Cover Story | Exploring the Impact of Transcatheter Mitral Valve Repair: Real-World Outcomes
Transcatheter edge-to-edge repair (TEER) of the mitral valve is considered an important alternative treatment for degenerative mitral regurgitation (MR). Currently holding an indication from the U.S. Food and Drug Administration (FDA) for only patients with severe degenerative MR at prohibitive and high surgical risk, or for patients with severe secondary MR and persistent heart failure despite medical treatment, TEER has been increasingly utilized in patients with diverse clinical risk and with a wide range of mitral valve anatomies.
Cardiology checked in with two of the top clinician-researchers in this field – one a surgeon, one an interventionalist – to look at the latest developments and real-world outcomes of TEER for patients with degenerative MR, and to better understand the data needed to consider applying TEER in lower-risk populations.
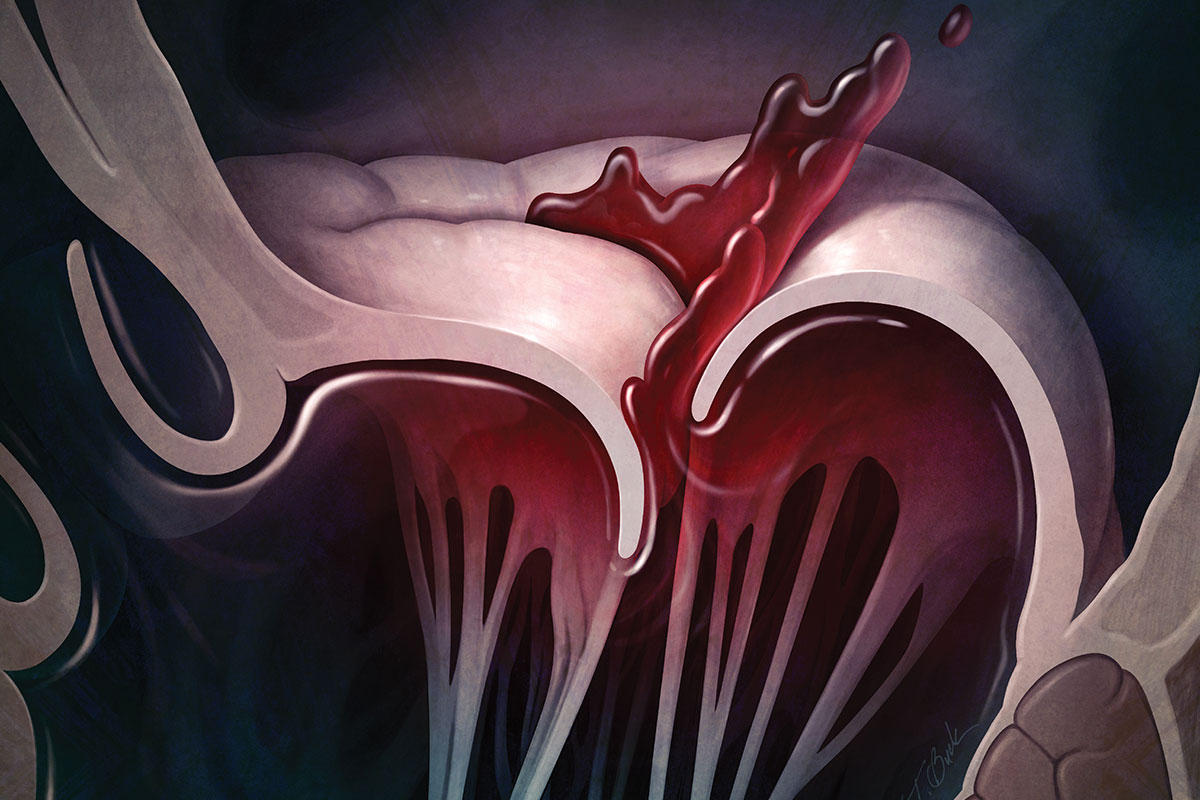
Mitral: Voted the Valve Most Likely to Leak
MR stands out as the most prevalent valvular heart disease, affecting approximately 2% to 3% of the general population. Moderate or severe MR is seen in approximately 10% of individuals over the age of 75.
Primary (or degenerative) MR is any regurgitation resulting from structural deformity of or damage to the leaflets, chordae or papillary muscles preventing the leaflets from closing sufficiently during systole. The most common cause of primary MR in developed countries is mitral valve prolapse related to myxomatous degeneration of the mitral valve.

– Joanna Chikwe, MD, FACC
Patients with chronic degenerative MR often remain asymptomatic until late in the clinical course. Clinical findings can appear benign; symptoms include fatigue, dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea and weight gain.
The onset of symptoms in patients with severe chronic MR is associated with poor outcomes, regardless of left ventricular ejection fraction (LVEF). But even in asymptomatic patients, the presence of significant MR is associated with an increased risk of LV dysfunction, heart failure, pulmonary hypertension, atrial fibrillation, reduced quality of life and death.
Surgical Repair: The Gold Standard

Surgical mitral valve repair is the gold standard for the treatment of degenerative MR, showing excellent survival rates, preservation of LV function, and a reduced risk of thromboembolic events and endocarditis.
Earlier this year, Badhwar, et al., reported on 53,462 surgical procedures performed for primary MR where the intention had been to perform a mitral valve repair.1 The data were taken from the Society of Thoracic Surgeons (STS) database for procedures performed between 2014 and 2020, covering 881 North American hospitals and 2,404 unique surgeons.
This real-world analysis found that overall mortality after mitral valve repair was very low at 1.16%. Mortality was higher in patients for whom the intent had been to repair the valve but who went on to have a mitral valve replacement (3.18% vs. 1.02% for planned repair). The mortality risk was <0.5% in patients <65 years of age. Stroke and permanent pacemaker rates were similarly low (1.2% and 3.7%, respectively).
Patient Tools For Managing MR
Patients are a key partner in managing their MR. CardioSmart infographics and worksheets support this partnership and shared decision-making. Click here to download these free tools to share with your patients.
The analysis included high- and low-volume surgeons. Median operations per surgeon was eight cases over six years, ranging from one to 1,077. While 81% of surgeons had no documented operative deaths through the study period, lower mortality (0.56%) and lower conversion to replacement rates (2.07%) were observed in centers doing ≥50 procedures per year (3% of centers).
The researchers suggested that the hospital volume associated with operative mortality of ≤1% may be estimated at 25 cases.
"Surgical mitral valve repair is a very good operation that restores appropriately referred patients with degenerative MR to normal life expectancy and one in which, in experienced hands, we can consistently offer patients a mortality risk of less than 1% if not less than 0.5%," says Joanna Chikwe, MD, FACC, chair of the Department of Cardiac Surgery in the Smidt Heart Institute at Cedars-Sinai in Los Angeles. "This is a very high bar for any alternative to beat."
The Transcatheter Alternative
Despite its safety and efficacy, however, surgery is still surgery and a considerable proportion of older patients with severe MR are left undertreated due to the associated risks of surgical complications. TEER offers a solution for this high-risk degenerative MR patient population.
Edge-to-edge mitral valve leaflet repair with the MitraClip (Abbott), which obtained CE marking in Europe in 2008 and approval for commercial use by the FDA in 2013, has significantly impacted the treatment of degenerative MR, especially in older patients.
The initial FDA approval was based on small-scale studies involving carefully selected patients with favorable mitral valve anatomy for transcatheter repair. However, real-world application has witnessed a widening scope, with diverse patient populations and varying mitral valve anatomies benefiting from this innovative therapy.
To gain deeper insights into the contemporary outcomes of TEER, Makkar, et al., published a comprehensive analysis of real-world data from the STS/ACC Transcatheter Valve Therapies (TVT) Registry to evaluate the trends and outcomes associated with TEER for degenerative MR that extend beyond current indications.2
Of 60,883 TEER procedures performed with the MitraClip system in the U.S. from January 2014 to June 2022, 19,088 patients were included in this analysis. From these, 10.1% were categorized as low surgical risk for mitral valve repair, 68.0% were at intermediate risk, and 21.9% were deemed at high risk.
– Martin B. Leon, MD, FACC
Median age was 82 years, 48% were women and median STS predicted risk of mortality with surgical repair was 4.6%.
In 88.9% of patients, MR success (defined as moderate or less residual MR and a mean mitral gradient of <10 mm Hg) was achieved. At 30 days, 2.7% of patients had died, 1.2% had a stroke, and 0.97% required mitral valve reintervention.
TEER success compared with an unsuccessful procedure was associated with significantly lower mortality (14.0% vs. 26.7%; adjusted hazard ratio, 0.49; 95% CI, 0.42-0.56; p<0.001) and heart failure readmission (8.4% vs. 16.9%; adjusted hazard ratio, 0.47; 95% CI, 0.41-0.54; p<0.001) at one year.
The best one-year survival was noted in patients who had both mild or less residual MR and mean mitral gradients of ≤5 mm Hg (11.4%).
The biggest downside to TEER is that, should surgical reintervention be necessary due to excessive residual or recurrent MR, subsequent surgical repair of the mitral valve is often not possible, and surgical valve replacement may be the necessary alternative.
"If your patient's TEER fails and they now have moderate or severe residual or recurrent MR, they now have a less than 5% chance of having a surgical repair and a 95% chance of needing that valve replaced," explains Chikwe.
Find Your Community!
ACC's Member Sections are important communities within your professional home. Click here to learn more about all the Sections, including the Cardiac Surgery Team Section and Interventional Section. Join today and help drive your field forward.
"This is a much worse option than a surgical repair to rectify the issue or if they'd had a surgical mitral valve repair in the first place."
In a 2021 JACC article, Chikwe provided some early insights into the surgical outcomes in patients in whom TEER failed.3 In a cohort of 463 patients, the surgical repair rate after failed TEER was only 4.8% overall (6.8% in the cohort of patients with degenerative disease).
Of note, in the study cohort, median age was 76 years, the median LVEF was 57% and 86.1% had heart failure symptoms. The median STS-predicted mortality was 7.7%.
In the cohort undergoing isolated mitral surgery, median STS-predicted mortality was 6.5% and observed mortality was 10.2%. And here again, experience matters: In the four centers that performed ≥10 procedures, mortality was 2.6%, jumping to 12.4% in centers performing fewer cases.
Although no randomized trials have directly compared repair and replacement, clinical experience indicates that patients who undergo replacement face higher short-term morbidity and mortality. "This may be due to the fact that these patients are often sicker, introducing a selection bias," notes Chikwe, "Replacement patients are also more likely to require anticoagulation, are at an increased risk of stroke, and have greater longer-term risk for future valve failures and repeat surgeries."
MitraClip: Fourth Generation
The original MitraClip was first implanted 20 years ago and now has been used in ≥150,000 patients worldwide. Over time, iteration has been a key factor driving improved outcomes and expanded adoption.
"There recently have been some important improvements in the technology for transcatheter repair – improvements in imaging, in the devices themselves and the variety of devices we have to suit specific anatomies, and in the experience of the operators," says Martin B. Leon, MD, FACC, chief innovation officer for the Division of Cardiology at Columbia University Irving Medical Center in New York.
The latest iteration of the MitraClip, dubbed the MitraClip G4, sports several notable improvements over its predecessor – two wider clip sizes (NTW and XTW, 6 vs. 4 mm width) and improved arm designs to reduce leaflet stress during clip deployment.
"The G4 also offers an independent leaflet grasping feature, so instead of having to grab both leaflets at the same time, now you can do one at a time. This tends to yield better results in some patients," says Leon, who is the founder of both the Cardiovascular Research Foundation and the Transcatheter Cardiovascular Therapies (TCT) meeting.
– Martin B. Leon, MD, FACC
EXPAND G4 is a postmarketing, prospective, multicenter, single-arm registry that enrolled 1,141 individuals with primary and secondary MR treated with the MitraClip G4 system at 60 centers in 10 countries between March 2021 and February 2022.
Importantly, there were no prespecified clinical or anatomical exclusion criteria. Study participants had either primary or secondary MR and were scheduled to receive the MitraClip per the current approved indications for use.
In 30-day outcomes published in June 2023, implantation and acute procedural success rates were 98.0% and 96.2%, respectively, with a mean of 1.4 clips implanted per patient.4 MR was significantly reduced at 30 days compared with baseline: 98% of patients achieved MR ≤2+ and 91% achieved MR ≤1+ (p<0.0001). The composite major adverse event rate was 2.7% and the all-cause death rate was 1.3% at 30 days.
The closest competitor to the MitraClip is the PASCAL system from Edwards Lifesciences, which received FDA approval in September 2022 for treatment of degenerative MR.
The CLASP IID randomized trial, which compared the MitraClip to the PASCAL device in primary MR, showed PASCAL to be noninferior to MitraClip for major adverse events and MR reduction among patients with degenerative MR and prohibitive surgical risk.5 The ongoing CLASP IIF trial is comparing the PASCAL device with MitraClip in patients with functional MR.
Heart Team For the Win

As per current ACC/AHA guidelines, all patients being considered for a valve intervention should be evaluated by a multidisciplinary heart valve team.6
"The valve clinic is a good place to screen almost anyone with valvular heart disease that is significant enough to justify advanced therapies of any kind," says Leon.
For the symptomatic prohibitive or high-risk patient with severe MR, TEER is clearly the appropriate treatment. "This is probably an elderly patient, over 80 years of age, with comorbidities, renal dysfunction and the like, or maybe they've had a previous repair that has failed and we know we're going to have to work very hard to give them a perfect outcome from surgery," says Chikwe.
"Conversely, the patient who should absolutely go to surgery at the moment, outside of the confines of a randomized trial, are the patients who have a less than 1% operative mortality after surgical repair and for whom we have a 99% chance of giving them a good repair and a good outcome," she adds, which, in practice, is probably a patient under the age of 75 without significant comorbidity.
It's the middle group, for whom both the surgical and the transcatheter options are good ones, where things get tricky.
"For the most part, patients currently undergoing TEER are in the higher risk categories. But risk is in the eye of the beholder. So, you might see an 80-year-old woman who is frail and has other comorbidities, and who falls into an intermediate risk category, but she doesn't want to undergo a thoracotomy and is sent for TEER," says Leon.
Part of this equation, Leon and Chikwe both stress, should be a consideration of operator and institutional volume. "If you have a borderline patient and you've got a very good TEER operator and the anatomy is suitable, then TEER becomes a more reasonable choice," says Chikwe.
"For those in the gray area, it absolutely relies on us having an ethical approach and wanting to do the right thing by the patient, keeping in mind that we are both driven by bias," says Chikwe.
PRIMARY: An NIH-Funded Landmark Comparison
Clinician Tools
ACC's ManageMR Toolkit guides clinicians from assessment to referral of a patient with MR. Click here to learn more and download an echo checklist, referral checklist and referral algorithm.
Click here to download the ManageMR mobile app.
The wait will be a substantial one but the PRIMARY trial promises to be a landmark clinical trial that will either establish TEER as a treatment for the wider world of primary MR or reestablish the gold standard status of surgical repair.
"The only randomized data we have comparing TEER vs. surgical therapy is from the EVEREST II trial, which is now 15 years old, using the original MitraClip device and involving much less experienced operators," says Leon. "At the present time, most structural interventionalists still believe that TEER should be largely confined to older patients who are not good surgical candidates."
"But with improved devices, shorter procedures and better imaging, as well as operators who have greater experience performing the procedures, there could be an opportunity for more patients with primary MR to be candidates for TEER. But we do not have data to support that yet, which is why we're doing these studies."
The Percutaneous or Surgical Mitral Valve Repair (PRIMARY) trial, funded by the National Heart, Lung, and Blood Institute (NHLBI), and designed and conducted by the Cardiothoracic Surgical Trials Network, is a prospective, international, multicenter, open-label, randomized trial comparing mitral valve TEER to surgical repair in patients with primary, degenerative MR.
Leon and Chikwe along with Patrick T. O'Gara, MD, MACC, from Brigham and Women's Hospital in Boston, MA, are the PRIMARY trial study directors.
The trial, which is nearly 20% through recruitment and which probably won't reveal results before 2027, is being conducted at 60 sites across the U.S., Canada, Germany and the U.K., and allows use of all devices legally marketed for TEER of primary degenerative MR in a particular country.
Importantly, although commercial TEER devices are currently only approved in the U.S. for high and prohibitive risk patients, participants at low or moderate risk for surgery will also be eligible.
"We are recruiting patients with severe, primary MR across all risk categories, as long as they are over 60 years, and either intervention is deemed appropriate and feasible, and we can expect them to have good outcomes with either TEER or surgery," says Chikwe. "We expect this will provide a robust evidence base to inform this key decision for these patients."
The trial will examine long-term effectiveness and safety of TEER and surgical repair, looking at a primary outcome of composite all-cause mortality, valve reintervention, hospitalizations and urgent visits for heart failure, or onset of ≥2+ MR (by transthoracic echocardiogram) at three years post randomization.
"There may be more residual MR with TEER than surgical repair, but we're not certain that the small increment in residual MR after TEER will impact clinical events or quality of life metrics. That's one of the questions this trial will answer," says Leon.
MITRA HR and REPAIR MR are two other ongoing trials comparing surgery to percutaneous mitral valve repair. The first is enrolling high-risk patients eligible for either surgery or TEER, and the second, patients older than 75 and at intermediate surgical risk.
"REPAIR MR is looking at the intermediate-risk patients, where we can't consistently deliver less than 1% or 0.5% operative mortality with surgical repair, so there is a degree of clinical equipoise here. Abbott has funded a noninferiority, two-year randomized trial to look at that," says Chikwe.
Eligible patients are those with a 2% estimated STS surgical risk, "which is only about 15% of intermediate-risk patients who are treated with surgery, so while this trial is important, it's not going to inform practice for the vast majority of patients where we need to know if TEER is an appropriate option," she notes.
Leon adds, "Over the next few years, these trials will provide new insights as to whether or not we can extend the use of mitral valve repair using transcatheter techniques and provide equivalent outcomes to what our surgeons have been doing very well with surgical repair."
Matching the Procedure to the Patient
"Experience matters both for surgery and TEER and, unfortunately, it's not easy for patients or referring physicians to know which operators are most likely to provide excellent outcomes," says Chikwe. Particularly important for surgical patients is to avoid an unnecessary mitral valve replacement.
"The likelihood that you'll get a repair over a replacement for degenerative MR goes from 100% at some centers to about 40% at others, and this is largely based on individual surgeon and hospital volumes, despite the clear evidence that repair is superior to replacement," explains Chikwe. "If a patient goes to a surgeon who does more than 25 mitral valve procedures each year, so about once every two weeks, they're more likely to get their mitral valve fixed. If the surgeon and the hospital are less experienced, they'll likely get a replacement," she adds.
In propensity-matched patients who underwent mitral valve repair vs. replacement, four-year mortality was 3.5% compared with 12.1% (p<0.001).7
"After a successful mitral valve repair, patients can expect to return to their normal daily activities without the need for anticoagulation or further interventions. On the other hand, a valve replacement procedure reduces life expectancy by approximately 10%, causing a decline in the patient's survival curve," notes Chikwe.
To prevent patients better served by a mitral valve repair from ending up with a replacement, a joint project between the Mitral Foundation and the American Heart Association identifies Mitral Valve Repair Reference centers in the U.S. The recognition program combines volume, resource and clinical performance measures to award experienced hospitals and surgeons.
Centers are chosen because they have performed at least 50 index mitral valve repair procedures in the most recent year and have at least one surgeon who has performed a minimum of 25 index mitral valve repair procedures in the most recent year or an average of 25 per year for the most recent two years. The program has now recognized 22 qualified centers.
ACC's Transcatheter Valve Certification program also can help identify appropriate referral centers. This certification program requires the engagement of a multidisciplinary care team and employs a shared decision-making model and patient-centered approach. It provides a blueprint to establish internal infrastructures to meet regulatory standards for launching and maintaining a successful mitral valve surgical and TEER program. Participants in this program must utilize data and metrics collected from both the STS/ACC TVT Registry and surgical registries to optimize appropriate patient selection, positive clinical outcomes and improve patient satisfaction. Click here to connect your patients with the right hospital.
To learn more about ACC's Transcatheter Valve Certification program, Click here.
This article was authored by Debra L. Beck, MSc.
References
- Badhwar V, Chikwe J, Gillinov AM, et al. Risk of surgical mitral valve repair for primary mitral regurgitation. J Am Coll Cardiol 2023;81:636-48.
- Makkar RR, Chikwe J, Chakravarty T, et al. Transcatheter mitral valve repair for degenerative mitral regurgitation. JAMA 2023;329:1778-88.
- Chikwe J, O 'Gara P, Fremes S, et al. Mitral surgery after transcatheter edge-to-edge repair. J Am Coll Cardiol 2021;78:1-9.
- von Bardeleben RS, Rogers JH, Mahoney P, et al. Real-world outcomes of fourth-generation mitral transcatheter repair: 30-day results from EXPAND G4. JACC Cardiovasc Interv 2023;16:1463-73.
- Lim DS, Smith RL, Gillam LD, et al. Randomized comparison of transcatheter edge-to-edge repair for degenerative mitral regurgitation in prohibitive surgical risk patients. JACC Cardiovasc Interv 2022;15:2523-36.
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021;77:e25-e197.
- Hannan EL, Samadashvili Z, Smith CR, et al. Mitral valve repair versus replacement for patients with preserved left ventricular function without heart failure symptoms. J Thorac Cardiovasc Surg 2019;157:1432-39.e2.
Clinical Topics: Valvular Heart Disease, Mitral Regurgitation
Keywords: ACC Publications, Cardiology Magazine, Mitral Valve Insufficiency, Stroke Volume, Ventricular Function, Left, Mitral Valve Prolapse, Endocarditis, Pacemaker, Artificial
< Back to Listings