Innovation in Precision Cardio-Oncology

Many of us can remember that patient with heart failure – that woman with cardiomyopathy we discovered was due to anthracycline chemotherapy years earlier, around two decades ago.
How can something meant to cure and help her end up hurting her?
That is the predicament in which we find ourselves in cardio-oncology. We choose this field to be among those who bring hope, health and healing to many individuals who have ever been diagnosed with cancer.
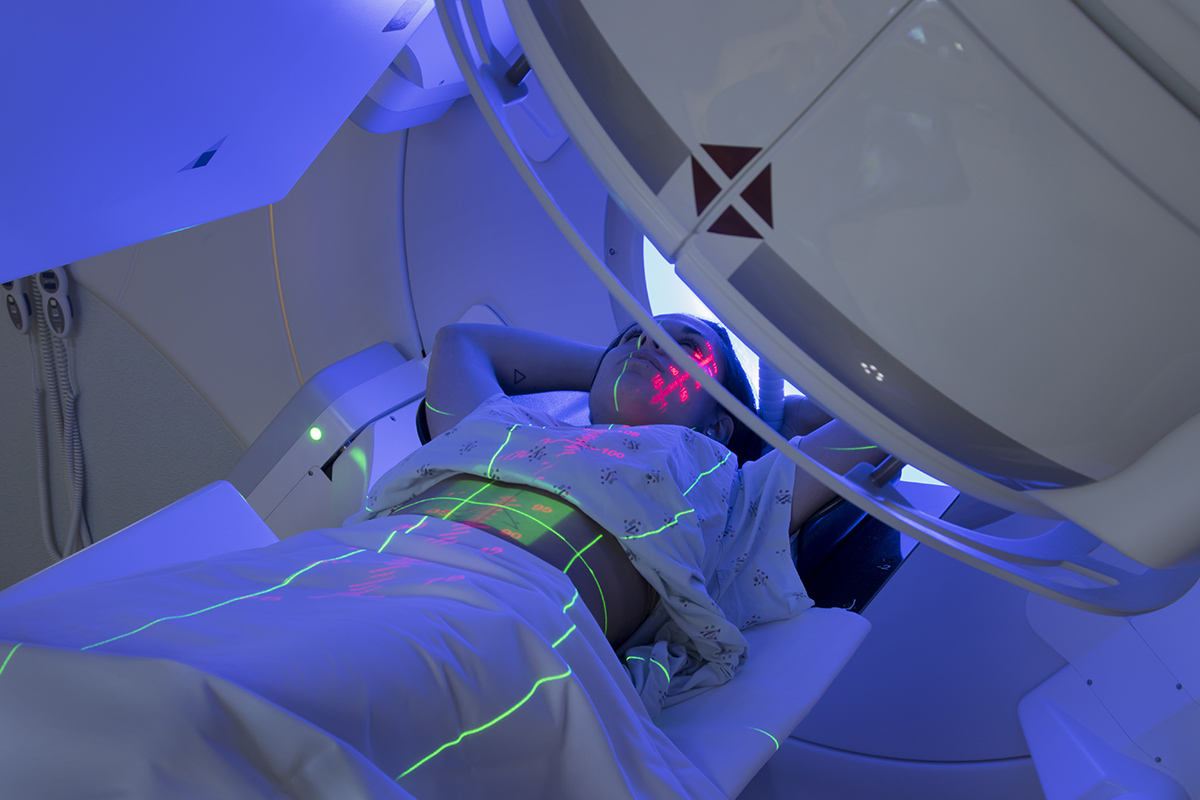
Almost no cancer patient is immune to some sort of cardiovascular effect of cancer and its associated therapies. The pericardium, myocardium, coronary vessels, valves and conduction system can all be affected. Patients often have to choose the lesser of two evils when they say yes to cancer treatment.
We are there in the shadows to help them also say yes to potential cardioprotective measures. Pharmacologics, lifestyle modification and selective methods of delivery of cancer therapies can all make a difference.
As cardio-oncologists, we walk alongside our patients in their incredible journey of cancer survivorship.
When we think of our patients, we want them to have healthier hearts. We reach into our toolboxes to rummage around and creatively put tools together to come up with new solutions.

In short, we innovate.
In fact, the entire field of cardio-oncology is about innovation. Someone had to take a look at the trends in cardiovascular toxicities and say, "Something needs to be done." And why shouldn't we be the ones to do it?
We are currently in the prime of our lives in the field of cardio-oncology. Boldly bringing two fields together to learn from each other and build something new. As our colleagues in oncology develop new drugs at a rapid pace, we develop new understandings of the consequent cardiovascular toxicities also at a rapid pace.
Not only do we seek to understand the cardiovascular toxicities, we also aspire to prevent and optimally treat them. Several studies in cardio-oncology have determined signals suggesting clinical utility of angiotensin converting enzyme inhibitors or angiotensin receptor blockers, as well as beta blockers and statins (and dexrazoxane) for preventing and treating cardiovascular toxicities.
These are tools that we reach in and take out of our cardiology toolbox. We repurpose each tool to achieve something else, something new.
We can take things a step further; we can develop new technologies and new ways of using technology we already have. New technologies such as genomics, transcriptomics, proteomics, microRNAomics, epigenomics, phenomics, populomics, environmentomics, radiomics and so on can all help us examine signals from patients' and populations' entire complement of genes, gene expression profiles, proteins, microRNAs, DNA methylation, phenotypic expression, socioeconomic characteristics, zip codes and more.
The days of "one size fits all" for prevention and treatment in cardio-oncology will soon be behind us and replaced by precision cardio-oncology, a paradigm in which we are truly able to reach into the toolbox and select the right combination of items to provide the right treatment for the right patient at the right time.

We all have unique journeys. If we think back over the years, we can identify times in which we pursued various kinds of training in our undergraduate, graduate, medical or science programs.
We did not always know how we would use that knowledge later, but we knew the knowledge and skills were worth obtaining. That is what we love about the innovative spirit. The things we have learned and experienced in the past gives us vision and insight into what we can design for the future.
When we look at electrocardiography, echocardiography, computed tomography, magnetic resonance imaging and positron emission tomography, we see a variety of modes of imaging what's inside our patients. All tools that were created through innovation. We also see robust opportunity to innovate further.
- What if we could automate more of the function of each tool, so that the tool could be even more useful at the point of care in a small package, likely in less experienced hands, and perhaps in remote communities?
- Could the operator of the tool be assisted by artificial intelligence, while communicating by digital video with a more experienced specialist or consultant in another location?
- Could such advancement in technology help bring more advanced care to patients in rural areas in the U.S. and throughout the world?
Artificial Intelligence (AI) uses computers to perform tasks or produce new insight that models human intelligence. Algorithms are trained on existing data to determine underlying trends and associations in the data that can be used to predict behaviors in new situations or for new patients.
This kind of technology or adaptation of technology is disruptive, groundbreaking and novel.
We could use various types of AI, such as natural language processing and machine learning (which includes deep learning), to extract data from electronic health records and classify patients into clusters, respectively. We can then use this to make better predictions for our patients in cardio-oncology.
We can use algorithms to identify intricacies on the electrocardiogram, echocardiogram, computed tomography, magnetic resonance imaging and positron emission tomography at a microscopic level that may evade human eyes at the macroscopic level, using innovations in AI-driven radiomics.
We can feed such images into the algorithms we create and have the algorithms help us determine who is most at risk for cardiovascular toxicity, so that we can even more aggressively prevent cardiovascular disease in these patients.
We should note that the algorithms are only as good as we make them. The algorithms will reflect our own biases and inaccuracies. Tremendous care must be put into algorithm development, validation and adjudication to ensure that we do the best for our patients and improve disparities in how we care for them, rather than worsen those disparities.
To paraphrase the great Sir William Osler: "The good physician treats the disease; the great physician uses innovation to prevent and treat the disease."

The "Why Innovation" section series is a brief write-up from ACC Health Care Innovation Section members to give readers a background of their professional journey, and explain the significance of innovation to their work and in the field.
Authors can include their personal definition of innovation, as well as tips or tricks on how to bring innovative ideas to the table in otherwise traditional settings and spaces.