Peripheral Matters | Outpatient Management For Acute Pulmonary Embolism: Current Evidence and Approach to Patient Selection

Acute pulmonary embolism (PE) is a frequently encountered diagnosis in both the emergency department (ED) and among hospitalized patients, with increasing incidence throughout the U.S.1
Over the past two decades, the landscape of PE care has drastically evolved due to numerous technological advances including improvements in diagnosis as well as novel oral anticoagulants.
Importantly, there also has been improved understanding as to which patients with a low-risk PE can be selected for management as an outpatient with home anticoagulation as opposed to inpatient hospitalization.2,3
In this review, we highlight the current evidence and guidelines supporting outpatient PE management and discuss the approach for selecting patients who may benefit from this treatment pathway.
Summary of Evidence

To date, several high-quality randomized controlled trials (RCT) have been published evaluating the safety and efficacy of managing patients with low-risk PE in the outpatient setting.4,5
The strongest evidence to date is derived from an international, open-label, noninferiority trial which randomized patients presenting with an acute, symptomatic low-risk PE (determined by the pulmonary embolism severity index [PESI] risk class) to either hospital discharge (within 24 hours following randomization) or inpatient hospitalization (five days of enoxaparin followed by the initiation of oral anticoagulation).4
Following exclusions, a total of 344 patients were enrolled and 171 patients were randomized to receive outpatient management. The primary endpoint of symptomatic, recurrent venous thromboembolism within 90 days was met by only one patient (0.6%) in the outpatient arm vs. 0 patients [0.0%] hospitalized. Among patients managed as outpatients, three (1.8%) had a major bleeding event and one (0.6%) died within 90 days.
The subsequent Low-Risk Pulmonary Embolism (LoPE) study also supported the safety of outpatient management.6 In this single-arm study, a total of 200 patients presenting with an acute PE and a low-risk PESI score were observed in the ED for 12-24 hours and then discharged for home anticoagulation.
The primary composite outcome of all-cause mortality, recurrent symptomatic venous thromboembolism or major bleeding assessed at 90 days following ED discharge occurred in only one patient (0.5%; 95% CI, 0.02-2.36%), which was a major bleeding event.6
Low rates of these complications have also been demonstrated in pooled analyses among larger cohorts. For example, in a meta-analysis including 1,657 patients across 16 different studies, the pooled incidence of recurrent thromboembolism, major bleeding and mortality at three months among outpatients was 1.7% (95% CI, 0.92-3.1%), 0.97% (0.58-1.6%) and 1.90% (0.79-4.6%), respectively.3
Altogether, these studies have demonstrated that outpatient management in low-risk populations is associated with low rates of recurrent thrombosis, major bleeding and mortality.
Approach to Patient Selection
The current society-endorsed recommendations and strength of evidence recommending outpatient care for patients with a low-risk PE are summarized in Table 1.
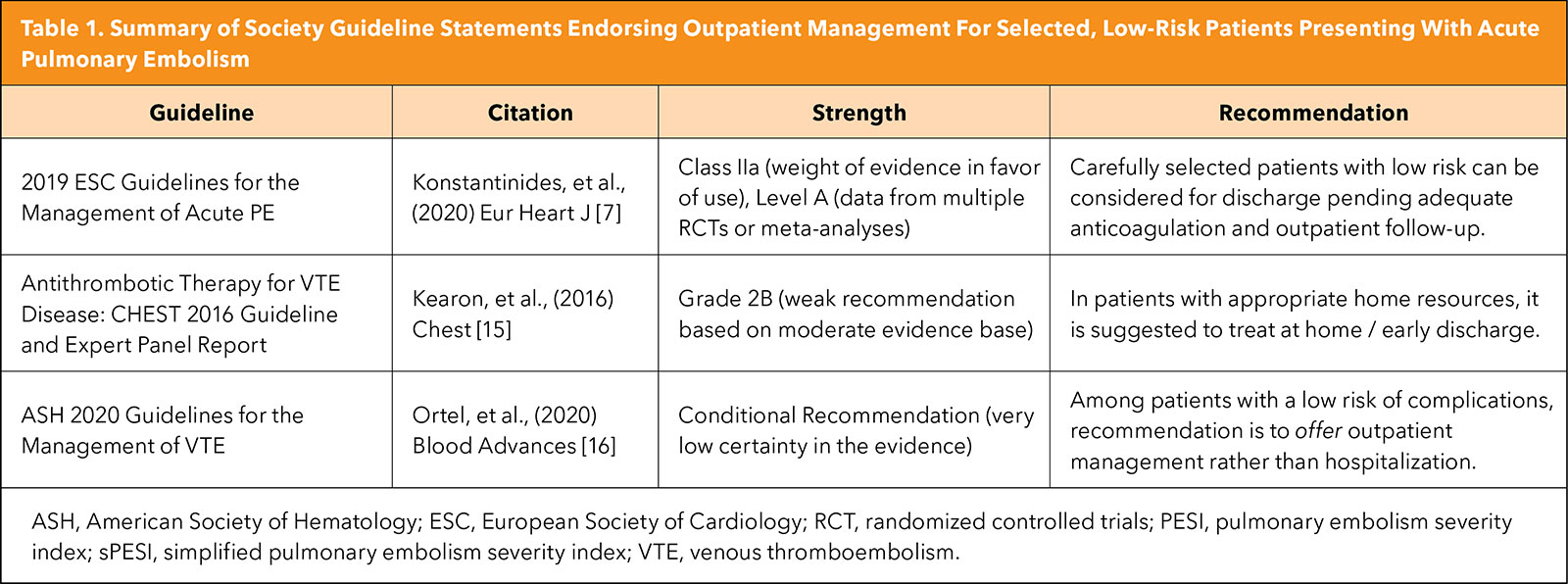
According to the 2019 European Society of Cardiology guidelines, outpatient management of low-risk patients is a Class IIa recommendation and should be considered in the appropriate clinical setting.7
Patients are typically identified based on numerous presenting features including assessment with validated clinical risk stratification scores, and determination of right ventricular function, cardiac biomarkers and hemodynamic status. As such, an ideal patient for outpatient management is one with an estimated low risk of PE-related death, stable hemodynamics and no evidence of right ventricular dysfunction by imaging or cardiac biomarkers.
Several clinical risk stratification scores have been developed and subsequently validated to aid in this assessment. The most well-known and utilized has been the PESI risk class and the simplified PESI score (sPESI). The PESI and sPESI scores incorporate parameters such as age, sex, comorbidities (history of cancer, heart failure or chronic lung disease), and vital sign abnormalities to assess patient risk of mortality at 30 days.8
The PESI score has been shown to have an impressively high sensitivity (91%; 95% CI, 71-97%) and negative predictive value (99%; 95% CI, 96-100%) for predicting overall mortality.9
More recently, the Hestia criteria has been developed to more precisely screen for patients who may be a candidate for outpatient management. As compared to the PESI risk classification, the Hestia criteria uniquely includes variables such as renal and liver function, assessment of bleeding risk and the need for thrombolysis, use of concomitant anticoagulation at presentation, pain scores, pregnancy, history of heparin-induced thrombocytopenia, and other medical or social reasons which necessitate admission.10,11
In external validation studies, the Hestia criteria has been shown to be exceptionally sensitive (100%; 95% CI, 87.7-100%) but offers a low specificity (<27.5%) for predicting 30-day mortality in this population.12
Future Directions
Despite the accumulating evidence derived from RCTs, high-quality prospective studies and meta-analyses supporting the safety of outpatient PE management, recent data have suggested that its utilization in clinical practice remains low.13
For instance, in a recent study which analyzed nationally representative data from the National Hospital Ambulatory Medical Care Survey (NHAMCS), rates of discharge from U.S. EDs remained stagnant between 2012-2020.
Additionally, in this analysis, only one-third of low-risk patients were discharged from the ED, suggesting that outpatient management may still be underutilized and that future efforts directed at implementation are necessary.14
Moving forward, it has become critical to better understand why the utilization of outpatient pathways remains low. While this is likely a multifactorial process, possible implementation challenges include an inability to provide adequate outpatient follow-up to manage anticoagulation, insurance limitations to cover oral anticoagulation, physician discomfort or legal concerns as complications of PE can be severe. Future research investigating solutions to these challenges are necessary.
Conclusion
In summary, outpatient management of acute PE should be considered in selected patients at a low risk of death who can be feasibly managed in the outpatient setting. Future studies focused on solutions to improve the implementation of these pathways are necessary.


This article was authored by Nathan W. Watson, BS, medical student at Harvard Medical School and research fellow at the Smith Center for Outcomes Research in Cardiology at Beth Israel Deaconess Medical Center (BIDMC), and Eric A. Secemsky, MD, RPVI, MSc, FACC, director of Vascular Intervention at BIDMC, section head of Interventional Cardiology and Vascular Research at the Smith Center for Outcomes Research in Cardiology, and associate professor of medicine at Harvard Medical School, all in Boston, MA.
References
- Smith SB, Geske JB, Kathuria P, et al. Analysis of national trends in admissions for pulmonary embolism. Chest 2016;150:35-45.
- Piran S, Le Gal G, Wells PS,et al. Outpatient treatment of symptomatic pulmonary embolism: A systematic review and meta-analysis. Thromb Res 2013;132:515-9.
- Zondag W, Kooiman J, Klok FA, et al. Outpatient versus inpatient treatment in patients with pulmonary embolism: A meta-analysis. Eur Respir J 2013;42:134-44.
- Aujesky D, Roy PM, Verschuren F, et al. Outpatient versus inpatient treatment for patients with acute pulmonary embolism: An international, open-label, randomised, non-inferiority trial. Lancet 2011;378:41-8.
- Otero R, Uresandi F, Jiménez D, et al. Home treatment in pulmonary embolism. Thromb Res 2010;126:e1-5.
- Bledsoe JR, Woller SC, Stevens SM, et al. Management of low-risk pulmonary embolism patients without hospitalization: The low-risk pulmonary embolism prospective management study. Chest 2018;154:249-56.
- Konstantinides SV, Meyer G, Bueno H, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (ERS). Eur Heart J 2020;41:543-603.
- Aujesky D, Obrosky DS, Stone RA,et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med 2005;172:1041-6.
- Donzé J, Le Gal G, Fine MJ, et al. Prospective validation of the pulmonary embolism severity index: A clinical prognostic model for pulmonary embolism. Thromb Haemost 2008;100:943-8.
- Zondag W, Mos ICM, Creemers-Schild D, et al. Outpatient treatment in patients with acute pulmonary embolism: The Hestia Study. J Thromb Haemost 2011;9:1500-7.
- Zondag W, Vingerhoets LMA, Durian MF, et al. Hestia criteria can safely select patients with pulmonary embolism for outpatient treatment irrespective of right ventricular function. J Thromb Haemost 2013;11:686-92.
- Weeda ER, Kohn CG, Peacock WF, et al. External Validation of the hestia criteria for identifying acute pulmonary embolism patients at low risk of early mortality. Clin Appl Thromb 2017;23:769-74.
- Lutsey PL, Walker RF, Maclehose RF, et al. Inpatient versus outpatient acute venous thromboembolism management: Trends and postacute healthcare utilization from 2011 to 2018. J Am Heart Assoc 2021;10:e020428.
- Watson NW, Carroll BJ, Krawisz A, et al. Trends in discharge rates for acute pulmonary embolism in U.S. emergency departments. Ann Intern Med 2024;177: 134-43.
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016;149:315-52.
- Ortel TL, Neumann I, Ageno W, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: Treatment of deep vein thrombosis and pulmonary embolism. Blood Adv 2020;4:4693-738.
Clinical Topics: Anticoagulation Management, Vascular Medicine
Keywords: Cardiology Magazine, ACC Publications, Outpatients, Pulmonary Embolism, Patient Selection, Anticoagulation Management, Enoxaparin