rationale for this trial is that INOCA is associated with dysregulation of the endothelin system. So, the recruited INOCA cohort is enriched by prospectively genotyping candidates for the minor G allele of the noncoding single nucleotide polymorphism rs9349379 that enhances expression of the ET-1 gene in human vascular cells, increasing circulating concentrations of ET-1.
The prevalence of this allele is higher in patients with ischemic heart disease. These patients are then randomized to receive either zibotentan, an endothelin A-receptor antagonist, or placebo using a double-blind, crossover design. The planned sample size is 356 patients. This agent may provide benefit by opposing the increased vasoconstrictor response of coronary microvessels to endothelin.26
The Women's IschemiA Trial to Reduce Events in Non-ObstRuctIve CORonary Artery Disease (WARRIOR; NCT03417388), sponsored by the Department of Defense, is currently enrolling.27
WARRIOR is a multicenter, PROBE design study evaluating the effects of intensive medical treatment with a potent statin, high-dose ACE inhibitor or ARB, and aspirin compared with usual care on major adverse cardiac events, angina and quality of life in symptomatic women with INOCA. Currently, 2,200 women have been randomized and the planned median follow-up is approximately three years.
Looking Ahead
Although some treatments have been associated with promising results, no specific treatment has been sufficiently well documented to be recommended in any patient group or subgroup with CMD. Clearly, there is a key unmet need for larger, well-designed, clinical trials addressing adverse outcomes prevention in this population.
It is strongly suggested that future studies stratify study populations according to pathogenic mechanisms and covariates. This approach should best permit investigating whether the specific individualized treatment approach would be more successful.
This article was authored by Carl J. Pepine, MD, MACC, professor, Division of Cardiovascular Medicine, University of Florida, Gainesville, FL.
References
- Prakash RO, Chakrala TS, Feuer DS, Valdes CA, Pepine CJ, Keeley EC. Critical role of the coronary microvasculature in heart disease: from pathologic driving force to "innocent" bystander. Am Heart J Plus 2022;22:100215.
- Likoff W, Segal BL, Kasparian H. Paradox of normal selective coronary arteriograms in patients considered to have unmistakable coronary heart disease. N Engl J Med 1967;276:1063-66.
- Cannon RO 3rd, Watson RM, Rosing DR, Epstein SE. Angina caused by reduced vasodilator reserve of the small coronary arteries. J Am Coll Cardiol 1983;1:1359-73.
- Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and no obstructive coronary artery disease (INOCA): developing evidence-based therapies and research agenda for the next decade. Circulation 2017;135:1075-92.
- Gulati M, Cooper-DeHoff RM, McClure C, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women's Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch Intern Med 2009;169:843-50.
- Pepine CJ, Anderson RD, Sharaf BL, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung, and Blood Institute WISE (Women's Ischemia Syndrome Evaluation) study. J Am Coll Cardiol 2010;55:2825-32.
- Jespersen L, Hvelplund A, Abildstrom SZ, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 2012;33:734-44.
- Murthy VL, Naya M, Taqueti VR, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 2014;129:2518-27.
- Konst RE, Guzik TJ, Kaski JC, et al. The pathogenic role of coronary microvascular dysfunction in the setting of other cardiac or systemic conditions. Cardiovasc Res 2020;116:817-28.
- Bairey Merz CN, Pepine CJ, Shimokawa H, Berry C. Treatment of coronary microvascular dysfunction. Cardiovasc Res 2020;116:856-70.
- Pizzi C, Manfrini O, Fontana F, Bugiardini R. Angiotensin-converting enzyme inhibitors and 3-hydroxy-3-methylglutaryl coenzyme A reductase in cardiac Syndrome X: role of superoxide dismutase activity. Circulation 2004;109:53-8.
- Chen JW, Hsu NW, Wu TC, Lin SJ, Chang MS. Long-term angiotensin-converting enzyme inhibition reduces plasma asymmetric dimethylarginine and improves endothelial nitric oxide bioavailability and coronary microvascular function in patients with syndrome X. Am J Cardiol 2002;90:974-82.
- Hamasaki S, Higano ST, Suwaidi JA, et al. Cholesterol-lowering treatment is associated with improvement in coronary vascular remodeling and endothelial function in patients with normal or mildly diseased coronary arteries. Arterioscler Thromb Vasc Biol 2000;20:737-43.
- Indraratna P, Naoum C, Ben Zekry S, et al. Aspirin and statin therapy for nonobstructive coronary artery disease: five-year outcomes from the CONFIRM Registry. Radiol Cardiothorac Imaging 2022;4:e210225.
- Ovrehus KA, Diederichsen A, Grove EL, et al. Reduction of myocardial infarction and all-cause mortality associated to statins in patients without obstructive CAD. JACC Cardiovasc Imaging 2021;14:2400-10.
- Pauly DF, Johnson BD, Anderson RD, et al. In women with symptoms of cardiac ischemia, nonobstructive coronary arteries, and microvascular dysfunction, angiotensin-converting enzyme inhibition is associated with improved microvascular function: A double-blind randomized study from the National Heart, Lung and Blood Institute Women's Ischemia Syndrome Evaluation (WISE). Am Heart J 2011;162:678-84.
- Bavry AA, Handberg EM, Huo T, et al. Aldosterone inhibition and coronary endothelial function in women without obstructive coronary artery disease: An ancillary study of the National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation. Am Heart J 2014;167:826-32.
- Bairey Merz CN, Handberg EM, Shufelt CL, , et al. A randomized, placebo-controlled trial of late Na current inhibition (ranolazine) in coronary microvascular dysfunction (CMD): Impact on angina and myocardial perfusion reserve. Eur Heart J 2016;37:1504-13.
- Merz CN, Olson MB, McClure C, et al. A randomized controlled trial of low-dose hormone therapy on myocardial ischemia in postmenopausal women with no obstructive coronary artery disease: Results from the National Institutes of Health/National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE). Am Heart J 2010;159:987 e981-87.
- Rambarat CA, Elgendy IY, Handberg EM, et al. Late sodium channel blockade improves angina and myocardial perfusion in patients with severe coronary microvascular dysfunction: Women's Ischemia Syndrome Evaluation-Coronary Vascular Dysfunction ancillary study. Int J Cardiol 2019;276:8-13.
- Eriksson BE, Tyni-Lenne R, Svedenhag J, et al. Physical training in Syndrome X: physical training counteracts deconditioning and pain in Syndrome X. J Am Coll Cardiol 2000;36:1619-25.
- Henry TD, Bairey Merz CN, Wei J, et al. Autologous CD34+ stem cell therapy increases coronary flow reserve and reduces angina in patients with coronary microvascular dysfunction. Circ Cardiovasc Interv 2022;15:e010802.
- Corban MT, Toya T, Albers D, et al. IMPROvE-CED Trial: Intracoronary autologous CD34+ cell therapy for treatment of coronary endothelial dysfunction in patients with angina and nonobstructive coronary arteries. Circ Res 2022;130:326-38.
- Sidik NP, McEntegart M, Roditi G, et al. Rationale and design of the British Heart Foundation (BHF) Coronary Microvascular Function and CT Coronary Angiogram (CorCTCA) study. Am Heart J 2020;221:48-59.
- Morrow AJ, Ford TJ, Mangion K, et al. Rationale and design of the Medical Research Council's Precision Medicine with Zibotentan in Microvascular Angina (PRIZE) trial. Am Heart J 2020;229:70-80.
- Abraham GR, Morrow AJ, Oliveira J, et al. Mechanistic study of the effect of endothelin SNPs in microvascular angina - protocol of the PRIZE Endothelin Sub-Study. Int J Cardiol Heart Vasc 2022;39:100980.
- Handberg EM, Merz CNB, Cooper-Dehoff RM, et al. Rationale and design of the Women's Ischemia Trial to Reduce Events in Nonobstructive CAD (WARRIOR) trial. Am Heart J 2021;237:90-103.
Clinical Topics: Acute Coronary Syndromes, Cardiac Surgery, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Cardiac Surgery and Heart Failure, Acute Heart Failure, Pulmonary Hypertension, Interventions and ACS, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Hypertension
Keywords: ACC Publications, Cardiology Magazine, Hypertension, Pulmonary, Metabolic Syndrome, Acute Coronary Syndrome, Myocardial Revascularization, Fractional Flow Reserve, Myocardial, Heart Failure, Coronary Artery Disease, Angiography, Aneurysm, Cardiology Magazine Spotlight Series
< Back to Listings