New in Clinical Guidance | ACC/AHA ACS Guideline, More
New Acute Coronary Syndromes Guideline From ACC, AHA
A new clinical guideline released by the ACC and the American Heart Association (AHA) includes new evidence and updated recommendations for managing patients with an acute coronary syndrome (ACS). The 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients With Acute Coronary Syndromes was published in JACC.
The guideline primarily focuses on the management of type 1 acute myocardial infarction – both NSTEMI and STEMI – and includes recommendations addressing initial evaluation and management of suspected ACS, standard medical therapies, reperfusion strategies, catheterization lab considerations, cardiogenic shock management, long-term management and secondary prevention, and more.
Among the highlights are updated recommendations for pharmacologic care. Dual antiplatelet therapy (DAPT) with aspirin and an oral P2Y12 inhibitor is indicated for at least 12 months as the default strategy in patients with ACS who are not at high bleeding risk, while several strategies are recommended for patients with a higher bleeding risk.
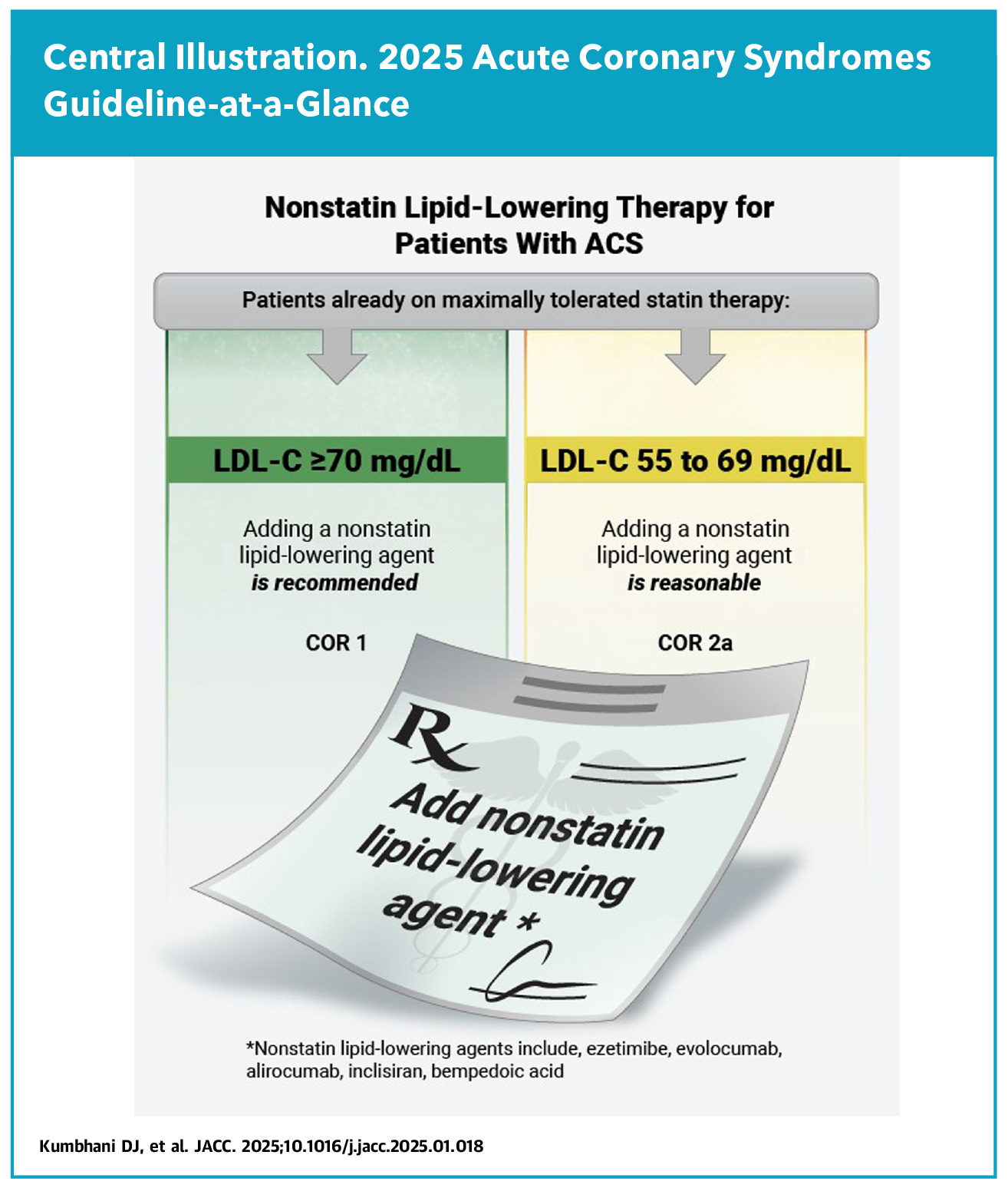
Additionally, high-intensity statin therapy is recommended for all patients with ACS. For those already on maximally tolerated statins and who have an LDL-C level ≥70 mg/dL, a nonstatin lipid-lowering agent such as ezetimibe, evolocumab, alirocumab, inclisiran or bempedoic acid is also recommended.
On the procedural front, the guideline stresses the importance of the radial approach over a femoral approach for PCI in patients with ACS to reduce the risk of bleeding, vascular complications and death. Reflecting the latest evidence, intravascular imaging to guide the PCI procedure is now a class 1 recommendation. In addition, the guideline recommends a strategy of complete revascularization in patients with STEMI or NSTE-ACS, with the choice of revascularization method based on the complexity of the coronary artery disease and comorbid conditions.
Important recommendations for treating cardiogenic shock, including prompt revascularization, are also included in the guideline. Based on new clinical trial data, use of the microaxial flow pump is recommended for select patients with cardiogenic shock related to acute MI. However, the guideline notes that "careful attention to vascular access and weaning of support is important to appropriately balance the benefits and risks."
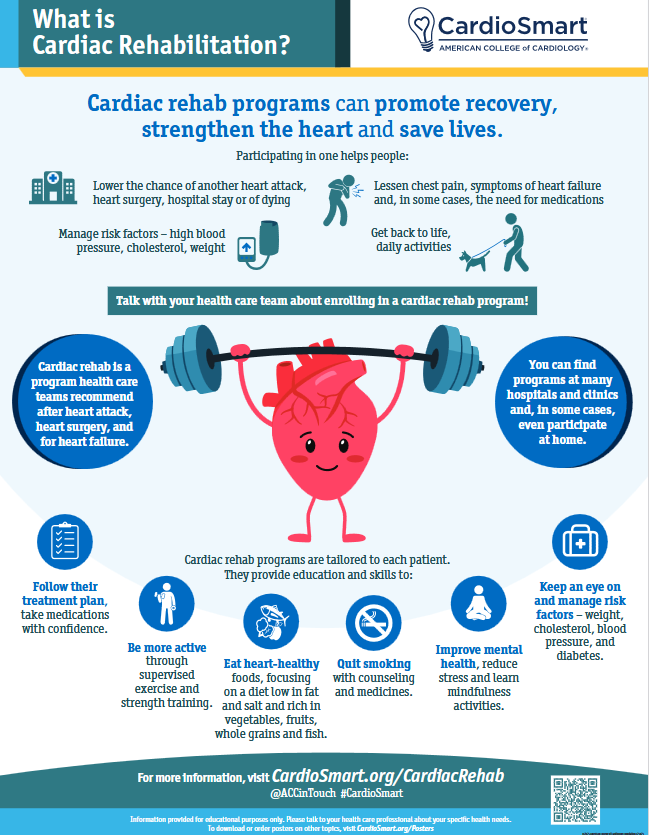
Secondary prevention following discharge is another important focus of the guideline, with recommendations ranging from referrals to outpatient cardiac rehabilitation (or home-based care if outpatient is not doable) to conducting a fasting lipid panel four to eight weeks after initiating or adjusting the dose of lipid-lowering therapy.
"Patients with ACS are at the highest risk for cardiovascular complications both acutely and chronically, which emphasizes the importance of staying up-to-date on the most recent evidence presented in this guideline," says Sunil V. Rao, MD, FACC, FSCAI, professor of medicine, the Leon H. Charney Division of Cardiology, director of Interventional Cardiology at NYU Langone Health and chair of the guideline writing committee. "With appropriate management, we can improve outcomes both in the hospital and over the long term."
In addition to the ACC and AHA, the guideline was written in collaboration with and endorsed by the American College of Emergency Physicians, the National Association of EMS Physicians, and the Society for Cardiovascular Angiography and Interventions.
Cardiac Rehab in a Nutshell
Download this CardioSmart infographic, created to support the new ACS guideline, and help patients understand the benefits of cardiac rehab.

Scientific Statement Addresses Competitive Sports Participation For Athletes With CV Abnormalities
A new joint Scientific Statement from the American Heart Association (AHA) and ACC provides new and updated clinical guidance on how to assess risk when considering competitive sports participation for people with various cardiovascular conditions.
Divided into 11 sections, the statement replaces a previous statement from 2014, and addresses sports classifications; the preparticipation cardiac evaluation; ethical aspects of competitive sports eligibility; cardiomyopathies; myocarditis/pericarditis, valvular heart disease and other acquired cardiovascular conditions; congenital heart disease; aortopathy and spontaneous coronary artery dissection; arrhythmias, devices and ECG abnormalities; cardiac channelopathies; masters athletes; and additional cardiac conditions and considerations (i.e., hypertension, performance-enhancing drugs, pregnancy, etc.).
Of note, the statement authors, led by Chair Jonathan H. Kim, MD, MSC, FACC, and Vice Chairs Aaron L. Baggish, MD, FACC, and Benjamin D. Levine, MD, FACC, highlight new evidence indicating that athletes of all ages who have certain cardiovascular abnormalities or diseases may often safely participate in competitive sports. It also specifically addresses athlete types, like masters athletes, extreme sports athletes and pregnant athletes, not included in previous documents.
Additionally, the statement offers increased guidance for clinicians around risks associated with specific types of sports. For example, certain activities with a higher risk of trauma and bleeding, such as tackle football, competitive cycling, outdoor skiing or baseball, must be considered for athletes taking blood-thinning medications. "We acknowledge that there are times when the risks of competing are much higher than the benefits for athletes with cardiovascular abnormalities," Kim said.
Shared decision-making is also front-and-center in the new Statement. "In the past, there was no shared decision-making about sports eligibility for athletes with heart disease. These athletes were automatically prohibited from participating in sports if almost any cardiac issue was present," said Kim. "This new scientific statement reviews best clinical practices for athletes with certain cardiovascular conditions and how health care professionals can guide these athletes – from children to masters athletes – in a shared decision-making discussion about potential risks and rewards."
Looking ahead, the statement emphasizes the need for more research to better understand how competitive sports participation impacts overall health among athletes with cardiovascular abnormalities, as well as the impacts of social disparities on these athletes. "We have to look at social disparities because it is a very reasonable hypothesis to believe that disparities play an important role in terms of health outcomes for athletes as they do for people in the general population," said Kim.
Clinical Topics: Acute Coronary Syndromes, Arrhythmias and Clinical EP, Congenital Heart Disease and Pediatric Cardiology, Invasive Cardiovascular Angiography and Intervention, Sports and Exercise Cardiology, Valvular Heart Disease, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Interventions, Interventions and ACS, Interventions and Structural Heart Disease, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology
Keywords: Cardiology Magazine, ACC Publications, Percutaneous Coronary Intervention, Acute Coronary Syndrome, Myocardial Infarction, Heart Defects, Congenital, Heart Valve Diseases, Arrhythmias, Cardiac, Athletes