Peripheral Matters | PAD: Putting the 2024 Guideline Into Practice
New guidance for clinicians for the evaluation and management of patients with lower extremity peripheral artery disease (LE PAD) was published in May. The 2024 ACC/AHA guideline for LE PAD, the first comprehensive update since 2016, provides evidence-based recommendations for patients across the clinical spectrum.
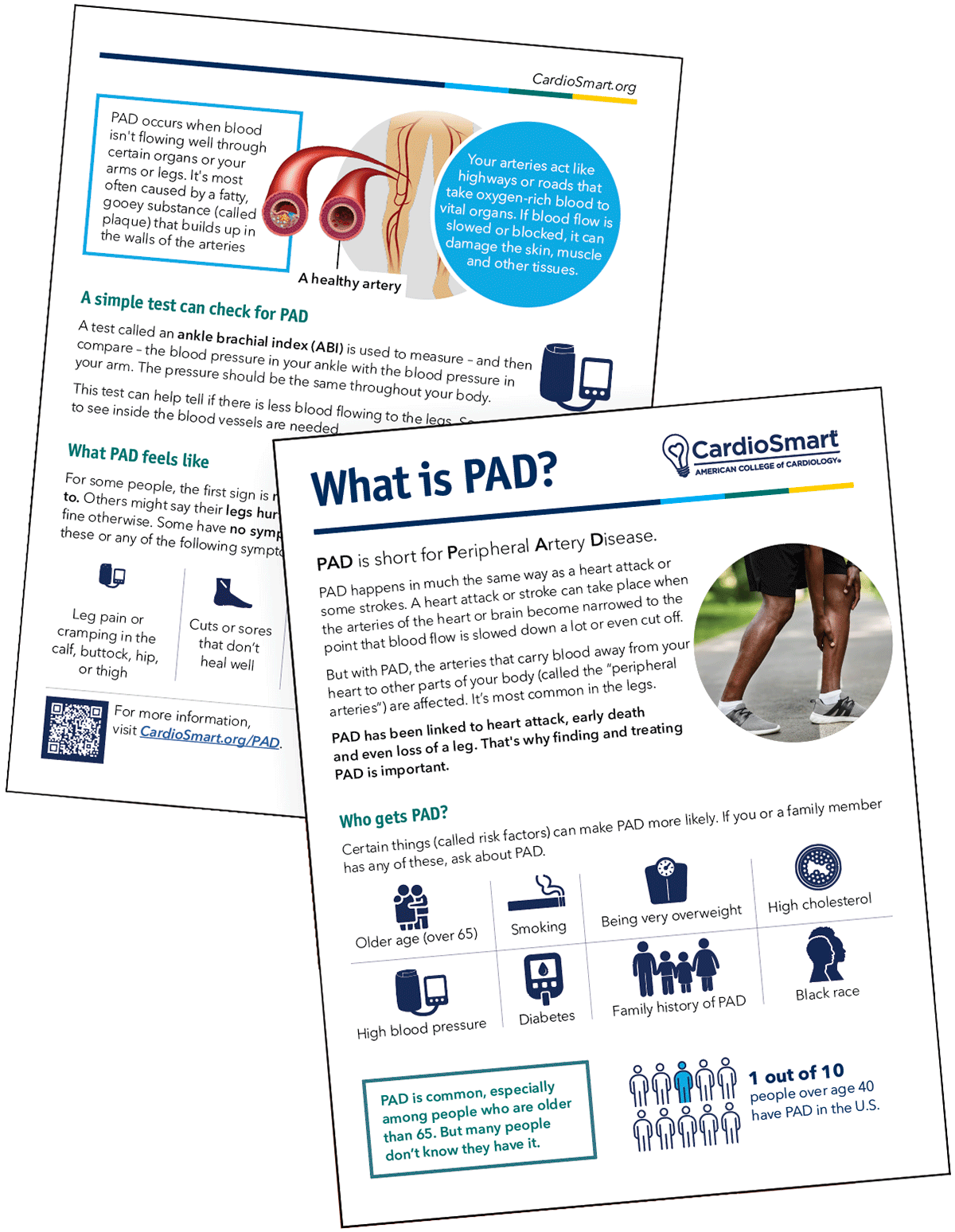
The burden of PAD is high. In the U.S., 10-12 million people have LE PAD, a condition often overlooked and that disproportionately affects those who reside in underserved communities. PAD is associated with an increased risk of major adverse cardiovascular events (MACE), including death, myocardial infarction and stroke, and with major adverse limb events (MALE), including need for amputation. For many, PAD culminates in impaired walking ability, functional status and quality of life.
Clinical Manifestations of PAD
The guideline defines four clinical subsets of PAD. The disease may be present without leg symptoms, and although functional impairment may be present, about 20-60% of patients with established PAD report no symptoms whatsoever.
Among those with symptoms, the most common clinically evident subset is those patients with chronic symptomatic disease, including claudication and other non–joint-related symptoms that impact walking performance; classically, these symptoms are absent at rest, progress with exercise intensity and resolve with cessation of activity after a few minutes.
Other patterns of exertional leg symptoms can also be present among patients with chronic symptomatic PAD. Between approximately 10-20% of patients with PAD will develop chronic limb-threatening ischemia (CLTI; formerly known as critical limb ischemia), which may present with ischemic rest pain, non–healing wounds/ulcers or frank gangrene. Prompt evaluation and endovascular or surgical revascularization, when feasible, is necessary to facilitate limb salvage.
The most urgent/emergent clinical presentation is that of acute limb ischemia (ALI), resulting from a sudden decrease in arterial perfusion that threatens limb viability. Symptoms are typically present for less than two weeks and include pain, pallor, pulselessness, poikilothermia (coolness), paresthesias and potential for paralysis. Patients with ALI require immediate assessment, and reperfusion/revascularization in the setting of a viable limb.
Diagnostic Assessment of PAD
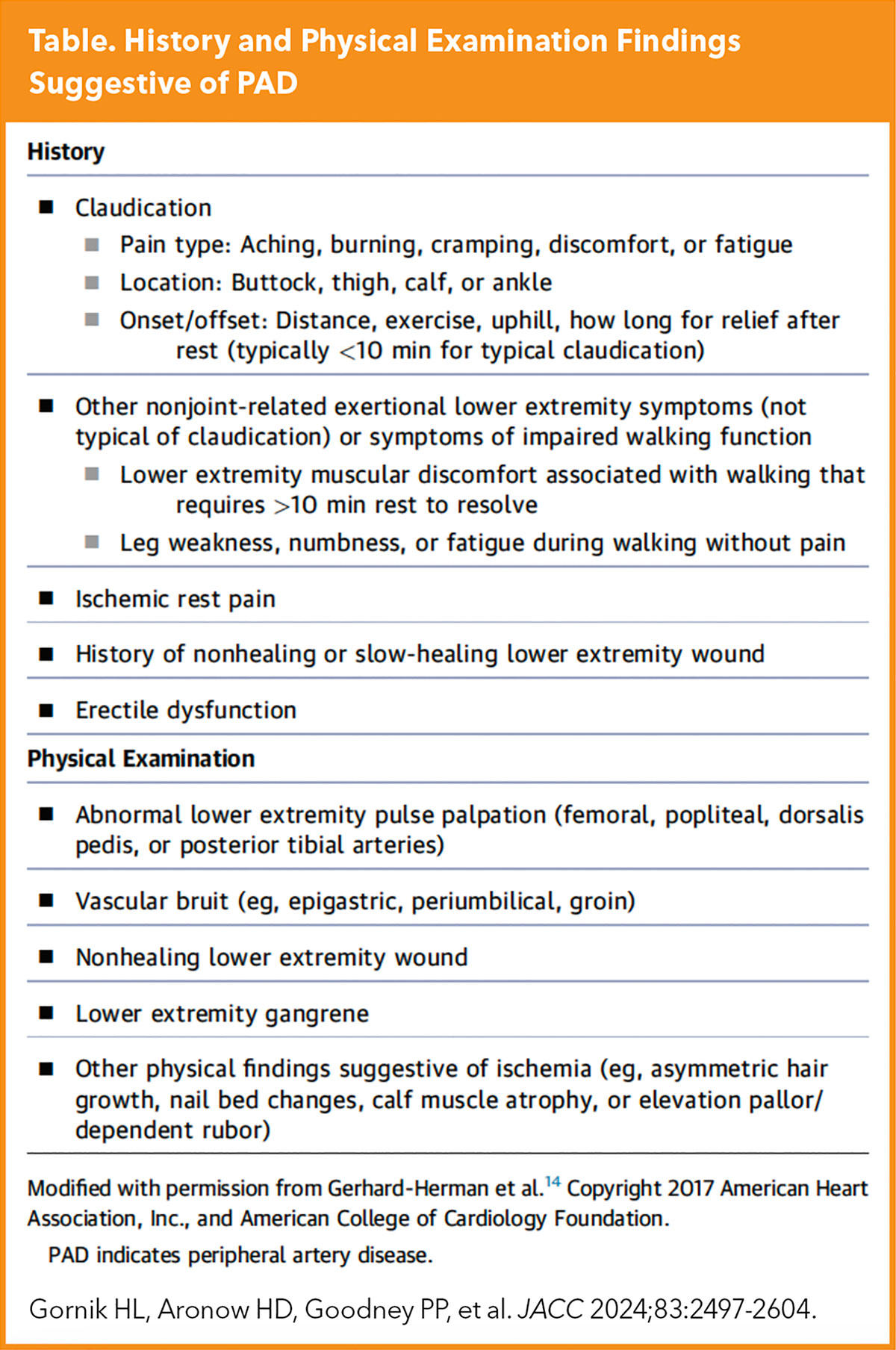
Important historical features and physical exam findings are highlighted in the guideline (Table). It is critical for practitioners to ask patients if they have difficulty walking or have leg symptoms – and to perform a thorough physical examination, including assessment for vascular bruits, characterization of pulses and a full LE skin survey (all of which require placement of patients in gowns and removal of shoes and socks).
Diagnostic studies, including the resting ankle brachial index (ABI), and additional physiological testing and their indications, are reviewed in the guideline. Multiple anatomic imaging modalities (i.e., duplex ultrasound, computed tomography angiography [CTA], magnetic resonance angiography [MRA] or catheter angiography) can be employed when considering or planning revascularization procedures.
The guideline includes diagnostic algorithms for patients who are at risk for or who have suspected PAD, as well as when CLTI is of concern.
Special Considerations in PAD
The 2024 guidleline includes a detailed section on special considerations in the most vulnerable patients with PAD, including risk amplifiers (e.g., older age, smoking, diabetes, chronic kidney disease, polyvascular disease and depression) and contributors to health disparities (e.g., race and ethnicity, gender, geography, structural racism and implicit bias, and social determinants of health).
ACC Webinar: Implementing Innovative Solutions to Achieving Equitable PAD Care
Join ACC's Health Equity Task Force, Vascular Disease Member Section, and Health Equity, Diversity, and Inclusion team on Tuesday, Sept. 10 at 7 p.m. ET for the next installment of the ACC Health Equity Webinar Series, "Implementing Innovative Solutions to Achieving Equitable PAD Care."
This webinar will review the new peripheral artery disease (PAD) guidelines, discuss health disparities and inequities in outcomes among patients with PAD, and more. Learn more.
Such disparities result in poor cardiovascular and limb outcomes in patients with PAD and should be addressed through coordinated stakeholder efforts both at the individual and population levels.
As an example, when compared with Hispanic and non-Hispanic White patients, who have a one in five lifetime risk of developing PAD, one in three Black patients will develop PAD during their lifetime. Furthermore, the risk of amputation vs. revascularization among Black patients is 77% higher compared with White patients. Clinicians and their health systems should actively seek evidence of health disparities in PAD diagnosis, treatment and outcomes, and should limit the impact of these disparities wherever possible.
Prevention and Medical Therapy For PAD
It is important that preventive foot therapy be employed for all patients with PAD. Collaboration with podiatrists and other foot care specialists can be helpful for patients with PAD, particularly those at higher risk for CLTI and foot ulcers. Among those with chronic stable symptoms (e.g., claudication), agents that improve symptoms (e.g., cilostazol) should be employed where not contraindicated.
Structured exercise therapy (SET) remains a vital component of care for patients with PAD and chronic stable symptoms. However, utilization of structured exercise programs, including SET, remains poor among patients who qualify.
Pharmacotherapy with cilostazol in combination with SET may allow many patients to forego revascularization in this setting. The armamentarium of medical therapies that reduces the likelihood of MACE and MALE has expanded over time and these agents should be routinely prescribed by all clinicians who care for patients with PAD.
These include antithrombotic therapy with antiplatelet agents (usually single antiplatelet therapy with either aspirin or P2Y12 inhibitors) and anticoagulants (e.g., dual pathway inhibition with combination low-dose rivaroxaban and low-dose aspirin for those who are not at increased bleeding risk), lipid-lowering therapy (e.g., high-intensity statins, ezetimibe and PCSK9 inhibitors), antihypertensive therapy (e.g., ACE inhibitors and ARBs), agents for those with PAD and diabetes (e.g., SGLT2 inhibitors and GLP-1 agonists), and smoking cessation interventions.
Revascularization For PAD
Revascularization for asymptomatic PAD is generally not indicated, except when performed to facilitate other lifesaving or health-improving therapies (e.g., catheter-based coronary or structural heart procedures, mechanical circulatory support, etc.).
Among those with claudication or other manifestations of chronic symptomatic PAD, endovascular or surgical revascularization may be employed electively when attempts at medical therapy, including SET, have failed and symptoms remain lifestyle-limiting.
In contrast, revascularization for patients with CLTI is paramount, barring contraindications, to minimize loss of tissue, facilitate wound healing, relieve pain and preserve limb function. The choice between endovascular and surgical approaches should be individualized and based upon many factors, including anatomy, availability of venous conduit, patient comorbidities and patient preference.
A multispecialty care team should evaluate for revascularization options before amputation occurs in these patients. Finally, among patients with ALI, prompt reperfusion is indicated to prevent limb loss and death.
Team-Based Care For PAD
The 2024 guideline emphasizes that optimal care of patients with PAD, especially when CLTI is present, requires input from and coordination through a multispecialty care team. This team should be comprised of multiple specialties and disciplines and the composition may vary depending upon available local expertise.
Potential members of the PAD multispecialty care team may include vascular medical and surgical specialists, APPs/PAs, nurses, podiatrists, orthopedic surgeons, wound care specialists, endocrinologists, internal medicine specialists, infectious disease specialists, diagnostic radiologists and other vascular imaging specialists, pharmacists, physical medicine and rehabilitation clinicians, social workers, clinical exercise physiologists, physical and occupational therapists, and nutritionists and dietitians.
Following Patients With PAD
PAD Resources
Click here to access ACC's Guideline Hub to download the full guideline and access all the tools and resources, including the Guideline app and CardioSmart infographics.
Given the chronic nature of PAD, long-term follow-up of these patients is paramount irrespective of whether revascularization has occurred. Regular clinical evaluations should include assessment for limb symptoms, functional status and quality of life, along with a lower extremity pulse and foot assessment.
Risk factors should be continually reassessed and modified as appropriate. Attention to ongoing smoking cessation and participation in structured exercise are important. Clinicians should confirm that guideline-directed medical therapies have been optimized. Surveillance following revascularization procedures may result in more durable arterial patency.
Take Action
September is PAD Awareness Month: a reminder to get-up-to speed on the new guideline and steps to incorporate it into daily practice. The 2024 multispecialty LE PAD guideline reviews the epidemiology and clinical presentation, and provides guidance on the diagnosis, prevention, treatment and long-term follow-up of this at-risk population.
Herein we've highlighted key messages and provided insights that should help translate this guideline into practice. We encourage downloading the full document and reviewing the recommendation statements and clinician-friendly algorithms.
This article was authored by Herbert D. Aronow, MD, MPH, FACC; Philip P. Goodney, MD, MS, and Heather L. Gornik, MD. Aronow and Goodney are co-vice chairs and Gornik is chair of the writing committee for the PAD Guideline.
Clinical Topics: Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Interventions and Vascular Medicine
Keywords: Cardiology Magazine, ACC Publications, Peripheral Arterial Disease, Myocardial Infarction, Stroke, Reperfusion, Quality of Life