Findings of the MANIFEST PF Survey: Real World Experience With Pulsed Field Ablation
Quick Takes
- The MANIFEST-PF survey aims to assess whether pulsed field ablation (PFA) delivers on safety and efficacy when employed in commercial use.
- Acute procedural success involving isolation of the pulmonary veins was almost universally achieved.
- Complications were rare and not associated directly with PF ablation. Larger studies will be needed to assess for rare complications specific to PFA.
There is increasing evidence that early intervention with rhythm control in atrial fibrillation (AF), most prominently with catheter ablation, can reduce not only the burden of arrhythmia but associated adverse outcomes such as stroke, heart failure (HF) and even mortality.1,2 Pulsed field ablation (PFA) is a non-thermal technology which has the potential to revolutionize the ablation of AF and further drive strategies in patient care. PFA energy's inherent selectivity for myocardium combined with its relative sparing of tissue architecture appears to result in reduced risks of phrenic nerve injury, pulmonary vein stenosis and atrial-esophageal fistula when compared to the indiscriminate tissue injury provided by thermal sources.3-6 Indeed, in early clinical and pre-clinical data it offers comparable if not superior efficacy to conventional techniques with improved safety.7-9
While the promise of PFA has been realized in small studies with experienced operators, the safety and efficacy profile of this technology remains to be proven in a larger scale. The MANIFEST-PF survey aims to summarize a "real-world" experience of PFA in commercial practice after the regulatory approval of the single-shot, pentaspline PFA catheter and compatible generator (Farapulse PFA System, Boston Scientific).10
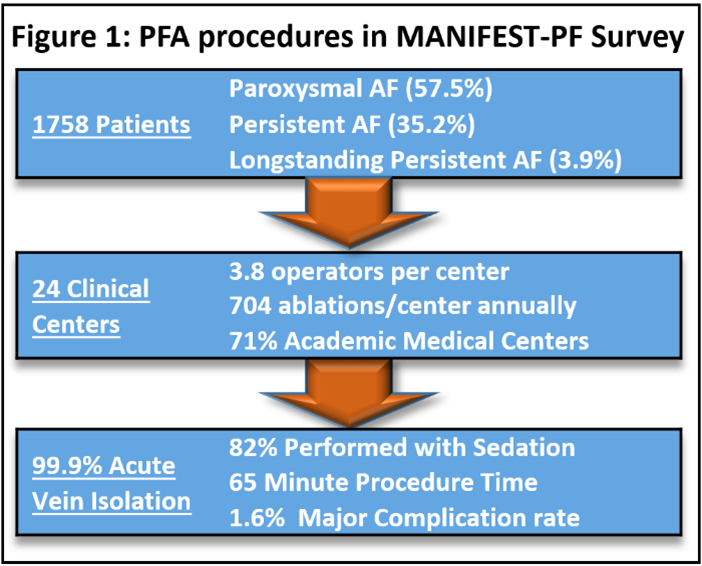
A survey was sent to all 24 centers in nine European Union countries with experience in PFA with a 100% response rate. Each center contributed from their respective institutional-level patient databases to culminate in a total of 1,758 patients undergoing ablation between March 2021 and January 2022. Patients treated included a mix of paroxysmal (57.5%), persistent (35.2%), or long-standing persistent AF (2.9%) with the majority of procedures (93.5%) being first-time ablations.
Most procedures (82.1%) were performed under deep sedation without endotracheal intubation with (84.9%) spending at least one night in the hospital. The mean procedural time was 65 minutes with an acute vein isolation rate of 99.9% (range 98.9-100%). The rates of major complications were 1.6% consisting mostly of pericardial tamponade and stroke with one stroke resulting in mortality (Table 1). Minor complications reached 3.86% and were mainly related to vascular access. Three "unusual adverse events" were reported including one case of coronary artery spasm, a second involving hemoptysis and a third with a chronic cough which persisted for 6 weeks post procedure. There were no reported cases atrial-esophageal fistulas, pulmonary vein stenosis or persistent phrenic nerve injuries.
Table 1: Rates of Complications During PFA. Courtesy of Musikantow DR, Koruth J.
| Major Complications | N (%) | Minor Complications | N (%) |
| Pericardial Tamponade | 17 (0.97) | Transient Ischemic Attack (TIA) | 2 (0.11) |
| Stroke | 7 (0.39) | Transient Phrenic Nerve Injury | 8 (0.46) |
| Vascular Complications Requiring Surgery | 4 (0.23) | Vascular Complications Not Requiring Surgery | 56 (3.28) |
| Coronary Spasm | 1 (0.06) | Other | 2 (0.11) |
| Death | 1 (0.06) |
MANIFEST-PF suggests that the safety and remarkable acute procedural success demonstrated in the early clinical studies can be achieved across a range of centers and operators in real-world practice. Complications in this series were rare and largely unrelated to the ablative modality employed (vascular access, pericardial effusion).
There are several inherent limitations in this analysis, the most notable of which is that it is a retrospective survey relying on the individual collection of data from each respective center raising potential for under-reporting. Secondly, while rates of acute vein isolation approach 100%, this study offers no insight into the long term success in both durable vein isolation and recurrence of atrial arrhythmias. Finally, the incidence of severe complications attributed to thermal energy (atrial-esophageal fistula, phrenic nerve palsy, pulmonary valve stenosis) are rare and similar complications may not be realized even with the number of patients assessed in this study.11 Additional analyses featuring longer follow up and larger patient populations remain necessary to further validate the success and safety of PF ablation.
References
- Kirchhof P, Camm AJ, Goette A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med 2020;383:1305-16.
- Packer DL, Mark DB, Robb RA, et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 2019;321:1261-74.
- Kaminska I, Kotulska M, Stecka A, et al. Electroporation-induced changes in normal immature rat myoblasts (H9C2). Gen Physiol Biophys 2012;31:19-25.
- van Driel VJHM, Neven K, van Wessel H, Vink A, Doevendans PA, Wittkampf FH. Low vulnerability of the right phrenic nerve to electroporation ablation. Heart Rhythm 2015;12:1838-44.
- Neven K, van Es R, van Driel V, et al. Acute and long-term effects of full-power electroporation ablation directly on the porcine esophagus. Circ Arrhythm Electrophysiol 2017;10:e004672.
- van Driel VJ, Neven KG, van Wessel H et al. Pulmonary vein stenosis after catheter ablation: electroporation versus radiofrequency. Circ Arrhythm Electrophysiol 2014;7:734-38.
- Reddy VY, Neuzil P, Koruth JS, et al. Pulsed field ablation for pulmonary vein isolation in atrial fibrillation. J Am Coll Cardiol 2019;74:315-26.
- Cochet H, Nakatani Y, Sridi-Cheniti S, et al. Pulsed field ablation selectively spares the oesophagus during pulmonary vein isolation for atrial fibrillation. Europace 2021;23:1391-99.
- Reddy VY, Anic A, Koruth J, et al. Pulsed field ablation in patients with persistent atrial fibrillation. J Am Coll Cardiol 2020;76:1068-80.
- Ekanem E, Reddy VY, Schmidt B, et al. Multi-national survey on the methods, efficacy, and safety on the post-approval clinical use of pulsed field ablation (MANIFEST-PF). Europace 2022;24:1256-66.
- Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design: a report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation. Developed in partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC) and the European Cardiac Arrhythmia Society (ECAS); and in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), the Asia Pacific Heart Rhythm Society (APHRS), and the Society of Thoracic Surgeons (STS). Endorsed by the governing bodies of the American College of Cardiology Foundation, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, the Asia Pacific Heart Rhythm Society, and the Heart Rhythm Society. Heart Rhythm 2012;9:632-696 e21.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Pericardial Disease, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias
Keywords: Ischemic Attack, Transient, Cardiac Tamponade, Incidence, Pericardial Effusion, Hemoptysis, Retrospective Studies, Follow-Up Studies, Catheter Ablation, Atrial Fibrillation, Stenosis, Pulmonary Vein, Myocardium, Intubation, Intratracheal, Fistula, Spasm
< Back to Listings