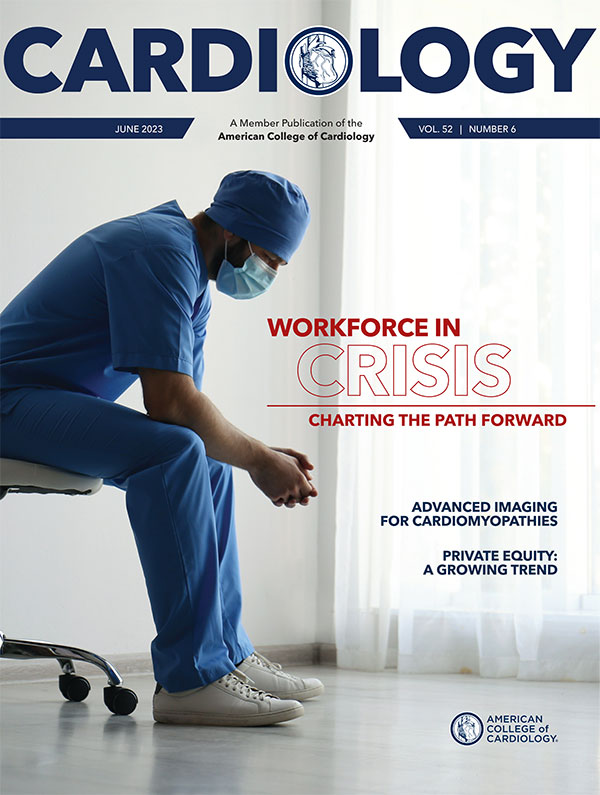
Workforce in Crisis: Charting the Path Forward
With not enough clinicians available to meet the needs of an ever-increasing patient population, the cardiology profession is on the brink of a crisis. In findings from an ACC Task Force convened by the Board of Trustees (BOT), long training and certification pathways, hyper-specialization, unfavorable work-life balance and an insufficient supply of physicians, APPs, nurses and allied health professionals, are the four primary stressors impacting the workforce supply. Meanwhile, an aging population that is living longer and with multiple comorbidities, coupled with other factors like the increasing complexity of cardiovascular care, are among the leading pressures augmenting demand for care.
"The challenges underlying the clinical workforce crisis in cardiology, common to cardiologists, nurses and CV Team members, are numerous and at times seem overwhelming," says ACC Immediate Past President Edward T.A. Fry, MD, MACC, who made solving for the workforce crisis one of the main priorities of his presidential year. "We must attack all the contributing factors now realizing that some are more likely to have short-term solutions and others long-term. Even if we are not 'boiling the ocean,' we need to at least turn on the burner."
Cardiology asked Fry, members of the Task Force, as well as other College leaders, for their thoughts on what it will take to navigate this crisis. Specifically, we take a deeper look at the Task Force's proposed steps forward that were presented during ACC.23/WCC in New Orleans, which include pursuing changes in training and certification pathways, incentivizing careers in general cardiology, providing well-being resources, promoting team-based care, creating new models and tools that optimize workflow, driving payment reform and incentives alignment, and partnering to better manage cardiovascular disease.
Partners in Care Transformation
"The best way to manage cardiovascular disease is to never develop it in the first place," says Thomas M. Maddox, MD, MSc, FACC, Task Force chair and BOT member. Accordingly, he notes, partnering with other cardiovascular societies, patient groups and key stakeholders to encourage the development and implementation of prevention programs, advocate for state and federal funding for education and research, and to provide clinical guidance and best practices can play an important role in solving for the workforce crisis and slowing the demand for cardiovascular care.
Tackling health equity in collaboration with community groups, industry and government partners is another critical element in managing cardiovascular disease. According to Fry, "advancing equity will require acknowledging and addressing implicit biases; accurately and objectively measuring health outcomes to reveal inequities; recognizing and closing gaps in quality outcomes among groups of patients; and effectively advocating for removal of structural barriers to equitable access, care and health outcomes."

– Edward T.A. Fry, MD, MACC
Social determinants of health account for 80% of cardiovascular health outcomes, making it imperative that addressing these factors are a focus for the ACC – and quite frankly everyone, says Paul L. Douglass, MD, MACC, chair of the ACC's Health Equity Task Force.
Ensuring everyone has the right to achieve their best health outcomes is everyone's responsibility – a responsibility the ACC takes very seriously. "The ACC has been on an evolutionary journey towards reducing health disparities and committing to achieving health equity," he says. "The elimination of health disparities would result in billions of dollars in health-related financial burden reduction."
Innovation can also play a role in better managing care, mitigating the impacts of social determinants of health, and helping to optimize clinician workflow by reducing burdens of day-to-day practice. "Virtual outreach clinics, creative uses of APPs and other allied professionals, and anticipatory care via predictive analytics are all promising approaches," says Maddox.
Among the biggest opportunities: the creative use of artificial intelligence (AI) to help streamline and simplify workflows across the cardiovascular care team, whether it's being used to screen for normal echoes, EKGs and other cardiac imaging texts, helping to incorporate use of evidence-based clinical guidance at the point of care, or assisting with the triage of tasks across a multidisciplinary team.
Additionally, Maddox highlights opportunities inherent in digital transformation, to optimize remote patient monitoring and telehealth and move care to a patient's home or workplace and allow for more personalized, equitable and accessible care.
Teaming Up
Short-Term and Long-Term Solutions

Addressing the workforce crisis will require both short-term and long-term interventions. It will also mean bringing together all of ACC's assets tied to Prevention (science, clinical guidance, research), Education (training, nonclinical competency, leadership training), Innovation (digital health, care delivery redesign, implementation science) and Advocacy (legislative, regulatory, health systems).
"This is an all-hands-on-deck call for involvement from all," says ACC Past President Edward T.A. Fry, MD, MACC, who offers up his thoughts on opportunities both now and into the future.
Short-Term Opportunities:
- Extension of senior cardiologists' careers through creative modified scheduling to provide expanded general cardiology coverage and access.
- Greater flexibility in scheduling and childcare support for physicians, nurses and technical staff.
- Expansion and optimization of true team-based care where everyone works at the top of their license and training.
- Operational audits and care redesign focused on efficiency and patient experience.
- Reconfiguration and optimization of EHR templates and functionality.
- Effective delegation of clinical tasks cascaded throughout the care team supported by clinician-designed and evidenced-based algorithms.
- Equipping the entire cardiovascular team with nonclinical competencies to better manage their system of care delivery and effectively utilize implementation science principles.
- Changing incentive models to support value-based care.
Longer-Term Opportunities:
- Expand training of physicians and nurses through funding of more training programs.
- Shorten internal medicine training for those who identify a desire to enter cardiology fellowships and consolidate general and subspecialty training.
- Engage health care systems to support a greater portion of care team development.
- Advocate to modernize payment incentives that foster creativity and high value care.
- Support and implement innovations that promote efficiency and reduce burdens (e.g., AI-enabled image interpretation, clinical decision support, etc.).
Promoting team-based care and leveraging the entire cardiovascular team to the fullest extent possible must play a critical role in solving for workforce issues. All members of the cardiovascular care team need to be empowered to lead care transformation within their organizations and institutions.
According to Kimberly Guibone, DNP, ACNP-BC, FACC, the new CV Team Lead for ACC's Annual Scientific Session, "the workforce crisis highlights the need to engage, empower and support the CV Team." For example, expanded use of APPs can improve access to care along the continuum and help close gaps in care, especially when paired with use of digital technologies like telehealth and remote monitoring, she says.
MedAxiom CEO Jerry Blackwell, MD, MBA, FACC, agrees, noting that current MedAxcess data show a growing number of cardiovascular practices are using APPs, with many approaching a 1:1 ratio between physicians and APPs with sophisticated care protocols and scripted messaging for patients around the role/value of APPs. "There is almost universal recognition in organizations of any size/complexity and with any ownership model that team-based care is required to meet the needs of patients and society," he says.
However, Blackwell says the number of practices using APPs could still be improved and the needle moved closer to 100%. He notes that some practices and systems focus their team-based approach on the provider side, directing resources almost exclusively to the patient-facing aspects of their practices (i.e., MAs, RNs and APPs), while others focus on the administrative side of team-based care, directing resources to optimize back-office functions (i.e., coding/billing, practice management, people operations, etc.).
The best performing organizations have realized that it is best to do both. "Failing to recognize the integrated clinical/business nature of contemporary cardiovascular practices is a mistake," Blackwell cautions. "A highly functional dyad model is optimal in almost all cases."
Looking ahead, both Guibone and Blackwell say that ongoing calibration of team-based care will be critical as practices, hospitals and health systems aim to define shared goals, clarify roles, and identify opportunities for collaboration and patient-centered care.
Building the Professional Pipeline
Strengthening and expanding the trainee pipeline and incentivizing careers in cardiology, especially among those currently underrepresented in cardiovascular medicine, is another important piece of the workforce puzzle.
"The ACC is committed to ensuring the development of a cardiovascular workforce that reflects the community that we are devoted to serving," says Douglass. "Developing a workforce that is aligned with our Mission, Vision and Values is key to our success and productivity in terms of business strategy, clinical strategy and educational strategy."
Efforts like the College's Young Scholars Program, Internal Medicine Program and the Clinical Trial Research Program are already starting to demonstrate success in helping to grow and expand the pipeline of cardiovascular clinicians to better reflect the diverse patient populations needing care.
According to Douglass, these programs, along with others, have made significant strides over the last few years in introducing a diverse, collaborative and inclusive network of individuals to careers in cardiovascular medicine. "Much work is still to be done," he says, "but the ACC's long-term commitment of financial and human resources toward this aim will help us achieve our goals."

– Kimberly Guibone, DNP, ACNP-BC, FACC
ACC's Member Sections are also helping clinicians find their niche in the College as early as medical school and grow in their professional knowledge throughout the course of their career. Additionally, Sections are important catalysts in ACC efforts to advocate for and implement educational programming, leadership training, mentoring and other initiatives aimed at creating a diverse and inclusive profession.
Improving Training and Well-Being
Workforce Quick Links
ACC Diversity, Equity and Inclusion Hub
Medical education is evolving and expanding rapidly as a result of increased global access to digital technologies and external factors like the COVID pandemic, which changed the landscape forever in terms of digital and hybrid learning. New technologies and digital platforms have helped to lower geographic and cost barriers and opened the doors to innovate and more effectively and efficiently deliver cardiovascular education across the care team.
"As we think about the needs of the cardiovascular workforce, leaning in to evidence-based education is important," says Julie B. Damp, MD, FACC. "Defining competency and understanding meaningful assessment in cardiovascular education helps us identify the skills needed for clinicians of all types and hone our ability to effectively assess achievement of these skills, allowing education to be tailored to the needs of the workforce."
Integrating nonclinical competency training into traditional clinical competency training as part of graduate and lifelong medical education is one important consideration. The ACGME already provides cardiovascular training "milestones" to aid in the shift to competency-guided education, and the Core Cardiovascular Training Statement (COCATS4) has evolved in the last decade to include training recommendations for cardiovascular fellows that include a full array of clinical and nonclinical competencies expected of clinical cardiologists upon completion of fellowship training. These efforts only continue to evolve, with the ACC continuing to provide training guidelines to help programs and trainees understand what skills are needed and the strategies needed to achieve competence.

– Paul L. Douglass, MD, MACC
"Within cardiovascular training, we continue to work towards accurate, meaningful methods of assessment, which will help determine how we can best use educational resources to provide each trainee with the skills they specifically need on a timeline that aligns with their development," says Damp.
In addition to training and competency-based education, addressing clinician well-being across the entire care time is vital in today's workforce. Educating about self-care strategies and advocating for institutional and training program policies that facilitate improved well-being can aid in long-term retention and mitigate burnout, while also helping to attract more individuals to the field.
Advocating For Change

Payment models that incentivize high-quality clinical outcomes and patient satisfaction at efficient and fiscally responsible costs are the North Star of ACC Advocacy efforts to advance health policy solutions that address clinician reimbursement and help to align incentives – key tenets of the Workforce Task Force roadmap.
According to William A. Van Decker, MD, FACC, chair of the ACC's Health Affairs Committee, there are several early opportunities in the sphere of evolving value-based care/payment reform helped by the current national spotlight. First and foremost is the need for the ACC and the broader medical community to advocate for stability in the Medicare Physician Fee Schedule and yearly positive updates based on the rate of inflation.
Second, a push for outcomes-focused collaborative care models that are flexible and locally adaptable, encourage patient choice and support access to CV specialty services at all stages of care, is necessary to keep patients healthier and improve quality of life and outcomes. Decreasing administrative burden on clinicians as a means of keeping the clinician workforce happy and productive is another important priority, he says.
Key to successful payment reform is ensuring a variety of flexible payment model options that are tailored to local care delivery needs, as well as the creation of governance models that recognize and reward clinicians for shared saving and value-based successes. Van Decker cautions that any model should minimize administrative burden to the greatest possible degree. He adds that clinical data registries can and should play a role in value-based care efforts.
"The impact of payment and practice reform on physician well-being is an important one," he says. "Initially, change is always difficult, but hopefully consistent communication, more financial stability in the system (without extracting competition and innovation), and fewer tasks not related to directing an optimal patient outcome will go a long way to provide peace of mind, promote the best care, and ensure the professional satisfaction of the cardiovascular workforce."
The Role of the Professional Home
The ACC will continue to take a leadership role in the discussion around workforce needs and identifying and implementing ways to address these needs and mitigate barriers. The College's next Strategic Plan, which will launch in January 2024, will be critical to this endeavor, with two key initiatives focused on optimizing the College's support for cardiovascular education and developing best practices for care delivery.
– Julie B. Damp, MD, FACC
"These initiatives will have a significant impact on our cardiovascular workforce pipeline and the experiences that our cardiovascular teams have in delivering frontline care," says Maddox. "The timing is fortuitous!"
In addition, the College is working with other stakeholder organizations on new training pathways within cardiology and is well positioned to lead the field in driving educational innovation, informing value-based care models, and growing a diverse pipeline of clinicians that can effectively meet the needs of patients around the world.
"I believe these efforts and other planned activities along with the ACC's continued commitment to embedding health equity into our Strategic Plan will pay real and meaningful dividends," says Douglass. "This goal is not a destination, but a journey that the ACC is providing the Vision, Mission and resources to achieve."
Call to Action: Re-Engineering Cardiology Care Delivery to Meet Growing Demands

For more than a decade there have been growing concerns about the annual net reduction in cardiologists who are part of the U.S. physician workforce. The causes of this deficit are numerous but are mainly driven by two key factors: 1) the aging of the existing cardiology population, and 2) fewer cardiologists entering the workforce through fellowships. Based on 2020 MedAxiom data, approximately one-quarter of practicing cardiologists were 61 years of age and older.1
These data further show that cardiologists in their 60s produce fewer work relative value units (wRVUs) than their younger peers.
Considering both the decline in wRVU production of the existing workforce and using statistical projections for physician slowdown and departures, an annual deficit of more than 500 cardiologists is estimated.
The same aging phenomenon that is impacting the cardiology workforce is also happening to the general population of the U.S. The "Baby Boom" generation of people born between 1946 and 1964 following the end of World War II have now entered their 60s and 70s and are generally consuming more health care – particularly cardiology.
Further, the demand curve for cardiovascular services is being pushed up by an increase in cardiac risk factors, such as obesity, hyperlipidemia, diabetes and hypertension.
Another trend increasing demand for cardiology services is the change in how a significant portion of primary care is delivered. Responding to acute national physician shortages, mega corporations like Amazon, CVS and Walmart are adding primary care services within their retail stores or building dedicated new offerings.
The vast majority of care in these settings is rendered by APPs. These nonphysician professionals, such as nurse practitioners and PAs, tend to have a lower threshold to refer a patient to a specialist.
Care Team Evolution
Click here to take the ACC/MedAxiom CV Care Delivery Assessment to determine if your facility is ready to benefit from one or more of ACC's Accreditation Services.
One way cardiology practices have adapted to meet the increasing patient demand is by increasing the deployment of APPs. According to MedAxiom data, from 2012 to 2021 the ratio of APPs to cardiologists increased nearly 70% from .36 APP FTEs per cardiologist to .60 FTEs.
Based on these data, this trend will need to continue for the next 10 years to maintain a similar cardiovascular provider (physicians plus APPs) ratio per 1,000 active patients.
However, simply expanding the APP workforce will likely be insufficient to meet future cardiovascular service demands. The care team itself may need to be extended to better utilize nurses, medical assistants, pharmacists and administrative personnel in a coordinated and standardized fashion.
Additionally, the orientation of these invaluable team members will need to change from serving the physician to serving patient populations.
Virtual and Digital Care of the Future
Click here to access MedAxiom's 2022 Cardiovascular Provider Compensation and Production Survey and learn more about MedAxiom Care Transformation Services.
Learn more about ACC's Innovation Program initiatives and access a focused workbook on telehealth best practices at ACC.org/InnovationProgram.
Virtual care remains a promising and underutilized opportunity in the struggle to match cardiology supply with demand. However, sustainable strategies must be implemented to ensure it's here to stay.
While virtual care was rapidly adopted early in the COVID pandemic, virtual visits receded quickly by late summer of 2020. Without more comprehensive changes to integrate virtual care into the health system, it will not be a sustainable part of the solution to improving access to care.
Digital care has also emerged. Newer generations of patients are increasingly using digital wearables and monitoring devices, and more and more people are using patient portals to review their charts and test results. Data are pouring in through these informatic firehoses, yet everything is still handled manually – each test result, each patient message, each phone call, each appointment reminder, each office visit and/or each hospital procedure.
Outside of traditional health systems, retail clinics, payment upfront urgent care, telemedicine and digital health care companies are thriving. Venture capital funding into the digital market peaked at $16.8 billion in Q2 of 2021.2 These investments suggest there is a growing demand for these digital services and that new technology tools are on the horizon.
Re-Engineering CV Care Starts Now
What is needed is a re-engineering of the entire care process. Data strongly suggest that over time the demand for cardiovascular services will increase faster than the growth in the provider community to manage it.
Two areas that are ripe for continued innovation are the advancement of the cardiovascular care team and the utilization of virtual care – not simply replacing an in-person visit with a video chat, but truly creating a comprehensive digital care platform.
Given these mathematical realities, the cardiovascular community can't afford to wait for legislative or payer-sponsored fixes to supply and demand challenges. The cardiovascular specialty, which has always been at the forefront of care evolution and innovation, must lead the way by shaping future care delivery models.
This article was authored by Xiaoyan Huang, MD, FACC, chief of clinical cardiology, Providence Heart Institute, Portland, OR; Meredith Rosenthal, PhD, C. Boyden Gray Professor of Health Economics and Policy, Harvard TH Chan School of Public Health, Boston, MA; and Joel Sauer, MBA, Executive Vice President of Consulting, MedAxiom.
References
- Sauer J. MedAxiom. 2021 Cardiovascular Provider Compensation and Production Survey Report.
- Shah BR, Schulman K. Do Not Let a Good Crisis Go to Waste: Health Care's Path Forward with Virtual Care. NEJM CatalystMarch 2021
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Dyslipidemia, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Pericardial Disease, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Sports and Exercise Cardiology, Stable Ischemic Heart Disease, Valvular Heart Disease, Vascular Medicine, Anticoagulation Management and ACS, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Cardiac Surgery and SIHD, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Acute Heart Failure, Pulmonary Hypertension, Interventions and ACS, Interventions and Imaging, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Hypertension, Sleep Apnea, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology, Sports and Exercise and ECG and Stress Testing, Sports and Exercise and Imaging, Chronic Angina
Keywords: ACC Publications, Cardiology Magazine, Work-Life Balance, Cardiologists, Fellowships and Scholarships, Population Growth, Workforce, Cardiology, Office Visits, Telemedicine, Informatics, Health Services Accessibility, Ambulatory Care, Wearable Electronic Devices, Acute Coronary Syndrome, Anticoagulants, Arrhythmias, Cardiac, Cardiac Surgical Procedures, Metabolic Syndrome, Angina, Stable, Heart Defects, Congenital, Dyslipidemias, Geriatrics, Heart Failure, Angiography, Diagnostic Imaging, Pericarditis, Secondary Prevention, Hypertension, Pulmonary, Sleep Apnea Syndromes, Sports, Exercise Test, Heart Valve Diseases, Aneurysm
< Back to Listings