Cover Story | Transformation and Evolution: The Clinical Guideline Journey
Forty years after the first clinical practice guideline on cardiac pacemakers, the ACC and the American Heart Association (AHA) continue to evolve the guideline process – and the documents themselves – to ensure clinicians are able to optimize the care and outcomes of patients with cardiovascular disease.
Adapting to the constantly changing health care environment, increasingly rapid pace of new research, and seemingly endless evolution of new technologies hasn't been an easy journey, but the commitment by both societies to creating and publishing the latest clinical guidance based on the best available evidence hasn't waned.
"Remember that the first guideline was developed in response to what was felt to be an overutilization of pacemakers," says Richard J. Kovacs, MD, MACC, ACC's Chief Medical Officer. "That was proven not to be true, but the negative connotation of a guideline to prevent certain kinds of care pivoted to the very positive role of the guidelines in saying what we should do to care for our patients."
Over the last four decades, ACC and AHA leaders and staff have regularly taken steps to evaluate processes and to adapt and evolve to meet the needs of clinicians and patients alike, all while developing and distributing dozens of guidelines ranging from aortic disease to valvular heart disease.
A Decade of Change
In a 2014 overview of "The Evolution and Future of ACC/AHA Clinical Practice Guidelines" published in JACC, guideline leaders highlighted several changes to the guideline development process over the previous three decades, including the addition of a separate process for conducting systematic reviews of research, the use of critical questions to focus the evidence review process, the addition of a lay representative on writing committees, the expansion of the peer review process, and an accelerated public release of the manuscripts.
Fast forward to 2019, and a report from the ACC/AHA Task Force on Clinical Practice Guidelines highlighted additional innovations and improvements. Among them, a focus on recommendations and figures versus lengthy text and background information, as well as early efforts to provide guideline information in modules, in a manner that has facilitated easier implementation at the point of care.
– Richard J. Kovacs, MD, MACC
"Physicians and all health care providers face increasing demands on their time …," said report authors Glenn N. Levine, MD, FACC, Patrick T. O'Gara, MD, MACC, and Joshua A. Beckman, MD, MS, et al. "These requirements and activities in aggregate often leave little time for reading lengthy guidelines. Thus, there is an increasing need to format guidelines and deliver practice-relevant information and guidance in actually readable, searchable and electronically accessible formats."
Another major change outlined in the 2019 report was the transition from a procedure-centric to condition-centric focus. Where early clinical practice guidelines addressed procedures such as pacemakers and defibrillators, newer guidelines were focused on conditions like atrial fibrillation, chest pain, valvular heart disease, etc.
What Does Optimization Look Like?

Since then, a comprehensive five-year "Guideline Optimization" effort undertaken by the ACC and AHA has resulted in even further progress and transformation.
"Not readily apparent to the average reader, each new Guideline since 2019 is written in a modular format, with recommendations followed by brief supportive text," says Kovacs. "This makes it easy to replace a section of the guideline with new findings that could change a category of recommendation or a level of evidence without having to re-write the guideline."
A second important change, according to Kovacs, involves rapid updates of the Guidelines when new information becomes available. "We are piloting annual updates of our newest guidelines, by surveying the medical literature as well as new drug and device development every year," he says. "If the data suggest a need to update a section, we can do so easily because of the modular format."
The "What is New" table that debuted in the recent 2024 Hypertrophic Cardiomyopathy (HCM) Guideline provides a glimpse into additional benefits of the modular format (Figure 1). Because both the 2020 and 2024 HCM guidelines were in modular format, guideline authors were able to compare and show new and revised recommendations in a table format that allowed readers to easily see specific areas of change.
– Richard J. Kovacs, MD, MACC
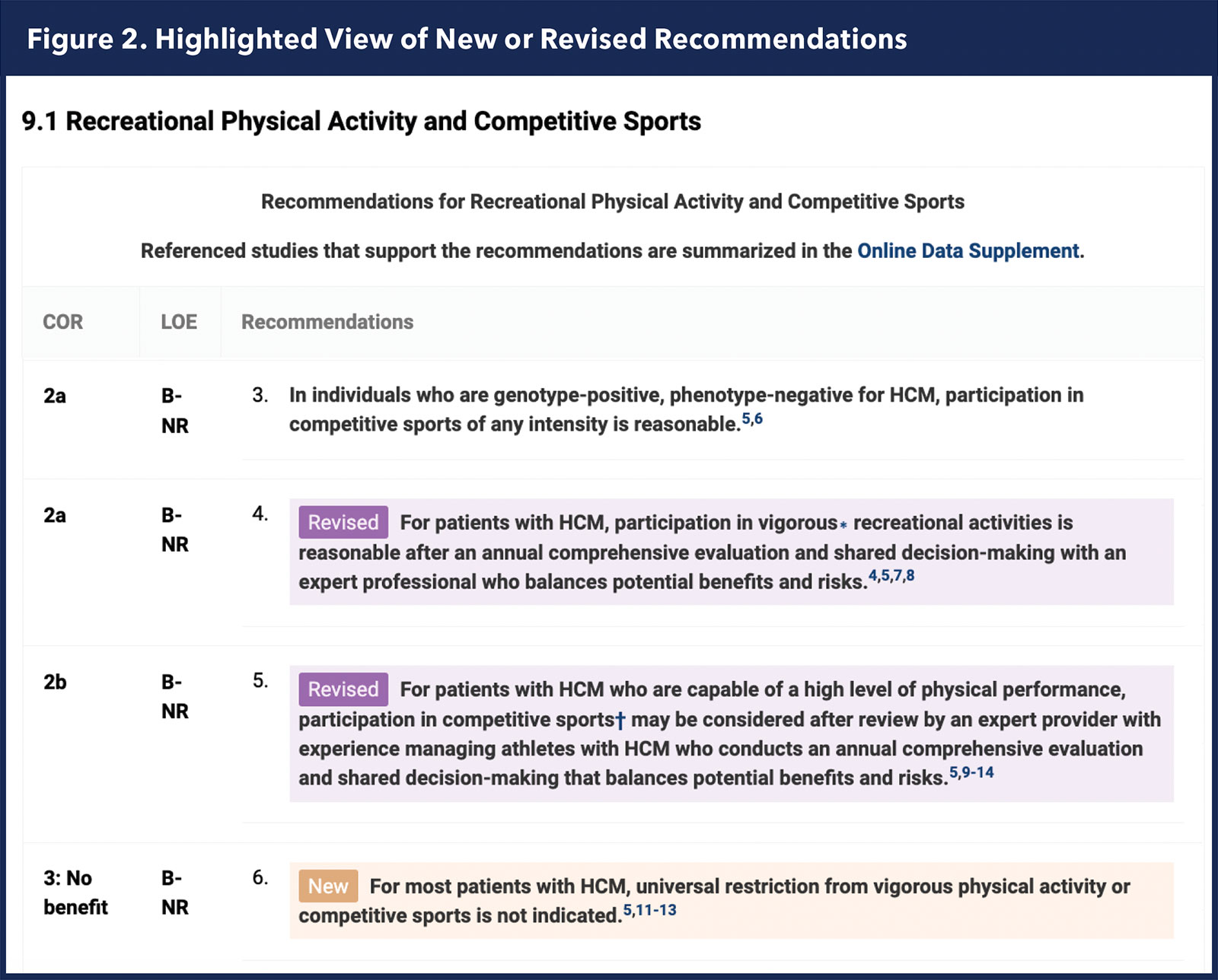
Also making its debut with the HCM guideline is the "Highlighted View" enhanced reading mode, available only in the online view on JACC.org, that highlights new or revised text throughout the guideline for fast, easy identification of changes (Figure 2).
In another major accomplishment, the Joint Committee on Clinical Practice Guidelines adopted a uniform outline for all disease-focused guidelines. "This is great news for future guidelines," says Kovacs, "as it further standardizes the development and format of guidelines going forward."
Continuing the Journey
The ACC has published the following four guidelines since 2023:

2024
- Lower Extremity Peripheral Artery Disease
- Hypertrophic Cardiomyopathy
2023
- Atrial Fibrillation
- Chronic Coronary Disease
Watch for the new Guideline for Perioperative Cardiovascular Management for Noncardiac Surgery coming soon.

Click here to download the ACC Clinical Guideline app.
Meanwhile, the guideline metamorphosis only continues.
According to Kovacs, the ACC and AHA, as part of the Guideline Optimization efforts, recently reaffirmed that guideline development is the most important thing the two organizations do together.
"The AHA brings a huge public presence and the ACC is the professional home for the cardiovascular clinician," he says. "Together we cover all the bases from basic science to bedside care. Not to mention, the two organizations together are a powerful and trusted voice for establishing standards of care."
Most recently, a survey of roughly 100 clinicians during ACC.24 in Atlanta, found that most would like to see a more unified style and formatting, along with more labels and legends. Staff and committee members are taking this feedback to heart and looking at new ways to further improve and enhance figures and tables to facilitate ease of use.
For example, algorithmic figures that incorporate guideline recommendations, as well as the class of recommendation rating system, will be improved to provide more clarity and consistency, resulting in visuals that support screening, risk stratification and diagnosis, as well as management.
The use of new technologies, including workflow and content management systems and artificial intelligence, also hold potential for helping to standardize and streamline processes even further.
"More efficient tracking and development ideally will allow us to work on guidelines simultaneously, publish more frequent updates, and ultimately more closely match the pace of the evolving evidence," says Kovacs.
"The greatest accomplishment over the last 40 years has been our ability to build and sustain trust in the guidelines," he says. "Continuing to maintain this trust is vital to ensuring clinicians are confident in their ability to care for their patients."
From Policy to Practice: Disseminating the Latest Guidelines
ACC guideline dissemination is an organization-wide effort overseen by the Solution Set Oversight Committee (SSOC) to ensure the integration of guideline content throughout ACC's clinical policy, education, registry, membership and advocacy efforts.
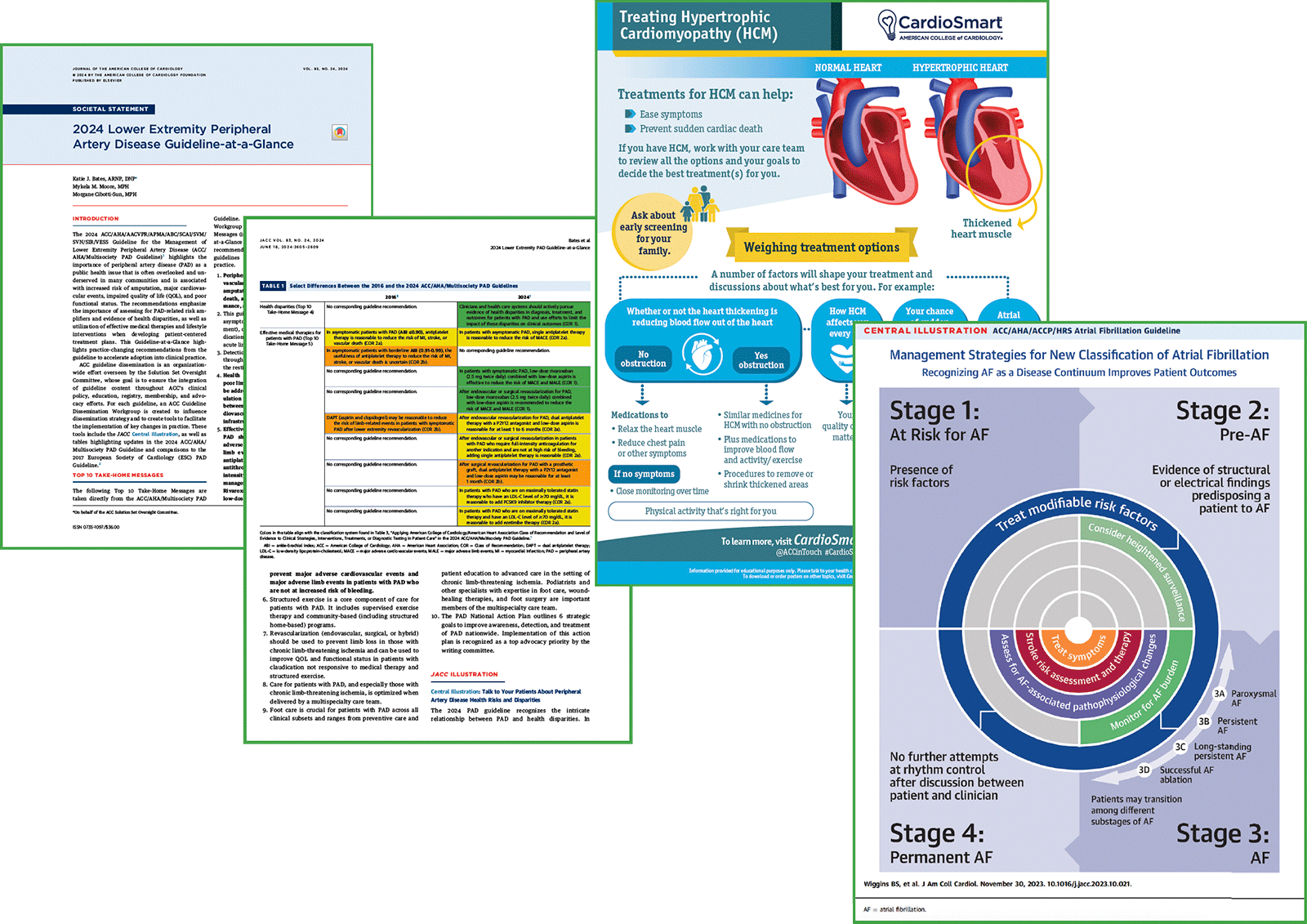
For each guideline, an individual ACC Guideline Dissemination Workgroup is created to influence the dissemination strategy and to create tools to facilitate the implementation of key changes in practice. These tools include the newer Guideline-at-a-Glance resource, which replaced the "Executive Summary" starting with the Aortic Disease Guideline in 2022.
– Megan Coylewright, MD, FACC
"The Guideline-at-a-Glance document includes the top take-home messages from the guideline, a central illustration that encapsulates some of the most important concepts, and tables comparing the current guideline to the previous ACC/AHA guideline and/or to the most recent ESC guideline as appropriate," says Nicole Bhave, MD, FACC, chair of the SSOC.
Interactive tools tied to specific guideline recommendations, as well as CardioSmart patient education ranging from infographics to decision aids and discussion guides, are also important to the dissemination toolbox.
Visit ACC.org/Guidelines to access dedicated hubs for each guideline, which include quick links to the Guideline-at-a-Glance and other SSOC-developed resources, dedicated slide sets, related-JACC resources and interactive tools, CardioSmart patient education, mobile apps and more.
"CardioSmart is ACC's platform for shared decision-making implementation and advocacy for the patient voice," says CardioSmart Editor Megan Coylewright, MD, FACC, who also served as an SSOC representative on the recent HCM Guideline Dissemination Work Group. "The role of CardioSmart continues to expand as formal guidelines focus on the role of shared decision-making. Validated decision aids help support clinicians to respond to, and share with patients, the latest evidence and clinical guidelines."
Looking ahead, Bhave says the SSOC is always seeking new opportunities for cross-College collaboration, both to leverage the wealth of expertise within the organization, and to ensure that content meets members' needs. "As the guideline writing and updating process becomes more dynamic, we will need to adapt our dissemination strategies, utilizing platforms including ACC.org and the DocMatter community to keep our members informed."
Meanwhile, Coylewright says she hopes that CardioSmart's validated decision aids will become more integrated into all cardiology clinics to signal to patients the ACC's key value of patient engagement and shared decision-making, and support clinicians in these conversations.
Clinical Topics: Valvular Heart Disease, Vascular Medicine
Keywords: Cardiology Magazine, ACC Publications, Pacemaker, Artificial, Heart Valve Diseases, Aortic Diseases, Delivery of Health Care, Health Policy

